Expanding The Kidney Donor Pool With Hepatitis C
Surgery Spring 2018 Winter 2019 Cutting Edge
Each year in the U.S., some 500 kidneys are deemed ineligible for donation and are discarded because they came from deceased donors who are hepatitis C-positive. Transplanting these organs into recipients who are virus free has been generally considered too high risk, and only a tiny fraction of patients awaiting kidney transplant are infected with the virus. Now, a recent study led by Johns Hopkins suggests that direct-acting antiviral prophylaxis before and after transplantation could significantly alter the landscape of organ transplantation from hepatitis C-infected donors to noninfected recipients.1 In a study of 10 virus-free patients who received hepatitis C-infected kidneys, none developed clinical signs of chronic hepatitis C infection in the three months following surgery, and all have continued to remain free of the infection.
Daas In The Treatment Of Hcv Infection Post
Following the discovery of HCV and the availability of an ELISA to identify anti-HCV antibody, many cases of transmission of HCV with kidney transplantation were reported . Adverse consequences of transmission at the time of transplantation with resulting de novo HCV infection in the setting of intense immunosuppression included an aggressive form of fibrosing cholestatic hepatitis and an immune complex injury to the allograft resembling membranoproliferative GN . The use of kidneys from HCV-infected donors was discouraged, and to a great extent, these kidneys were either not retrieved or discarded .
Transmission Of Hepatitis C Virus Through Transplanted Organs And Tissue Kentucky And Massachusetts 2011
Please note: An erratum has been published for this article. To view the erratum, please clickhere.
On September 29, 2011, the United Network for Organ Sharing notified CDC of two patients who tested positive for hepatitis C virus infection approximately 6 months after receiving kidney transplants from a deceased donor. Before transplantation, the donor had tested negative for HCV antibody by the organ procurement organization. Tissue also was procured from the donor for possible transplantation. The tissue bank performed an HCV antibody test on the donor’s serum specimen that was negative and nucleic acid testing that was positive, but misread as negative. Retesting of the donor specimen during the investigation confirmed the NAT results as positive. Donated tissue included 43 musculoskeletal grafts and one cardiopulmonary patch, which were distributed to health-care facilities in several states. An investigation was initiated to 1) identify potential sources of the donor’s infection, 2) document the mode of transmission to the organ recipients, and 3) ensure timely notification of the implanting surgeons and testing of tissue recipients. Implantation of infected HCV tissue occurred after recognition of new HCV infection in the organ transplant recipients, highlighting the need for rapid communication between transplant centers, organ procurement organizations, tissue banks, and public health authorities regarding suspected transplantation transmission events.
You May Like: What Is The Treatment For Autoimmune Hepatitis
Can I Donate A Kidney If I Have Hepatitis C
In the past, having hepatitis made it impossible to donate a kidney. Now that HCV is curable, recommendations are changing.
Whether you can donate will likely come down to your overall health, and the health of your kidney. If your HCV was left untreated for a long time, your kidneys might be damaged.
Your healthcare team will conduct tests to determine if youre healthy enough to donate a kidney. If youre currently HCV-positive, your doctor might recommend treating the infection with DAAs prior to the transplant surgery to eradicate the virus.
You should ask your doctor whether previously having HCV increases the risk of complications after donating your kidney.
Transplanting Organs From Hepatitis C

Doctors at UAB are now able to safely transplant organs from hepatitis C-positive donors into uninfected recipients and then treat the patients with antiviral therapy.Four years ago, 28-year-old Ana Kenney was told that she would either spend the rest of her life on dialysis or have to wait up to 10 years for a kidney transplant.
Today, she has a working kidney and is off dialysis, thanks to a new organ transplant program at the University of Alabama at Birmingham. Doctors at UAB are now able to safely transplant organs from hepatitis C-positive donors into uninfected recipients and then cure the hepatitis C with antiviral therapy.
This has allowed more organs to be transplanted, helping patients get transplanted sooner and enabling more people to lead healthier and longer lives. In the past, organs from hepatitis C-positive donors were available only for hepatitis C-positive recipients, which led to many organs being discarded as they could not be used.
In October, UAB began transplanting kidneys and livers from infected donors into uninfected patients. The recipients are told ahead of time that the organ is from a hepatitis C-positive donor and that they will have to be treated for the illness after the transplant. If the patient agrees to accept an organ from a hepatitis C-infected donor, the transplant candidate will receive the transplant and immediately start the three-month treatment.
Also Check: Can Hepatitis Cause A Rash
Kidney Transplantation From Hepatitis
- 1Department of Renal and Pancreatic Transplantation, Manchester University NHS Foundation Trust, Manchester, United Kingdom
- 2Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom
- 3Department of Hepatology, Manchester University NHS Foundation Trust, Manchester, United Kingdom
Background: Donor hepatitis-C infection has historically represented a barrier to kidney transplantation . However, direct-acting antiviral medications have revolutionised treatment of chronic HCV infection. Recent American studies have demonstrated that DAA regimes can be used safely peri-operatively in KT to mitigate HCV transmission risk.
Methods: To formulate this narrative review, a comprehensive literature search was performed to analyse results of existing clinical trials examining KT from HCV-positive donors to HCV-negative recipients with peri-operative DAA regimes.
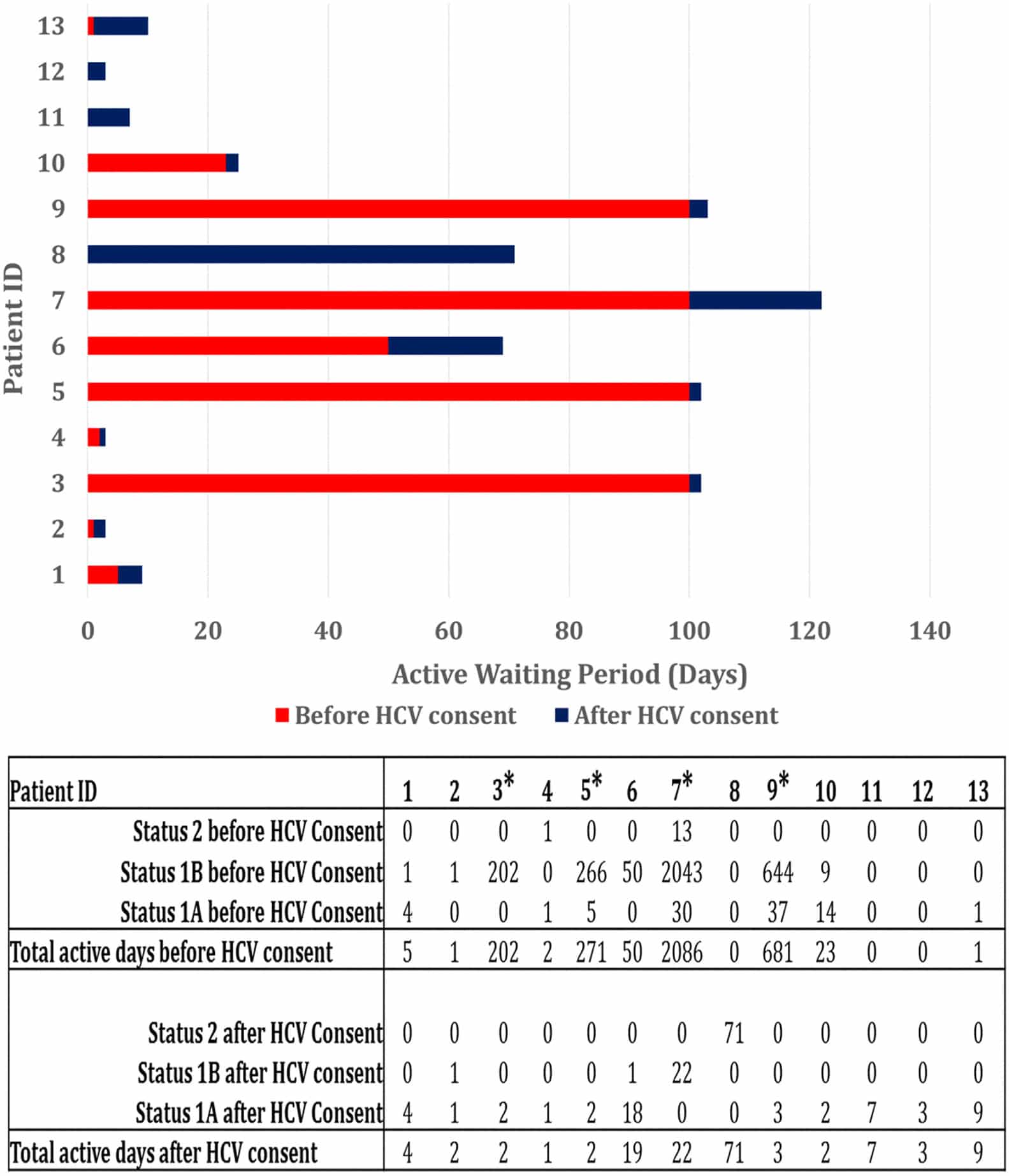
Results: 13 studies were reviewed . Outcomes for 315 recipients were available across these studies. A sustained virological response at 12 weeks of 100% was achieved in 11 studies. One study employed an ultra-short DAA regime and achieved an SVR12 of 98%, while another achieved SVR12 of 96% due to treatment of a missed mixed genotype.
Getting A Kidney Transplant When You Have Hepatitis C
You can still be eligible to get a kidney transplant if you have hepatitis C. When you have hepatitis C, your transplant team will consider the health of your liver:
- If your liver is badly damaged, you may not be recommended for a kidney transplant.
- In certain cases, if your liver is damaged but you are healthy otherwise, you may be considered for a kidney and liver transplant at the same time.
If you are approved for transplant, your doctor might suggest you get a kidney from a person with hepatitis C or from a person without hepatitis C.
Read Also: Is Hepatitis C Contagious Through Intercourse
Can I Receive A Kidney Transplant If I Have Hepatitis C
Yes, its possible to receive a kidney transplant if you have hepatitis C. Being HCV-positive shouldnt affect your eligibility. With that said, not everyone who has HCV is a good candidate for transplantation and it can be difficult to procure a donor kidney.
Your healthcare team will conduct extensive tests before recommending a transplant. If youre HCV-positive, theyll pay extra attention to your liver health. If you have complications, such as cirrhosis or liver cancer, you might not be healthy enough to undergo a kidney transplant.
On the other hand, if your liver is compromised but youre otherwise healthy, your healthcare team might consider doing a liver transplant alongside your kidney transplant. This option can involve a longer wait, though, as it requires two donor organs.
If youre recommended for a transplant, a friend or family member might be able to donate one of their kidneys to you. Otherwise, youll be placed on the Organ Procurement and Transplantation Network waiting list for a kidney from a recently deceased person.
You might have to wait more than 5 years. If youre HCV-positive, you could potentially receive a transplant faster by accepting a kidney from an HCV-positive donor.
new medical regimen for HCV revolutionized treatment.
Direct-acting antivirals can now eradicate the virus in most people. This is known as a sustained virologic response , and it means that the virus is no longer detectable in your body after a certain amount of time.
Hepatitis C And Health
How can health-care personnel avoid exposure to HCV?
Avoiding occupational exposure to blood is the primary way to prevent transmission of bloodborne illnesses among health-care personnel. To promote blood safety in the workplace, health-care personnel should consult infectious-disease control guidance from the National Institute for Occupational Safety and Health and from CDC. Depending on the medical procedure involved, Standard Precautions may include the appropriate use of personal protective equipment .
What is the risk of acquiring hepatitis C after being accidentally exposed to HCV-contaminated blood or body fluids in the workplace?
Although sharps injuries have decreased in recent decades due to improved prevention measures, they continue to occur, placing health-care personnel at risk for several bloodborne pathogens like hepatitis C. A recent analysis of several studies revealed an overall 0.2% risk for infection among those exposed to HCV-antibody-positive blood through needlestick or sharps injuries . Updated guidelines for management and treatment of hepatitis Cexternal icon are available to provide guidance for health-care personnel who become infected via exposure to contaminated blood at the workplace.
Other than needlesticks, do other exposures place health-care personnel at risk for hepatitis C?
Should HCV-infected health-care personnel be restricted in their work?
Read Also: What Is Hepatic Steatosis Of The Liver
Recommendation Regarding Timing Of Daa Therapy For Hcv
RECOMMENDED Earlya treatment with a pangenotypic DAA regimen is recommended when the patient is clinically stable. II, B a Early treatment refers to starting within the first 2 weeks after liver transplant but preferably within the first week when the patient is clinically stable.
a Other considerations in selection of the DAA regimen:
b Dosing is 3 coformulated tablets taken once daily. Please refer to the prescribing information. |
What Is The Impact On The Person Receiving The Transplant
In most cases, kidney transplantation significantly improves an individuals quality of life. A person who receives a new kidney may no longer require dialysis and can return to a more normal life.
However, kidney transplantation is not a cure for chronic kidney disease, and the individual must take medications for the rest of their life. As a result, they may still experience some physical and mental health challenges.
A persons HCV status may also affect their life expectancy following a transplant. In an earlier , doctors found that HCV-positive people have a 5-year survival rate of 77% following a transplant compared with 90% of HCV-negative patients.
However, this survival rate in transplant recipients with HCV is
Recommended Reading: Can Hepatitis B Be Cured With Antibiotics
Can People Donate A Kidney If They Have Hepatitis C
It is possible for individuals with HCV to donate healthy kidneys, either during their lifetime or after they die. However, it depends on the health of their kidneys.
Previously, people with HCV could not donate kidneys, but this has changed with the availability of direct-acting antiviral drugs. These drugs offer cure rates above 95% for people who have contracted the virus and also have chronic kidney disease or end stage renal disease.
There is a high demand for organ donors in the U.S., so a doctor may recommend using a healthy kidney from an HCV-positive donor and then treating the recipient with DAAs after the transplant surgery.
Some evidence indicates that HCV-positive individuals who receive kidneys from HCV-positive donors have than people who receive a kidney from HCV-negative donors. However, they have a shorter waiting time, which can be lifesaving.
People with HCV are not eligible for kidney donation if they have any kidney damage or disease.
Limitations Of The Study
The study has shown several limitations in that it has not addressed how some factors affect the effectiveness of DAA intervention. Additionally, given the types of studies included in this review, there is a possibility of finding a positive outcome to the research. This review does not also address the safety of DAA in organ transplants concerning other factors. It has also failed to address the effectiveness of DAA treatment regimens in patients requiring transplantation of other organs aside from the heart, kidney, and liver.
Also Check: Can A Hepatitis B Carrier Get Vaccinated
Hepatitis C Positive Organs In Heart Transplant Recipientsthe Old Era
Studies of organ transplantation from HCV positive donors to HCV naïve recipients in the old era demonstrated a variable but unacceptably high rate of HCV transmissibility , associated with poor outcomes. A retrospective study of 34 HCV naïve HT recipients showed a threefold higher risk of mortality and 2.8-fold greater risk of coronary allograft vasculopathy among patients who received HCV+organs compared to those who received HCVorgans . In another study, 261 HT recipients of HCV+donors demonstrated 50% lower survival at 1, 5, and 10 years compared to recipients of HCVdonor hearts, with significantly higher rates of mortality related to viral hepatitis or liver failure, as well as CAV . It was in this context during the old era that HCV+donor organs were generally considered unsuitable for HT.
Future Considerations For United Kingdom Application
Real world data from the US has demonstrated that outside of clinical trials, where regimens are supplied by manufacturers or funding for DAA therapy is guaranteed, there have been difficulties in acquiring approval from insurers following HCV transmission . Many funders are reluctant to provide cover for a pre-emptive or prophylactic DAA regimen and subsequently favour transmit and treat approaches . Consequently, this has led to delays in treatment . Such delays have the potential to induced sequelae of HCV infection, with serious implications such as fibrosing cholestatic hepatitis . It should be noted that treatment failure has the potential to induce devastating complications including graft loss. Concerns have also been raised regarding the increased risk of the development of BK viraemia and cytomegalovirus and severe cases have coincided with the formation of de novo donor specific antibodies . Studies to date have not noted significant difference in the prevalence of such viral complications, but when such events occur, the severity has been increased . Consequently, thorough surveillance strategies will be required.
Also Check: Hepatitis C Can You Catch It
Does The Evidence Support Accepting A Kidney From An Hcv
Transplanting a kidney from an HCV-infected donor into an HCV-positive or HCV-negative recipient is an exciting opportunity to increase access to transplantation. This has been made possible by the unique coincidence of timing and events, whereby highly effective antiviral therapies became available at the same time that we have been witness to a dramatic increase in the number of kidneys available from HCV-infected donors as a consequence of the opioid epidemic. For the patient already infected with HCV, the available evidence suggests that the answer to this question is yes in most circumstances. In contrast, the trials in which kidneys from viremic donors were transplanted into uninfected recipients are limited by their small size and short follow-up time. Nevertheless, they have caught the attention of both transplant professionals and patients with ESKD facing long waiting times for a deceased donor kidney .
The implied advantages of accepting an HCV-infected kidney must be weighed against the risk of FCH, altered immune responsiveness leading to the emergence of other viral infections , and potential logistical challenges to obtain the DAA medications. In addition, any patient that is considered for an HCV-positive organ should be evaluated by a hepatologist to ensure that he or she will be a candidate for DAA treatment and for a liver transplant should antiviral treatment fail and progressive liver injury occur after acquiring de novo HCV post-transplant.
What Is The Procedure
Before individuals can undergo a kidney transplant procedure, they must find a suitable donor who fits their specific health criteria. A donor can be an individual who has recently died and stipulated their wish to donate a kidney, or it can be a living donor who wants to give a kidney to the person in need.
Following a doctors identification of a suitable donor, a kidney transplant from a live donor usually involves the following steps:
With donations from deceased individuals, the procedure for the recipient is much the same. Instead of taking the kidney from a live donor, doctors carefully chill and package a kidney from a recently deceased donor and transport it to the hospital.
Read Also: Hepatitis C Symptoms In Males And Females
Daa Medication For Hcv
HCV positivity is defined as a positive HCV antibody in a donor. A donors high-risk behavioral features may put them at risk of spreading HCV due to the window period, or the interval between infection and detection by a certain testing procedure . A nucleic acid testing assay that detects HCV virus RNA in the donors blood is advised for these high-risk donors. NAT tests reduced the time between HCV infection and detection from 70 days to 35 days. The advent of NAT has led to a redefinition of the phrase HCV-positive donor by the American Society of Transplantation . A NAT-negative HCV donor indicates that the infection has cleared up on its own or has been successfully treated. An HCV-seropositive and NAT-positive donor indicates active infection and a high risk of disease transmission. HCV transmission is highly permissive in recipients of HCV-positive donor organs, with infection based on several genetically distinct donor viruses. However, at week 12 after medication, all participants achieved clinical cure from HCV infection with SVR, and have maintained HCV clearance .