How Is Autoimmune Hepatitis Treated
Treatment works best when autoimmune hepatitis is found early. The goal of treatment is to control the disease and to reduce or get rid of any symptoms .
To do this, medicines are used to help slow down or suppress your overactive immune system. They also stop your body from attacking your liver.
Once you have started treatment, it can take 6 months to a few years for the disease to go into remission. Some people can stop taking medicine, but often the disease comes back. You may need treatment now and then for the rest of your life. Some people need to remain on treatment if they have relapsed many times or if their disease is severe.
In some cases autoimmune hepatitis may go away without taking any medicines. But for most people, autoimmune hepatitis is a chronic disease.
It can lead to scarring of the liver . The liver can become so badly damaged that it no longer works. This is called liver failure.
If you have liver failure, a liver transplant may be needed.
Be sure to ask your healthcare provider about recommended vaccines. These include vaccines for viruses that can cause liver disease.
Incomplete Or Failed Response To Treatment
Some people with autoimmune hepatitis have an incomplete response to treatment, meaning that treatment helps but does not lead to remission. If you have an incomplete response to treatment, you may need to take different medicines to help prevent liver damage.
Some people may fail to respond to treatment, meaning that the inflammation and liver damage of autoimmune hepatitis keep getting worse. Your doctor may recommend additional blood tests and higher doses of medicines. If liver damage leads to complications, you may need treatment for complications.
Exacerbation Recrudescence And Relapse
During the course of maintenance therapy with corticosteroids/AZA, a substantial number of AIH patients spontaneously and asymptomatically experience biochemical exacerbation or recrudescence, i.e., an elevation of ALT coupled with or without an increase in IgG. The 2019 AASLD practice guidance and guidelines strictly define relapse as disease exacerbation that occurs after remission and drug withdrawal or by nonadherence . Multiple relapses have been shown to be associated with worse outcomes , but the definitions of relapse in the literature differ from that issued by the AASLD, including the concept that biochemical remission may not have proceeded relapse. Following the AASLD rules regarding biochemical remission-induction with first-line or even second-line drugs could result in fewer exacerbations. Relapse after drug withdrawal and exacerbation should be managed appropriately to induce re- remission with an increase in dosage or the reinstitution of immunosuppressive agents, or with the add-on of second-line drugs. In a case-control study, psychological stress was associated with relapse after drug taper-off or recrudescence .
Also Check: Pcr Quantitative Test For Hepatitis C
Unmet Needs And Future Persperspectives
The topics not addressed in this review include genetics, potential therapeutics based on the current understanding of the immune-pathogenesis of AIH, the inequity of AIH disease management worldwide, and patient-reported outcomes highlighted by the health-related quality of life. For example, the marked disparity in the prevalence of cirrhosis around the world, exemplified by the very high rate in South Asia , should be evaluated based on determinations of the patients genetic backgrounds and managed by the standardization of diagnosis and treatment. Improvements are anticipated regarding the accessibility to the flowchart of AIH diagnosis, with special attention to the differential diagnosis from emerging pandemic NASH. At the same time, the health-related quality of life of AIH patients, which was reported to be severely impaired , must be evaluated for future improvement from the standpoint of personalized management including appropriate first-line therapy even with potential therapeutics, and by the prediction of the success of treatment withdrawal. Using a multifaceted approach, we hepatologists are encouraged to achieve AIH patients total wellness.
Why Do We Treat Autoimmune Hepatitis With Steroids And Azathioprine
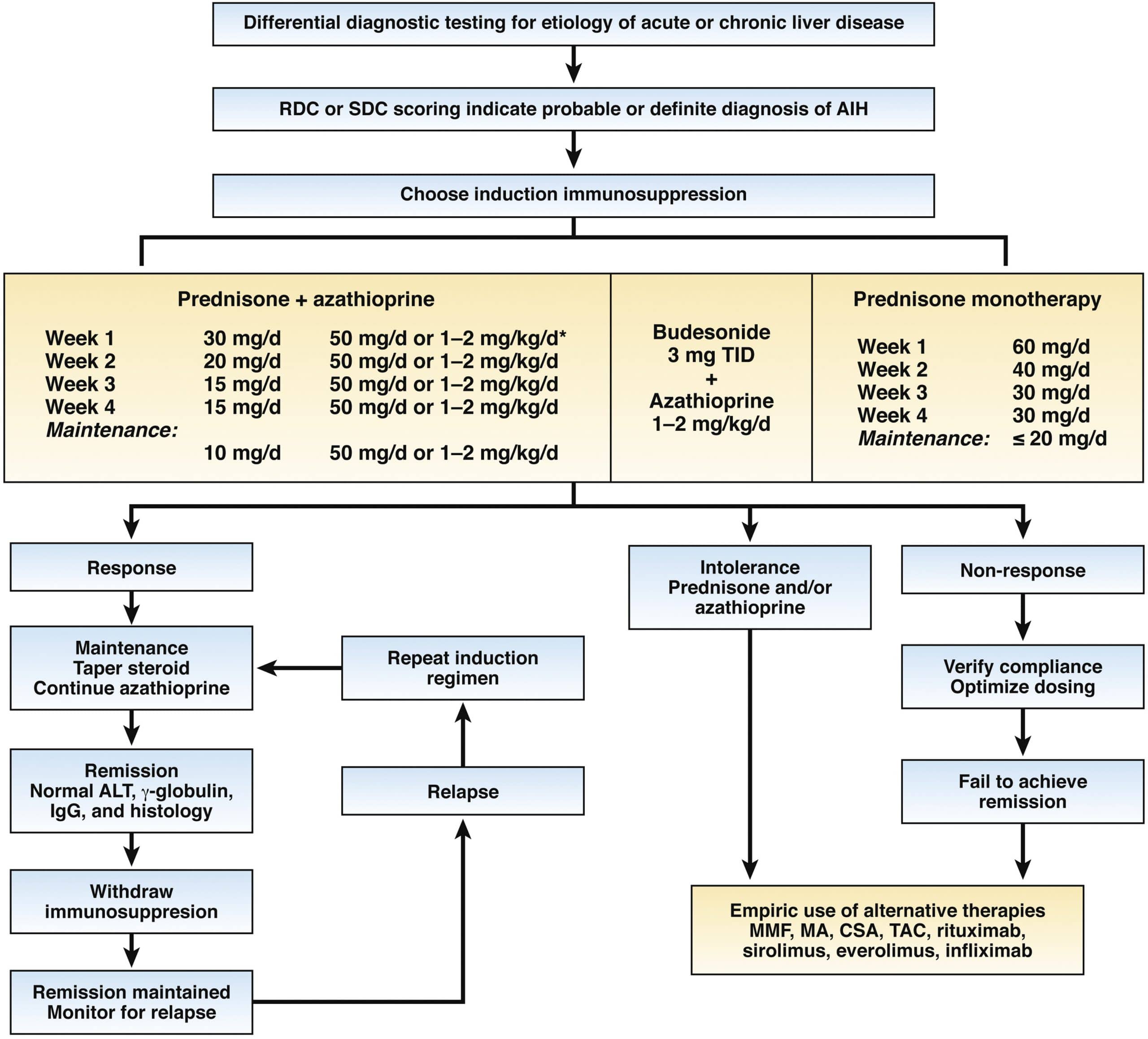
Despite the limitations of these early trials, prednisone ± azathioprine remains the mainstay of treatment for AIH, several reports showing high remission rates and favourable outcomes in both adult and juvenile AIH.
Of note, azathioprine monotherapy, though unsuccessful in the induction of remission, is effective in adults as maintenance therapy, at a dose of 2 mg/kg per day. A 5-patient report suggests that it may be effective also in children. In a recent retrospective series, 87% of 66 children with AIH were reported to maintain sustained biochemical remission in association with low 6-thioguanine nucleotides levels on an azathioprine dose of 1.2-1.6 mg/kg per day with or without associated steroids.
Also Check: How Much Is A Hepatitis A Shot
Genetics And Predisposing Factors
Autoimmune hepatitis is thought to result from an environmental trigger in a genetically predisposed individual, leading to loss of tolerance of T lymphocytes with subsequent hepatocyte attack.
It is a polygenic disease and does not follow a Mendelian distribution. Therefore there is no need to screen family members of patients with AIH. There is a strong genetic association with the alleles of the major histocompatibility complex class II. The presence of human leukocyte antigen genes HLA DRB1*03 and HLA DRB1*04 predisposes to AIH type 1 and affect the disease course and response to treatment. Individuals who are positive for HLA DRB1*03 are younger, respond less favorably to corticosteroid therapy, and progress more often to liver failure. On the other hand, the presence of HLA DRB1*04 is associated with higher rates of concomitant autoimmune disorders.
Autoimmune hepatitis can also be associated with autoimmune polyendocrinopathy candidiasis ectodermal dystrophy syndrome, an autosomal recessive disease characterized by hypoparathyroidism, adrenal insufficiency, and chronic mucocutaneous candidiasis. Autoimmune polyendocrinopathy candidiasis ectodermal dystrophy is the only AIH-associated disease that follows a Mendelian pattern of inheritance and genetic counseling should be offered for patients and family members.
Table 1: Drugs Associated With Drug-Induced Autoimmune-Like Hepatitis
| Association |
|---|
What Causes Autoimmune Hepatitis
Experts dont know what causes autoimmune hepatitis, but it is more likely to show up in people with other autoimmune conditions, including:
- Fluid buildup in the belly
- Rectal bleeding or vomiting blood
The symptoms of autoimmune hepatitis may look like other health problems. Always see your healthcare provider for a diagnosis.
Also Check: How Do You Treat Hepatitis
When The Liver Is Under Attack
In people with autoimmune hepatitis, immune cells inappropriately mistake the liver’s normal cells as abnormal and attack them. Over time, this can lead to inflammation, scarring , impaired liver function, and even cirrhosis , which can result in liver failure, and death if not treated. Some people may eventually need a liver transplant. The liver disease specialists at NewYork-Presbyterians Center for Liver Disease and Transplantation are experienced in diagnosing and treating autoimmune hepatitis.
Side Effects Of Steroids And Azathioprine
Steroid side effects are dose and time dependent, and arise if a dose exceeding 7.5-10 mg/d is administered over several months. The most common side effect is the development of cushingoid features. In a retrospective monocentric study of 103 adult AIH patients, mostly treated according to a standard protocol with a steroid starting dose of 1 mg/kg per day and a mean follow-up period of 95 mo, 15.5% developed cushingoid features. Although not severe, these changes are often a great concern for the patients, and may lead to non-adherence, with the dangerous consequence of poor disease control. Almost half of AIH patients discontinue steroids because of cosmetic changes or obesity. Severe, but less frequent steroid side effects include osteoporosis, brittle diabetes, cataract, psychosis and hypertension. They are mainly related to the initial high dose, and are reversible. Monitoring of these complications is advisable, including ophthalmologic controls and bone density scans on a regular basis.
Measurement of the azathioprine metabolites 6-TGN and 6-methylmercaptopurine can be helpful in identifying drug toxicity and non-adherence, and in distinguishing azathioprine hepatotoxicity from disease non-response, as shown by a retrospective study in adults, and a small prospective study in children, but an ideal therapeutic level of the 6-thioguanine metabolites has not been established for AIH, unlike for inflammatory bowel diseases .
Don’t Miss: Best Food For Hepatitis B
Noninvasive Assessment Of Fibrosis
The long-term outcome of AIH is associated with the stage of fibrosis. Since the evaluation of liver fibrosis by biopsy during the course of disease management is not feasible, noninvasive assessments have been conducted in clinical hepatology by using serum biomarkers, including the serum AST/platelet ratio index and the fibrosis-4 index . However, a recent systemic review of the diagnostic accuracy of APRI and FIB-4 demonstrated their poor performance for detecting advanced fibrosis and cirrhosis in AIH .
Noninvasive assessment by liver stiffness has been shown to identify advanced fibrosis and cirrhosis in AIH with reasonable accuracy. The performance levels of vibration-controlled transient elastography and magnetic resonance elastography were indicated to be superior to those of the APRI and FIB-4, and VCTE was validated in a systemic review as providing good performance . Considering that liver inflammation affects liver stiffness, the stiffness value at the initial diagnosis before the initiation of treatment with immunosuppressive agents is confounded by disease activity. In fact, the value of VCTE within 3 months after the start of treatment was significantly correlated with histological grading, but not with the fibrosis stage . Thereafter, at least 6 months after the successful treatment of AIH, the area under the receiver operating curve of VCTE reached 1.0 . Sustaining biochemical remission and the use of VCTE help monitor and manage the disease course of AIH.
How Do Doctors Treat Autoimmune Hepatitis
Doctors treat autoimmune hepatitis with medicines that suppress, or decrease the activity of, your immune system, reducing your immune systems attack on your liver. The medicines doctors most often prescribe are corticosteroidsprednisone or prednisolonewith or without another medicine called azathioprine.
Doctors typically start with a relatively high dose of corticosteroids and then gradually lower the dose. Your doctor will try to find the lowest dose that works for you. Your doctor will use blood tests to find out how you are responding to the treatment. A decrease in levels of the liver enzymes alanine transaminase and aspartate transaminase shows a response to treatment. ALT and AST falling to normal levels shows a full response. In some cases, a doctor may repeat a liver biopsy to confirm the response to treatment and find out whether the damage has resolved.
Treatment can relieve symptoms and prevent or reverse liver damage in many people with autoimmune hepatitis. Early treatment of autoimmune hepatitis can lower the chances of developing cirrhosis and other complications. A minority of people who have no symptoms or only a mild form of the disease may or may not need medicines.
Read Also: How Do People Contract Hepatitis C
What Are The Symptoms And Complications Of Autoimmune Hepatitis
Often, the symptoms of autoimmune hepatitis are minor. When symptoms do occur, the most common are fatigue, abdominal discomfort, aching joints, itching, jaundice , enlarged liver, nausea and spider angiomas on the skin. Other symptoms may include dark urine, loss of appetite, pale stools and absence of menstruation. More severe complications can include ascites and mental confusion. In 10%-20% of cases, autoimmune hepatitis may present with symptoms like an acute hepatitis.
What Are The Current Treatment Options
Very mild cases or inactive phases of the disease may not require treatment. However, for more serious cases, treatment to fight acute episodes is important.
For many individuals, lifelong medication use may be required to keep the bodys autoimmune response under control and preserve liver health.
The two main medications used to treat autoimmune hepatitis are:
- prednisone: a corticosteroid
- azathioprine: an immunomodulator or steroid-sparing agent
Other medications may be added in severe cases. If medications are no longer effective and liver failure is likely, a liver transplant may be necessary.
If possible, your treatment should be supervised by a hepatologist, which is a physician who specializes in liver health.
Also Check: Antibodies To Hepatitis B Surface Antigen
Autoimmune Hepatitis Causes And Risk Factors
Doctors aren’t sure exactly what causes your immune system to turn against your liver. Your genes may have something to do with it, since AIH can run in families.
But genes aren’t the whole story. Something you come into contact with may trigger your genes to set autoimmune hepatitis in motion. This could include:
- Medicines such as statins and hydralazine or antibiotics like nitrofurantoin and minocycline
- Infections such as viral hepatitis, herpes, Epstein-Barr, and measles
Aim And Methodology Of The Systematic Review
The aim of this review is, in its first part, to critically summarize the evidence on which standard AIH treatment is based, and, in its second part, to provide a systematic review of the published data on alternative treatments. For the purpose of the systematic review of the literature on alternative AIH treatment, publications cited in PubMed were selected using the search words autoimmune hepatitis and treatment. Citations were chosen on the basis of their relevance to the aim of this article .1). Fundamental characteristics of the abstracts judged pertinent to the review were noted, and full-length original articles were selected from the abstracts. Seventy-six articles were identified, 22 of them are not discussed in this review because of anedoctal reporting, the remaining 54 are included in Table Table11 and Table Table22 . Children/adolescents have a more aggressive disease, with a more frequent acute presentation and therefore need a different management. For this reason, the present review article discusses adult and pediatric treatment separately.
You May Like: What Are The Stages Of Hepatitis B
Alf And Acute On Chronic Liver Failure
AS-AIH with encephalopathy is defined as ALF caused by AIH . With regard to noninvasive diagnoses, heterogenous hypo-attenuated regions within the liver as visualized by unenhanced computed tomography is useful to differentiate patients with AS/ALF-AIH from those with viral-associated ALF . The volumetric measurement of the liver on CT is also valuable, because the size of the liver was reported to be significantly reduced in non-acetaminophen cases of acute liver injury/ALF compared to the acetaminophen-induced cases . A direct evaluation of indications for LT is recommended in ALF-AIH, because glucocorticoid therapy has not been associated with improved overall survival and is even harmful to patients with a model for end-stage liver disease score > 40 .
Fda Clears Autoimmune Hepatitis Treatment Zetomipzomib As Investigational New Drug
The FDA cleared zetomipzomib as an Investigational New Drug. A phase 2 clinical trial is the next step for this autoimmune hepatitis treatment.
This week, Kezar Life Sciences, Inc. announced their autoimmune hepatitis treatment had received clearance of an Investigational New Drug application by the US Food and Drug Administration .
The therapy, zetomipzomib, is a first-in-class, selective immunoproteasome inhibitor, intended for the treatment of autoimmune hepatitis . AIH is a rare chronic disease that causes the immune system to attack the liver. This leads to inflammation and tissue damage that ultimate severely burdens patients health and quality of life.
AIH affects approximately 140000 persons in the US, with incidence rates 4 times higher in women than men. Left untreated, AIH can lead to cirrhosis, liver failure, and hepatocellular carcinoma.
While there are AIH treatments currently available, these chronic corticosteroids can increase the burden of morbidity and mortality. With zetomipzomib, Kezar Life Sciences seeks to provide a treatment regimen to reduces the need for chronic immunosuppression via corticosteroids.
The primary efficacy endpoint will evaluate the proportion of patients who achieve a complete response, measured as normalization of alanine aminotransferase and aspartate aminotransferase levels with a successful corticosteroid taper by Week 24.
Related Content:
Don’t Miss: Hepatitis C Causes Liver Damage
What Is The Outlook For Someone With Autoimmune Hepatitis
Autoimmune hepatitis is a chronic disease, meaning you will have it for the rest of your life. With proper treatment, its possible to enjoy years of remission without symptoms and healthy liver function.
The Canadian Society of Intestinal Research suggests that people who respond well to treatment can expect to have a normal life expectancy.
Also, a 2020 study found that with proper immunosuppressant therapy, about 90 percent of the 86 people with autoimmune hepatitis in this study achieved complete remission.
How To Use Prednisone And Azathioprine
There is no treatment schedule applicable to all AIH patients. The suggested algorithms and treatment schedules must be tailored to the single patient, taking into account the severity of the disease, age and co-morbidities.
The AASLD guidelines published in 2010 recommend two alternative schedules: either prednisone alone at a dose of 60 mg/d or a combination of prednisone 30 mg/d and azathioprine 50 mg/d as initial treatment, favouring the latter because of fewer steroid side-effects. However, as azathioprine can be hepatotoxic, particularly in cirrhotic and jaundiced patients, the more recent guidelines by the European Association for the Study of the Liver recommend that it is added after two weeks of steroid monotherapy , when partial disease control has been achieved. In addition, this approach avoids the problem of distinguishing between azathioprine-induced hepatotoxicity and non-response, this distinction being an important issue in clinical practice. A retrospective series of 133 adult patients reports better results with a combination of steroids and another immunosuppressant from disease presentation compared to steroids alone or steroids followed by the addition of azathioprine/other immunosuppressants. Of note, only 2% of the patients included in this study were jaundiced at presentation, possibly explaining the high remission rate on azathioprine, without hepatotoxicity.
Also Check: Fast Track Hepatitis B Vaccine In Houston Tx
Who Is At Risk For Autoimmune Hepatitis
Autoimmune hepatitis affects one in every 100,000 people. The disease is more common in women than in men, and women are typically diagnosed in their 40s or 50s. Girls between two and 14 years old may also get the disease.
Those who may suffer from other autoimmune conditions, such as diabetes, rheumatoid arthritis, thyroid disease and celiac disease, are also at risk to develop autoimmune hepatitis .
A person who has a family history of autoimmune hepatitis also has a higher risk of developing the disease.