What Is Hepatitis B
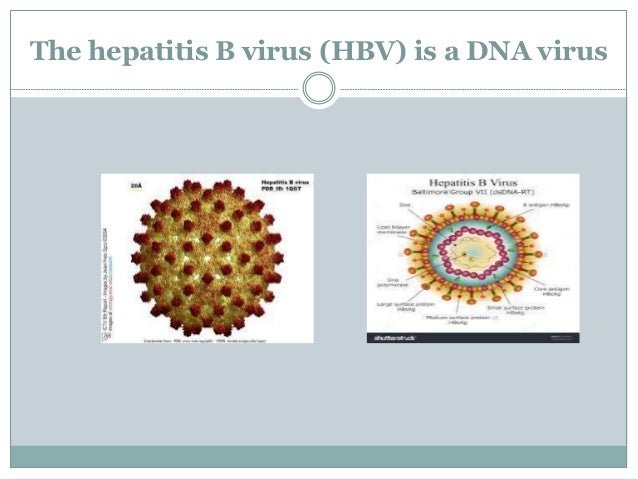
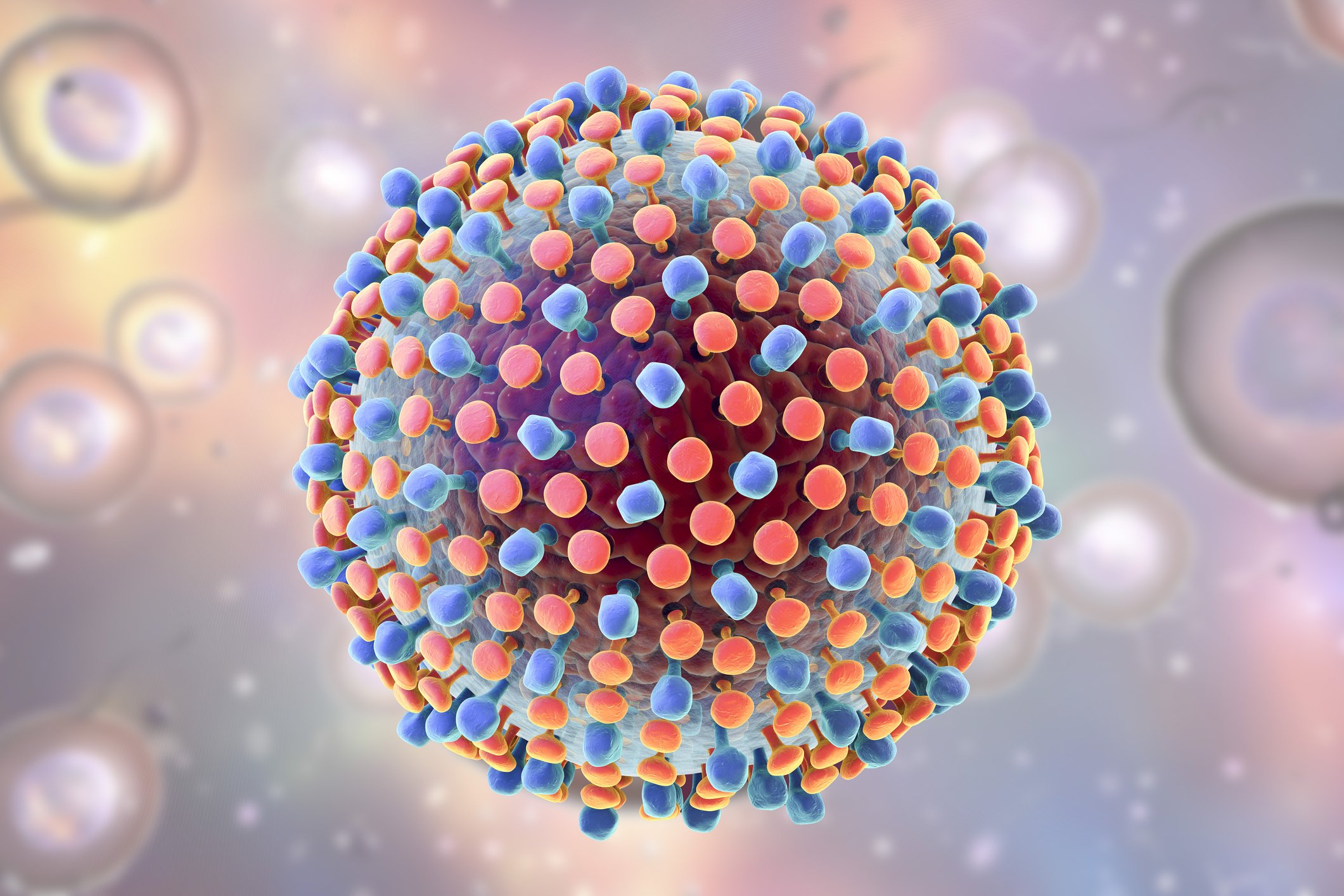
Hepatitis B is a liver infection caused by the hepatitis B virus . The abbreviation HBV can stand for either the virus or the infection it causes.
HBV can be a short-term or a long-term illness:
- Acute HBV occurs within 6 months after a person is exposed to HBV. In some people, acute HBV can lead to chronic HBV.
- Chronic HBV is a lifelong disease. Without treatment, chronic HBV can cause liver cancer or liver damage that leads to liver failure.
HBV is a contagious infection that can spread from person to person.
Functions Of The Liver
The liver serves several functions: it filters blood, removing toxic substances from drugs, food and body waste it makes bile, which is released into the gut to help digest fat and it breaks down food, releasing energy and storing vitamins and minerals. So the liver is important in getting rid of waste and in giving you energy. The liver also has a role in fighting infections, particularly in the bowel.
Impact Of Hbv And Hiv Cure Strategies
As in HIV, there has been recent increased interest in strategies that may lead to a cure for HBV. In contrast to HIV infection, there is a clear biomarker for HBV remission which is the development of antibodies to HBsAg ]. The main barriers to cure include the persistence of cccDNA and HBsAg . The use of currently available NRTIs can successfully suppress replication of HBV DNA and reduce but not eliminate HBsAg production but have little impact on cccDNA. Hence, in most individuals in the absence of HBsAg seroconversion, HBV DNA rebounds following cessation of NRTI . Furthermore, although suppression of plasma HBV DNA leads to decreased levels of fibrosis, cirrhosis and HCC, levels of HBsAg still remain elevated which may be related to the persistence of cccDNA.
Also Check: Hepatitis C Genotype 2b Treatment
Why Might People Infected With Hiv Have A Higher Risk Of Some Types Of Cancer
Infection with HIV weakens the immune system and reduces the body’s ability to fight viral infections that may lead to cancer . The viruses that are most likely to cause cancer in people with HIV are :
- Kaposi sarcoma-associated herpesvirus , also known as human herpesvirus 8 , which causes Kaposi sarcoma and some subtypes of lymphoma
more advanced at diagnosis, delays in cancer treatment, or poorer access to appropriate cancer treatment.
Hiv/aids Hepatitis And Tuberculosis
The global objective under target 3.3 of the United Nations Sustainable Development Goals seeks to end by 2030 the epidemics of AIDS, tuberculosis and combat hepatitis, among others. The EU has shown its commitment to play its role in this important endeavour by supporting actions and policies in Member States to improve their response to these three epidemics and reach the SDGs.
Also Check: Is Hepatitis A Sexually Transmitted
Hiv Hepatitis And Sexually Transmitted Infections
The HIV, Hepatitis and Sexually Transmitted Infection Unit is engaged in protecting the health of people of the Western Pacific and eliminating HIV, viral hepatitis and STIs by supporting Member States in the implementation of Regional Action Plansfor HIV, Hepatitis and STI.
Focus areas:
- Increasing access to pre-exposure prophylaxis, revitalizing condom promotion
- HIV testing community-based testing, self-testing, and partner notification
- Introduction of new/cheaper antiretrovirals
- Mid-term review of regional action plan for viral hepatitis cascade analyses and progress monitoring
- Expansion of testing services
- Prevention of health care associated infections
3. STI
- Regional review and STI disease burden estimates
- Strengthening response against gonococcal AMR and syphilis
- Explore joint action on HPV control
4. Cross cutting
- Implementation of regional framework for triple elimination of mother-to-child transmission of HIV, hepatitis B and syphilis
- Transitioning to sustainable financing mechanisms
Whats The Outlook For People Who Have Hiv And Hepatitis
HIV-hepatitis coinfections are treatable, but there are differences in the overall outlook depending on the severity and type.
For example, HCV may be cured within months, while HBV often requires lifelong treatment. If youre living with HIV, youll also need lifelong treatment for HIV, too. Complications may include cirrhosis or liver cancer.
Theres no medication available for HAV infections. If youre living with HIV and receive an HAV diagnosis, your doctor will monitor your condition carefully for complications, such as liver failure.
With treatment, HIV can become undetectable. When the virus is undetectable, it cant be transmitted to other people.
If youre living with HIV without a current hepatitis infection, your doctor may recommend regular testing to help detect hepatitis early on, depending on your risk factors. The earlier hepatitis is diagnosed and treated, the better the outcome.
Recommended Reading: What Is Hepatitis C From
B New Antivirals/strategies For Hiv And Their Impact In Hiv
i) Integrase inhibitors
In the 2016 updated WHO adult HIV treatment guidelines, first line recommended regimens have been updated to include integrase strand transfer inhibitors , consistent with guidelines from high income countries . Three INSTI dolutegravir , raltegravir and elvitegravir/cobicistat are now in widespread use.
In phase 3 randomised studies of DTG, individuals coinfected with HIV and HBV or HCV were more likely to experience liver enzyme flares which was attributed to IRID . In ART naïve individuals less liver enzyme elevations were seen in those with HIV and HBV/HCV who were on DTG in comparison to RAL. In combined analysis of three double blind, randomized controlled studies of RAL in HIV, 6% of individuals had hepatitis B or C coinfection . Liver enzyme elevations were again more common in coinfected individuals, however clinical sequelae were not seen, and there was no difference in efficacy in terms of HIV suppression between RAL and control groups. Similar results were seen in subsequent observational studies including over 150 individuals commenced on RAL, coinfected with either HCV or HBV .
iii) NRTI sparing regimens
Causes Of Noninfectious Hepatitis
Although hepatitis is most commonly the result of an infection, other factors can cause the condition.
Alcohol and other toxins
Excess alcohol consumption can cause liver damage and inflammation. This may also be referred to as alcoholic hepatitis.
The alcohol directly injures the cells of your liver. Over time, it can cause permanent damage and lead to thickening or scarring of liver tissue and liver failure.
Other toxic causes of hepatitis include misuse of medications and exposure to toxins.
Autoimmune system response
In some cases, the immune system mistakes the liver as harmful and attacks it. This causes ongoing inflammation that can range from mild to severe, often hindering liver function. Itâs three times more common in women than in men.
You May Like: Is There A Cure For Hepatitis C Virus
Factors Associated With Hiv And Hiv/hbv Co
Among the risk factors, age , gender , tattoo , marital status , province , clinical status , and chronic consumption of alcoholic beverages significantly associated with the rate of HIV infection . Of the risk factors, only age exhibited a significant association with HIV/HBV co-infection frequency. About 55% and 14% of chronic liver disease patients were chronic consumers of alcohol and cigarette smokers, respectively. Consequently, chronic alcohol consumption and smoking showed a marginal association with HCC than non-HCC cases . Compared with non-HCC, older age exhibited a significant association with HCC cases .
|
Table 3 Factors Associated with Human Immunodeficiency Virus Infection |
|
Figure 2 Trend of HIV and co-HIV/HBV infection across the different age groups of chronic liver disease patients in Ethiopia. |
What Is The Treatment For Individuals With Hiv And Hepatitis
Doctors primarily treat HIV with antiretroviral therapy. This effective treatment helps stop HIV from progressing to a later stage disease called AIDS.
With the exception of HAV, most hepatitis infections are treated with medications called antivirals. Treating HBV and HCV early is important in preventing liver diseases and cancers, some of which may be fatal.
HCV is treated with antiviral medications taken over the course of 8 to 12 weeks. The HHS says that this treatment has a 97 percent cure rate, including in people with HIV.
While HBV is also treatable, medications work to suppress the virus. They cant get rid of it entirely. Similar to HIV, treatment for HBV may be lifelong.
HAV is an acute infection. It can resolve on its own, or it can last up to 6 months, according to the . Rest and fluids are standard treatments, but more severe cases may require hospitalization.
HIV-hepatitis coinfections are treatable when detected early, according to the HHS.
Some people may take separate medications for HIV and hepatitis, like in the case of HCV. However, you can sometimes treat both viruses at the same time with the same medications. It may be helpful to find a doctor whos also experienced with treating both viruses.
Risk factors for contracting HIV or hepatitis may include:
- sharing needles, razors, or syringes
- having sex without a condom or other type of barrier method
- transmission during childbirth
Also Check: Can You Donate Blood If You Had Hepatitis A
History And Physical Exam
To diagnose all forms of hepatitis, your doctor will first take your history to determine any risk factors you may have.
During a physical examination, your doctor may press down gently on your abdomen to see if thereâs pain or tenderness. Your doctor may also check for any swelling of the liver and any yellow discoloration in your eyes or skin.
How Serious Is It
- People can be sick for a few weeks to a few months
- Most recover with no lasting liver damage
- Although very rare, death can occur
- 15%25% of chronically infected people develop chronic liver disease, including cirrhosis, liver failure, or liver cancer
- More than 50% of people who get infected with the hepatitis C virus develop a chronic infection
- 5%-25% of people with chronic hepatitis C develop cirrhosis over 1020 years
You May Like: Hepatitis B Surface Ab Ql Reactive
Inclusion And Exclusion Criteria
Inclusion Criteria
Chronic liver disease patients aged 18 years old, attending the gastroenterology units of all study sites, but mentally competent and willing to participate in the study.
Exclusion Criteria
Chronic liver disease patients with metastasized liver cancer, clinically confirmed chronic hepatic schistosomiasis, and a critical health condition/ hepatic coma were excluded from the study.
If I Have Hepatitis How Can I Avoid Giving It To Someone Else
For hepatitis A, one of the best things you can do is wash your hands a lot. That will keep the virus out of food and drinks.
If you have hepatitis B and C, you need to find ways to keep others from making contact with your blood. Follow these tips:
- Cover your cuts or blisters.
- Carefully throw away used bandages, tissues, tampons, and sanitary napkins.
- Don’t share your razor, nail clippers, or toothbrush.
- If your blood gets on objects, clean them with household bleach and water.
- Don’t breastfeed if your nipples are cracked or bleeding.
- Don’t donate blood, organs, or sperm.
- If you inject drugs, don’t share needles or other equipment.
Show Sources
Read Also: How Often Do You Need Hepatitis B Vaccine
Management Of Hepatitis Co
Initial assessment
Since HBV, HCV and HIV share common routes of transmission, initial assessment of an HIV infected patient should include a detailed history and physical examination looking for symptoms and signs of viral hepatitis and chronic liver disease. Liver function tests should be routinely checked together with viral serology including IgG anti-hepatitis A virus, HBsAg, anti-HBc and anti-HCV. Occult HBV and/or HCV infection is not uncommon in HIV-infected patients. If a patient has negative hepatitis serology but unexplained impairment in liver function, HBV DNA and HCV RNA should be checked as well.
In patients confirmed to have HBV-HIV or HCV-HIV co-infection, further assessment is necessary because the risk of advanced liver disease is increased. Complete blood count should be performed to look for thrombocytopaenia, and ultrasound scan should be arranged to rule out cirrhosis. Liver biopsy should be considered when a decision of treatment needs to be based on the severity of liver fibrosis. This is particularly important for genotype 1 HCV infection which is less likely associated with sustained virological response. Alpha-fetal protein should be performed every 6 months to screen for hepatocellular carcinoma. In patients confirmed to have liver cirrhosis, upper gastrointestinal endoscopy to screen for varices is recommended.
Hepatitis vaccinations
What Is Viral Hepatitis
Hepatitis means inflammation of the liver. The liver is a vital organ that processes nutrients, filters the blood, and fights infections. When the liver is inflamed or damaged, its function can be affected. Heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by a virus. In the United States, the most common types of viral hepatitis are hepatitis A, hepatitis B, and hepatitis C.
Don’t Miss: What Is The Definition Of Hepatitis
Special Considerations For Antiretroviral Therapy In Patients With Hepatitis C Virus/hiv Coinfection
Special considerations for ART in patients coinfected with hepatitis C virus and HIV include the following:
Patients receiving or considering therapy with ribavirin should avoid didanosine, stavudine, and zidovudine.
Use caution with antiretroviral agents with the greatest risk of DILI .
Assess cirrhotic patients for signs of liver decompensation according to the Child-Turcotte-Pugh classification system hepatically metabolized antiretroviral drugs may require dose modification or avoidance in patients with Child-Pugh class B and C disease.
Treatment of both HCV and HIV can be complicated by drug interactions, drug toxicities, and pill burden. Many of the newer directly acting anti-HCV drugs have significant interactions with antiretroviral agents however, ledipasvir with sofosbuvir and daclatasvir plus sofosbuvir have been demonstrated as efficacious.
Regimen selection for HCV infection can vary based on genotype, history of prior HCV treatment, stage of underlying liver fibrosis, and, in rare cases, the presence of baseline NS5A inhibitor resistanceâassociated substitutions.
A Hiv Replication In The Liver
A number of studies have shown various cell types in the liver are permissive to HIV infection in vitro including HSC, Kupffer cells and hepatocytes . HIV infection of these cells has also been demonstrated in vivo in individuals naïve to ART and HIV sequences from the liver in individuals off ART have distinct compartmentalised sequences when compared to other tissue sites . There have been few studies to determine whether HIV persists in the liver on ART but studies of animal models, including SIV-infected macaques and HIV-infected humanized mouse models both suggest that HIV can persist in the liver on ART, primarily in Kupffer cells . Recently, infectious replication competent HIV was isolated from Kupffer cells obtained from liver at autopsy from three HIV-infected individuals who died on ART .
In the absence of virus replication on ART, HIV may also contribute to liver inflammation and fibrosis by binding of gp120 to CXCR4 which is expressed on hepatocytes and HSC . The effect of HIV infection and or HIV proteins in the liver has primarily been studied in the context of HIV-HCV co-infection in vitro but not in HIV-HBV co-infection. HIV infection alone, or in the presence of HCV, induced profibrotic processes in hepatocyte and HSC cell lines including increased chemokine production, HSC migration, hepatocyte apoptosis and expression of profibrotic genes .
Recommended Reading: Hepatitis C Symptoms In Child
Screen And Understand Results
The only way to diagnose chronic viral hepatitis is blood testing. Viral hepatitis screening includes multiple tests and can be complex. These resources may help to identify which tests are most appropriate for your patient.
- The U.S. Preventive Services Task Force has published recommendations to screen for hepatitis B in pregnant women as well as hepatitis B and hepatitis C in persons at high risk for infection.
- CDC provides these resources on viral hepatitis screening:
- Hepatitis A, hepatitis B, and hepatitis C testing guidelines and recommendations that include PDF resources for testing sequences and interpreting test results
- Hepatitis B testing guidelines, recommendations, and resources for pregnant women and infants to prevent perinatal transmission of hepatitis B and
- Hepatitis B and hepatitis C testing and diagnosis FAQs for health professionals.
Diagnosing Hepatitis C In People Living With Hiv
Everyone with HIV should be tested to see if they also have hepatitis C. A blood test for antibodies to hepatitis C is used to see whether you have been exposed to the virus. You might be given a PCR test to confirm infection.
In people living with HIV, the diagnosis of hepatitis C can be more difficult, as the infection may not show up on their antibody tests.
If you think you may be at risk of hepatitis C infection, you should have regular tests to see if you have been infected with the virus.
Also Check: What Are The Symptoms Of Hepatitis B Virus
Treatment Of Hepatitis B Virus With Coexisting Hiv Infection
Patients with HIV infection are at a greater risk for hepatitis B virus infection, due to the common route of transmission.
Patients with HIV infection are at a higher risk of developing cirrhosis, hepatic decompensation, and hepatocellular carcinoma than patients diagnosed with only chronic HBV infection.
Treatment of HIV infection may improve the virological, histological, and clinical evolution of chronic HBV infection.
Several antiretroviral agents, such as emtricitabine, lamivudine, and tenofovir, have activity against HIV and HBV, while others, such as entecavir, have limited activity against HIV but lead to the development of HIV-resistant strains if used alone.
Prior to the initiation of ART, all patients who test positive for hepatitis B surface antigen should be tested for HBV deoxyribonucleic acid using a quantitative assay to determine the level of HBV replication.
Chronic HBV is defined as testing positive for HBsAg on 2 occasions for more than 6 months patients with chronic HBV infection already receiving ART active against HBV should undergo quantitative HBV DNA testing every 6-12 months.
Routine screening and immunization are recommended for all HIV-infected patients to prevent primary HBV infection however, the immune response to HBV vaccine is lower in patients with HIV infection than in uninfected patients, and postvaccination HBsAg must be tested to document immunity.