Other Causes Of Liver Disease Top Of Page
It should be recognized that liver disease in patients with HBV-HIV coinfection can be from causes other than HBV, including other viral infections , alcohol, medications, HAART-related hepatotoxicity, and nonalcoholic fatty liver disease . Abnormal liver enzymes in HBV-HIV coinfected patients may be due to any of these factors, as well as the development of drug resistance or reactivation of HBV.
| Table 4. Differential Diagnosis of Liver Abnormalities in Patients with HBV-HIV Coinfection. |
| hbv |
Occult Infection Top Of Page
Occult HBV infection is defined as the presence of HBV DNA in the absence of HBsAg . Often the only serum marker in occult HBV is anti-HBc . The prevalence of occult HBV in HIV-infected populations varies from 10% to 43% depending on the study , whereas the presence of anti-HBc alone is rarely associated with occult infection in HIV-uninfected patients. One study showed ongoing necroinflammatory liver disease with chronic ALT elevations in HIV-infected patients with occult HBV, illustrating that occult HBV represents chronic HBV with active viral replication and should be managed as such .
Hiv And Hepatitis And Participation In Sport
The Equal Opportunity Act 2010 makes it unlawful in Victoria to fail or refuse to select a person with HIV or hepatitis B or C for a sporting team, or to exclude them from participating in a sporting activity, because they have HIV or hepatitis B or C. People with these viruses are not required to disclose their health status to coaches, sporting teams or sporting organisations. They are entitled to keep the fact that they have HIV, hepatitis B or C confidential.
Read Also: Hepatitis C And Liver Cancer
Symptoms And Disease Progression
The majority of adults with hepatitis B have no symptoms, and infection is often only diagnosed by routine blood tests and monitoring the health of the liver. Among people living with HIV, routine liver function monitoring sometimes shows elevated liver enzymes, which can be a sign of liver inflammation due to hepatitis B.
Some people develop symptoms soon after hepatitis B infection, known as the acute phase. These can include the following:
- fatigue
- pain in the upper abdomen or belly
- muscle or joint aches
- feeling generally unwell
- yellowing of the skin and whites of the eyes .
A minority of people may develop severe symptoms during acute hepatitis B infection, and in rare cases it can lead to death.
After the acute stage , many people with chronic hepatitis B have few or no symptoms. Others may experience ongoing symptoms including fatigue and feeling unwell. Even if you have no symptoms, you can still pass on hepatitis B to others.
With or without symptoms, chronic hepatitis B infection can lead to serious liver disease over years or decades, including fibrosis, cirrhosis and liver cancer.
Sharing Injection Drug Equipment
most efficiently . This is because used needles and syringes can still contain blood, which can carry the virus.
HIV is not the only virus that can be transmitted by sharing drug injection equipment. The viruses that cause hepatitis B and hepatitis C can be
- having other types of sexually transmitted infections
Recommended Reading: Does Hepatitis Have A Cure
How Is Hepatitis Diagnosed
Getting tested for hepatitis is important to help detect infection early. Tests may even detect hepatitis before symptoms begin. In people with HIV, this is especially important so that they may receive treatment early. Testing for hepatitis may also reduce transmission to others.
Hepatitis is diagnosed with blood testing. This may involve:
- antibody testing for HAV
- hepatitis B surface antigen, to detect either acute or chronic infections of HBV
- hepatitis C antibody test if antibodies are found in the blood, your doctor may order a follow-up test to confirm HCV
- liver function tests, which may find chronic hepatitis infections
Should People With Hiv Get Tested For Hbv
CDC recommends that all people with HIV get tested for HBV. Testing can detect HBV even when a person has no symptoms of the infection.
There are several HBV blood tests. Results of different tests show different things. For example, a positive hepatitis B surface antigen test result shows that a person has acute or chronic HBV and can spread the virus to others.
Don’t Miss: What Is The Blood Test For Hepatitis C
Symptoms Of Liver Disease
In the early stages of liver disease, there may not be any obvious symptoms. Once there is some damage to the liver, typical symptoms include extreme tiredness, a feeling of general poor health, weight loss, loss of appetite, nausea and vomiting, fever, abdominal pain, itchy skin, and an enlarged or tender liver. Jaundice may also develop. This is easily noticeable as the skin and whites of the eyes turn yellow, urine becomes dark and stools pale.
Flares And Immune Reconstitution Top Of Page
Flares result from changes in the balance between the level of HBV replication and the immune response . Although spontaneous flares and seroconversion occur in HIV-uninfected individuals, this is rarely seen in HIV-infected individuals without HAART . A substantial reduction in HIV viremia and improvement in CD4 cell count after the initiation of HAART, called immune reconstitution, can lead to improved host immune response to HBV and other viral opportunistic infections. In HBV coinfection, immune reconstitution is often manifested by a flare followed by reduction in HBV viremia and less commonly seroconversion. In addition to immune reconstitution, flares of HBV disease in individuals with HIV can occur when anti-HBV therapy is withdrawn, when anti-HBV drug resistance develops , or because of HAART-related hepatotoxicity .
Occasionally, a severe flare associated with immune reconstitution in patients with high-level HBV DNA can cause hepatic decompensation and even death . This experience highlights the importance of screening all HIV-infected patients prior to initiation of HAART, and control of HBV prior to or in conjunction with initiation of HAART . Control of HBV with an anti-HBV drug that has no anti-HIV activity prior to initiation of HAART should be considered in patients with advanced fibrosis and cirrhosis who are at higher risk for hepatic decompensation resulting from a flare.
Also Check: How Do You Get Hepatitis Of The Liver
When Should You Start Treatment For Hepatitis C
With the new antiviral drugs for hepatitis C, it’s now recommended that everyone with hepatitis C shouldn’t wait to be treated, regardless of liver disease severity.
The aim of this treatment is a cure sometimes described as a sustained virologic response. This means that no hepatitis C virus is detectable in your blood six months after youve finished treatment.
What Can People Infected With Hiv Do To Reduce Their Risk Of Cancer Or To Find Cancer Early
Taking cART as indicated based on current HIV treatment guidelines lowers the risk of Kaposi sarcoma and non-Hodgkin lymphoma and increases overall survival.
The risk of lung, oral, and other cancers can be reduced by quitting smoking. Because HIV-infected people have a higher risk of lung cancer, it is especially important that they do not smoke. Help with quitting smoking is available through the National Cancer Institutes smoking quitline at 18774487848 and other NCI resources, which are listed on the Tobacco page.
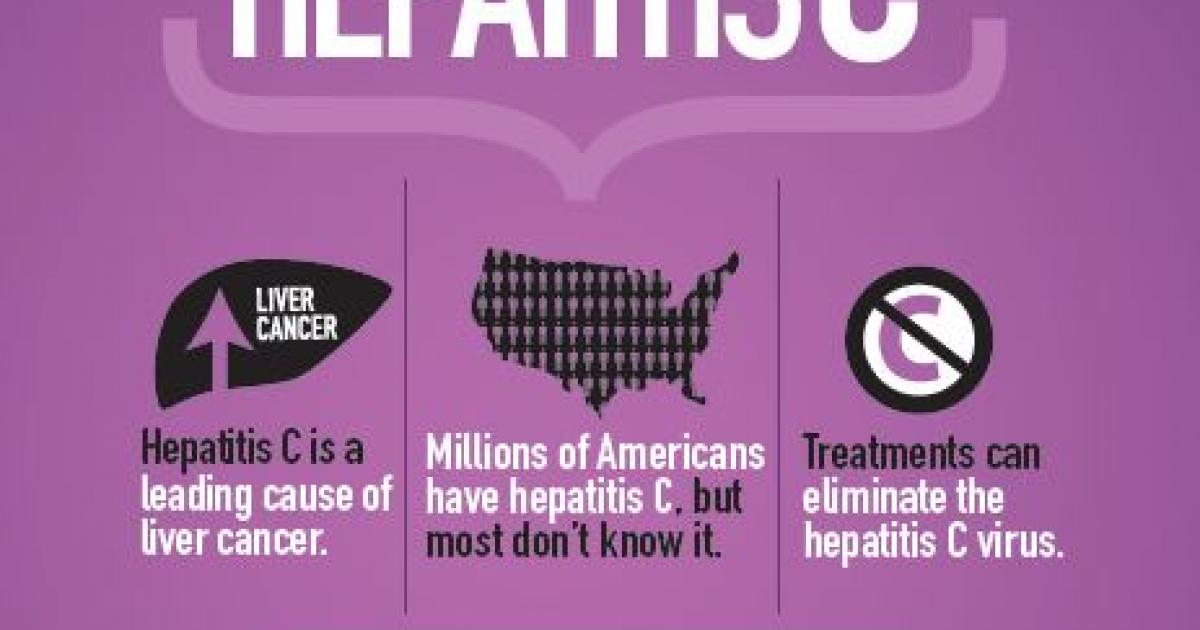
The higher incidence of liver cancer among HIV-infected people appears to be related to more frequent infection with hepatitis virus than among HIV-uninfected people . Therefore, HIV-infected individuals should know their hepatitis status.
In addition, if HIV-infected people currently have viral hepatitis, they should discuss with their health care provider whether antiviral treatment is an option for them . Some drugs may be used for both HBV-suppressing therapy and cART .
Because HIV-infected women have a higher risk of cervical cancer, it is important that they be screened regularly for this disease. In addition, the Centers for Disease Control and Prevention recommends vaccination against human papillomavirus for women and men with HIV infection up to age 26 years. Cervical cancer screening guidelines that incorporate results of a Pap test and an HPV DNA test are evolving, and women should discuss screening options with their healthcare provider .
Read Also: How Long Does Hepatitis B Last
Why Might People Infected With Hiv Have A Higher Risk Of Some Types Of Cancer
Infection with HIV weakens the immune system and reduces the body’s ability to fight viral infections that may lead to cancer . The viruses that are most likely to cause cancer in people with HIV are :
- Kaposi sarcoma-associated herpesvirus , also known as human herpesvirus 8 , which causes Kaposi sarcoma and some subtypes of lymphoma
more advanced at diagnosis, delays in cancer treatment, or poorer access to appropriate cancer treatment.
Screening And Vaccination Top Of Page
All HIV-positive patients should be screened for HBV with HBsAg, hepatitis B surface antibody and total hepatitis B core antibody . If these tests are negative, the patient should receive HBV vaccination, though HIV-infected patients do not respond as well to HBV vaccination as HIV-uninfected patients, and the persistence of protective surface antibody is short-lived . The response is poorer in patients with CD4 cell counts between 200 and 500 cells/L compared with patients with CD4 cell counts above 500 cells/L, with response rates of 33% and 87.5%, respectively . Patients who fail to respond to a conventional course of vaccine should receive booster doses or a repeat cycle with the 40-g dose .
If any of these tests are positive, HBV DNA should be measured, since atypical serologies occur in HIV coinfection . Household and sexual contacts should also be screened and vaccinated if not already immune.
Also Check: How Does Hepatitis C Spread
Natural History Top Of Page
After acute infection, there is an early replicative phase of HBV. It is during this phase that patients are most infectious and at greatest risk for development of progressive liver disease . The risk of developing chronic HBV following infection varies with age of HBV acquisition . Perinatal acquisition and infection in children younger than 1 year leads to chronic infection in 90% to 100% of cases, whereas less than 5% of adults who acquire HBV develop chronic infection . Individuals with HIV are at significantly higher risk of developing chronic HBV, with a risk of 21% in unvaccinated persons .
In chronic infection, HBV DNA titers decline over time, though HBsAg remains detectable. There is a spontaneous loss of HBeAg and anti-HBe seroconversion at a rate of about 5% to 10% per year, leading to a phase of nonreplication or low-level replication . A flare, or transient rise in alanine aminotransferase levels, often accompanies this seroconversion . What follows is a period of low HBV DNA levels, detectable only by polymerase chain reaction, and normal ALT levels . Spontaneous loss of HBsAg and anti-HBs seroconversion is less common, with an annual incidence below 1% .
| Table 2. Risk of Chronic HBV by Age of Acquisition and Immune Status. |
| Neonates |
| < 5% |
| hbv, hepatitis B virus hiv, human immunodeficiency virus |
Should People With Hiv Get Tested For Hcv
Every person who has HIV should get tested for HCV. Usually, a person will first get an HCV antibody test. This test checks for HCV antibodies in the blood. HCV antibodies are disease-fighting proteins that the body produces in response to HCV infection.
A positive result on an HCV antibody test means that the person has been exposed to HCV at some point in their life. However, a positive antibody test does not necessarily mean the person has HCV. For this reason, a positive result on an HCV antibody test must be confirmed by a second test. This follow-up test checks to see if HCV is present in the personâs blood. A positive result on this test confirms that a person has HCV.
Recommended Reading: How To Test For Hepatitis
Hiv And Hepatitis B And Hepatitis C Coinfection
Hepatitis B and hepatitis C are liver infections caused by a virus. Because these infections can be spread in the same ways as HIV, people with HIV in the United States are often also affected by chronic viral hepatitis.
Viral hepatitis progresses faster and causes more liver-related health problems among people with HIV than among those who do not have HIV. Liver disease, much of which is related to HBV or HCV, is a major cause of non-AIDS-related deaths among people with HIV.
Given the risks of hepatitis B or hepatitis C coinfection to the health of people living with HIV, it is important to understand these risks, take steps to prevent infection, know your status, and, if necessary, get medical care from someone who is experienced in treating people who are coinfected with HIV and HBV, or HIV and HCV.
What Is The Connection Between Hiv And Hbv
Both HIV and HBV spread from person to person in semen, blood, or other body fluids. For this reason, the main risk factors for HIV and HBV are the same: having sex without a condom and injection drug use.
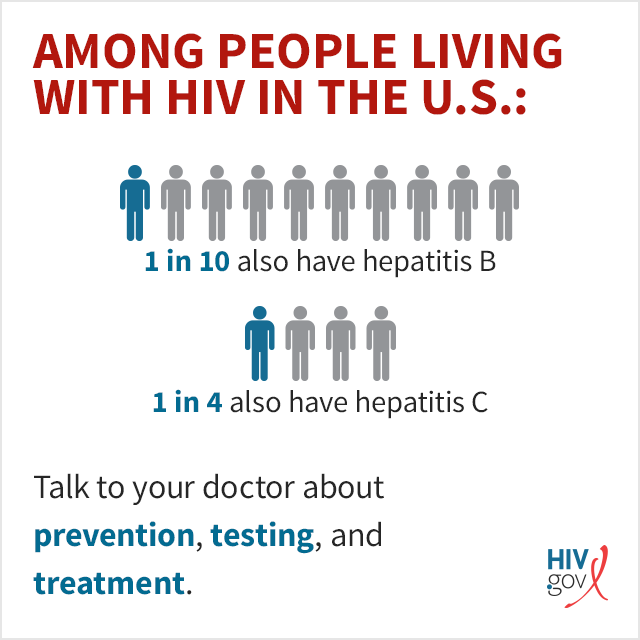
According to the Centers for Disease Control and Prevention , approximately 10% of people with HIV in the United States also have HBV. Infection with both HIV and HBV is called HIV/HBV coinfection.
Chronic HBV advances faster to cirrhosis, end-stage liver disease, and liver cancer in people with HIV/HBV coinfection than in people with only HBV infection. But chronic HBV does not appear to cause HIV to advance faster in people with HIV/HBV coinfection.
Don’t Miss: Quest Diagnostics Hepatitis B Titer
How Are Hepatitis B And Hepatitis C Spread From Person To Person
Like HIV, the hepatitis B and hepatitis C viruses spread:
- From mother to child: Pregnant women can pass these infections to their infants. HIV-HCV coinfection increases the risk of passing on hepatitis C to the baby.
- Sexually: Both viruses can also be transmitted sexually, but HBV is much more likely than HCV to be transmitted sexually. Sexual transmission of HCV is most likely to happen among gay and bisexual men who are living with HIV.
What Is The Link Between Hcv And Hiv
Both HCV and HIV are bloodborne viruses that people can acquire from sharing injection drug equipment. Although sexual transmission of HCV is less common than the sexual transmission of HIV, it can happen if there is direct exposure to blood containing HCV.
A potential complication of HIV is a coinfection. This describes when more than one infection is active at the same time. Evidence indicates that roughly 21% of people living with HIV in the U.S. also have HCV. Other data suggests that approximately 4% of people with HCV have coinfection with HIV. Globally, nearly 2.3 million people are living with an HIV-HCV coinfection.
However, these rates can vary significantly depending on an individuals risk factors. A 2016 systematic review suggests that people living with HIV were six times more likely to have hepatitis C than people without HIV. Additionally, the CDC notes that HIV-HCV coinfection occurs in of people with HIV who use injection drugs.
Chronic liver disease represents a
Also Check: How Many People Have Hepatitis C
Epidemiology Top Of Page
More than 350 million people are infected with HBV, with 75% of the worlds HBV carriers residing in Asia . Forty million people are infected with HIV worldwide. Due to shared modes of transmission, coinfection is common, and an estimated 4 million people worldwide are coinfected with HBV-HIV. The prevalence of HBV in HIV-infected individuals varies with the population studied. In the United States, up to 10% of all HIV-infected individuals have HBV coinfection . Several studies support an increased prevalence of HBV in HIV-infected populations of sub-Saharan Africa, with more than 80% of HIV-positive individuals in some of those countries carrying serum markers for HBV .
Figure 1.Geographic Distribution of Chronic HBV Infection.
HBsAg, hepatitis B surface antigen Source: Department of Health and Human Services Centers for Disease Control and Prevention. Viral Hepatitis Slidesets: Hepatitis B 101. Available here. Accessed January 15, 2007.
The prevalence of HBV surface antigen varies geographically, with high endemicity areas in Southeast Asia, sub-Saharan Africa, the Amazon Basin, parts of the Middle East, the central Asian republics, and parts of Eastern Europe. Areas of low endemicity include North America, Western and Northern Europe, Australia, and parts of South America .
Hiv And Substance Use
Substance use disorders, which are problematic patterns of using alcohol or another substance, such as crack cocaine, methamphetamine , amyl nitrite , prescription opioids, and heroin, are closely associated with HIV and other sexually transmitted diseases.
Injection drug use can be a direct route of HIV transmission if people share needles, syringes, or other injection materials that are contaminated with HIV. However, drinking alcohol and ingesting, smoking, or inhaling drugs are also associated with increased risk for HIV. These substances alter judgment, which can lead to risky sexual behaviors that can make people more likely to get and transmit HIV.
In people living with HIV, substance use can hasten disease progression, affect adherence to antiretroviral therapy , and worsen the overall consequences of HIV.
Also Check: Can Your Body Cure Hepatitis C
What Is The Connection Between Hiv And Hcv
Because both HIV and HCV can spread in blood, a major risk factor for both HIV and HCV infection is injection drug use. Sharing needles or other drug injection equipment increases the risk of contact with HIV- or HCV-infected blood.
According to the Centers for Disease Control and Prevention , approximately 21% of people with HIV in the United States also have HCV. Infection with both HIV and HCV is called HIV/HCV coinfection.
In people with HIV/HCV coinfection, HIV may cause chronic HCV to advance faster. Whether HCV causes HIV to advance faster is unclear.