The Patient Advocate Foundation
This organization provides copay relief and a directory of national and local resources that can offset some of the financial burden of medical expenses.
Whatever the cost, the benefit to the person to eradicate hepatitis C today and not deal with complications is immense, says Joseph Galati, MD, medical director for the center of liver disease and transplantation at Houston Methodist Hospital.
The average person may not appreciate the savings from preventing somebody from getting liver cancer or a liver transplant or the disability associated with chronic hepatitis C, says Dr. Galati. Whatever the cost for treatment is, its a drop in the bucket when you look years down the line as far as the potential cost of living with hepatitis C.
How Do I Know If I Have Hep C
If youre a Baby Boomer, you have a fairly high risk but 40% of infected people dont know they have it. Chronic Hep C usually has no symptoms until liver damage is dangerously bad. Thats why guidelines say all adults should get tested for the virus at least once.
Medicare covers the cost of testing once if:
- you were born between 1945-1965
- you have a history of IV drug use
- you received a blood transfusion before 1992
Medicare Will Cover Hepatitis C Screening In Primary Care Settings
On June 2, 2014, the Centers for Medicare & Medicaid Services announced its determination that hepatitis C virus screening will be covered by Medicare for adults in primary care. Specifically, the determination stated that CMS will cover HCV screening when ordered by a beneficiary’s primary care physician or practitioner within the context of a primary care setting, and performed by an eligible Medicare provider, for beneficiaries who meet either of the following conditions:
Don’t Miss: How To Cure Hepatitis C Naturally
What We Need From Providers
Action! This is a huge opportunity to rid our state of the most common blood borne disease in the United States and now it is possible.
Effective immediately, we would like all providers licensed to treat HCV to screen and treat the target population. In order to support our provider community in this monumental effort, Apple Health has made important policy changes:
- The antiviral Mavyret no longer requires prior authorization . Other direct-acting antivirals will require review and will be approved only when Mavyret is not clinically appropriate.
- Anyone licensed to prescribe direct acting antiviral medications is allowed to screen and treat Apple Health members to support this effort.
Medicare Coverage Allows For Treatment Success
Sherilyn C. Brinkley, a certified registered nurse practitioner and a program manager at the Johns Hopkins Viral Hepatitis Center in Baltimore, advised Pannell on his care. She says he was fortunate to receive Medicare coverage.
What came with this incredibly easy, short, extraordinarily effective regimen was a really high cost, Brinkley says. Ever since then, weve been able to cure thousands of patients just here in Baltimore. But weve had to really struggle with access to drugs along the way. Many are still not able to get treated because of the cost, and thats a frustrating element of this whole process.
Also Check: How Do You Cure Hepatitis B
How Part D Plans’ Preference For Higher Cost Hepatitis C Drugs Affects Medicare Beneficiaries
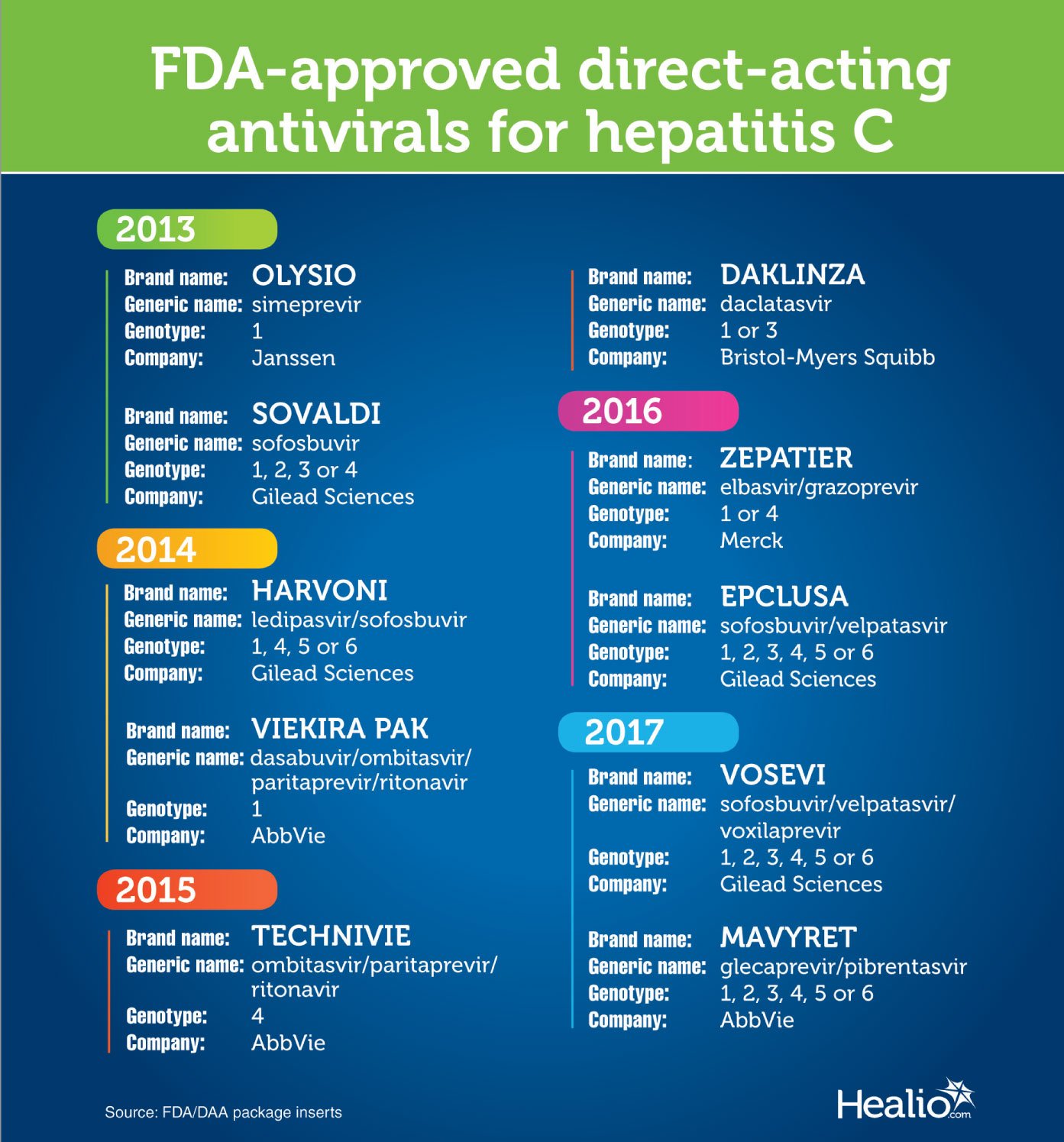
In 2019, Medicare Part D spent approximately $2.5 billion for hepatitis C drugs to treat 50,000 beneficiaries with the disease. Three drugsHarvoni, Epclusa, and Mavyretaccounted for 93 percent of expenditures, with annual Medicare costs ranging from $28,000 to $77,000 per beneficiary. A portion of these totals was shared by Medicare beneficiaries who faced thousands of dollars in out-of-pocket costs for hepatitis C drugs under Part D. In early 2019, Gileadthe manufacturer of Harvoni and Epclusalaunched authorized generic versions of both drugs with the expressed goal of reducing patients’ outofpocket costs. The retail price of authorized generic versions is $24,000, which is significantly less than the prices of Harvoni and Epclusa, and even less than Mavyret. These lower list prices should in turn lead to lower out-of-pocket costs, as authorized generics are as effective as branded versions but sell for only a fraction of the cost. However, a preliminary analysis indicates that Medicare utilization has not shifted from brandname versions of Harvoni and Epclusa to their significantly cheaper, authorized generic versions or to Mavyret. This study will examine the utilization of hepatitis C drugs under Part D and the financial impact on Medicare Part D and beneficiaries.
| Announced or Revised |
|---|
Does Medicare Cover Hep C Testing
Medicare typically does cover Hepatitis C testing one time if you have risk factors that put you at a high risk for getting Hepatitis C.
Medicare Advantage plans may also cover Hep C testing that meets eligible criteria and is ordered by a doctor. Many Medicare Advantage plans also cover prescriptions drugs, which Original Medicare doesnt cover.
Also Check: How Can One Get Hepatitis C
Medicare Coverage For Single And Repeated Hepatitis C Screenings
Depending on your situation, Original Medicare will cover a one-time screening or repeated hepatitis C screenings.
Single Screening vs. Repeat Screening Coverage
- Single Hepatitis C Screening Coverage
- Original Medicare covers a single screening for beneficiaries born from 1945 through 1965 but do not have other high-risk factors.
- Repeated Hepatitis C Screening Coverage
- Original Medicare covers repeated hepatitis C screenings for certain high-risk beneficiaries. These include people who have used illicit injectable drugs in the past or for those who have received a blood transfusion prior to 1992. Medicare will pay for annual screenings for people still using illicit injectable drugs since their last negative screening.
Your doctor or other primary care provider will determine whether you are at high risk for HCV based on your medical history. This assessment typically comes as part of your Medicare annual wellness visit and the development of the comprehensive prevention plan you and your doctor create.
Edema Symptoms Lead To Diagnosis
The Baltimore resident found out he had the disease in 2018 after his feet swelled up. My feet were so bad, I had to take the shoestrings out of my shoes so I could walk, he says.
When he visited nearby Johns Hopkins Hospital to get help, the medical team conducted a simple blood test to see if Pannell had hepatitis C.
Edema, a swelling of the feet, ankles, or legs due to a buildup in fluids, is a common symptom of cirrhosis.
I couldnt believe I tested positive, says Pannell, 64. I was mad, but I figured that I probably got the disease from sharing needles because I was an addict at one time. Today, Im going on 17 years clean.
After completing eight weeks of antivirals, Pannell was retested. He still had hepatitis C. I was frustrated and discouraged that it didnt work, says Pannell, but my care provider said lets try it again.
After a second round of therapy, Pannell was cured.
Recommended Reading: How To Spread Hepatitis B
How Does Medicare Cover Hepatitis Screenings
Hepatitis C is a viral infection that can lead to serious liver damage if untreated. Medicare Part B may cover one-time Hep C testing for patients who are at high risk of contracting the virus.
You are considered high risk if you meet one or more of the following criteria:
- You use or have used illicit injected drugs
- You had a blood transfusion earlier than 1992
- You were born between 1945-1965
If you are considered at risk for Hep C, Medicare Part B will also cover yearly screenings to check on your health compared to your initial Hep C test.
Medicare Part B may also cover Hepatitis B Virus screening if youre at high risk for HBV or if youre pregnant.
How Do You Get Tested For Hep C
Hepatitis C is tested with a blood test that measures antibodies to the virus. When you get tested, a lab technician will draw some bleed from a vein with a small needle, and the blood sample will be tested for antibodies to the Hepatitis C virus.
Once youve been infected with the Hepatitis C virus, you will always have antibodies in your blood. While the antibodies will always be in your body, it may be confusing to understand your test results.
- If your test comes back non-reactive, or as a negative antibody result, this means that you dont have a current, active infection from the virus. However, if you suspect you may have been infected with the virus at some point in the last six months, a repeat test is recommended.
- A reactive test, or positive antibody result, means that you were infected with Hepatitis C at some point, but you might not have a current, active infection.
Don’t Miss: Facts About Hepatitis C Virus
Tracking The Costs Of Hepatitis C Treatment
Researchers are continuing to create medications that shorten the duration of treatment for hepatitis C.
According to the Pharmacy Times, the cost of treatment can be as low as $54,600 for the 12-week course and the entry to the market of new, cheaper drugs is likely to continue to bring the cost of hepatitis C treatments down.
The level of insurance cover for hepatitis C treatments can vary, depending on a persons insurance policy and overall health.
Some insurance companies will pay for people whose hepatitis C has not responded to less-expensive treatments or for those who are already showing signs of liver damage.
Some insurance companies may require a person to prove they have been drug- and alcohol-free before authorizing treatment.
Insurance companies may believe people who fall into these categories will cost them less money.
If a person has a hepatitis C diagnosis, they may first ask what treatments their doctor recommends. Then, they should contact their insurance company to find out what medications their insurance plan may cover.
Even if an insurance plan does not provide cover for treatments, there are still some patient assistance programs that help reduce the costs of specific treatments.
To find out about these, people can try researching the following:
Obtaining additional financial assistance and discounts can sometimes be a time-consuming and frustrating process.
Does Medicare Cover The Newer Hep C Treatments
The short answer is yes. Medicare requires each Part D or Medicare Advantage plan to have at least one of the new DAAs in its formulary, or list of covered drugs.
But the real answer is more complicated. Before we share the good news, heres what you need to know: Even though one of these Hep C drugs is covered, your doctor cant just write you a prescription. Youll have to go through a few steps first:
- Medical necessity: Youll need to get coverage approved first before Hep C medications are covered and you wont get it unless the drugs are medically necessary. You might need to show that you have liver damage or you might need to try a less expensive treatment first. Work with your doctor on the testing and paperwork. Its time consuming, but worth it.
- Patient readiness: You might need to show your readiness to undergo treatment. That could mean taking a urine test to show youre not currently using recreational drugs. Your doctor may also need to promise that youll take the medications properly.
- Cost: Because theyre expensive, even when theyre covered, these drugs can have a co-pay as high as 30%. You could be paying almost a third until you hit your policys out-of-pocket maximum and youll probably still pay 5% of the cost after that. Even with insurance, that can add up. But dont lose heart. Keep reading to find out how to make it work.
Recommended Reading: At What Age Do You Get Hepatitis B Vaccine
Who Can Access The Cures
Hep C cures are now available to everyone in Australia who has hep C.* The national and state governments want everyone with hep C to be cured, including prisoners and people who inject drugs. Now is a very good time to consider testing for hep C or speaking to your doctor about the hep C cures.
*Cures are available to people who have a Medicare Card or Health Care Concession Card and who arent hospital inpatients.
You might be able to access healthcare and the cures via your computer or phone.
Hepatitis C And Its Treatments
More than 3 million Americans are infected with hepatitis C virus .8 Its prevalence is concentrated among baby-boomers, who were born between 1945 and 1965.8 HCV causes more deaths in the US than HIV/AIDS.9 Chronic hepatitis C is a cause of serious and costly liver diseases such as cirrhosis and liver cancer. Hospitalizations and costs related to HCV and liver diseases have increased during the past decade.10 While the burden of HCV can be reduced through screening and treatments, the implementation of recommended screening is limited and half of the infected population is not diagnosed.10
The conventional HCV treatment for the most common type of HCV consisted of peginterferon and ribavirin , which required a 48-week treatment course. The cure rate measured by sustained virologic response , defined as having no HCV RNA in blood 24 weeks after a treatment, was about 50%.11 Due to side effects of interferon, some patients could not tolerate this therapy.
The first direct acting antivirals telaprevir and boceprevir were approved in 2011. With these drugs, SVR reached 75-80%11 however, patients had to be on the PR regimen and were required to dose every 7-9 hours.
Don’t Miss: What Is Hepatitis C Infection
What Costs Should I Expect To Pay
Even with Medicare coverage, medication treatments for hepatitis C can still be costly. According to a 2017 analysis, the cost could range from $6,297 to $10,889 for the entire treatment course.
Depending on your income, you may be able to qualify for a low-income subsidy. This means youd get assistance to pay for your medication costs. According to the same analysis, Medicare beneficiaries with a low-income subsidy paid between $10.80 and $1,191 for their total hepatitis C treatment costs.
Several FDA-approved medications can treat hepatitis C. The following are some commonly prescribed medications that Medicare plans cover, as well as their estimated costs according to GoodRx.com.
| Medication | |
|---|---|
| 81% | $211$28,658 |
Cost is certainly a factor to consider in your hepatitis C treatment. However, complications from hepatitis C can be life threatening. Ideally, you and your doctor can find a treatment plan that will be affordable, safe, and effective for you.
Hepatitis C Treatment: Screening Comes First
Of course, you wonât need âhep Câ treatment unless you have the disease. Medicare Part B may cover a one-time hepatitis C screening test if itâs ordered by your primary care doctor or health-care practitioner.
In some situations, Medicare covers a repeat hepatitis C screening once a year if youâre considered high risk for getting the condition. Youâre considered high risk for contracting hepatitis C if you meet at least one of the following conditions:
- You were born between 1945 and 1965.
- You had a blood transfusion before 1992.
- You currently use illicit injection drugs, or you have a past history of illicit injection drug use.
Youâll pay nothing for this hepatitis C test if your doctor accepts Medicare assignment, meaning that he or she agrees to accept the cost Medicare has approved for the test as full payment and not charge you above that .
You May Like: What Is Hepatitis B And C
Will Medicare Pay For A Hepatitis C Vaccine
Hepatitis C is contracted in the same manner as hepatitis B. Unfortunately, theres no vaccine yet to help prevent this type.
Yet, Medicare Part B provides coverage for a one-time hepatitis C screening if you:
- Have a date of birth between the years 1945 and 1965
- Received a blood transfusion before 1992
- Have used or currently use illegal drugs via injection
For those who are high-risk, Medicare Part B covers an annual screening for hepatitis C. Qualifying screenings receive full coverage.
What Is The Treatment
If you have been diagnosed with hepatitis C, it is important to talk to your healthcare provider about what your options are. Since it can vary, so can the treatment options. If your case is mild, you may have coverage under Medicare Part B with outpatient services.
A doctor may also prescribe a medication to help with treatment. Medicare does not cover most of the prescriptions that are used to treat hepatitis C, except in special inpatient and outpatient situations.
Medicare Part D will cover certain prescription drugs in special situations.
Also Check: Is Hiv The Cause Of Hepatitis B
Who Can Help Me
If youre concerned about paying for HCV medications, remember that you arent alone as you seek treatment. There are people and organizations that can help you, including the following:
- Your doctor. They can help you by ordering and documenting the tests youll need so you can qualify to get your medications, especially if youre working with a liver or infection specialist.
- Most drug manufacturers. There are patient assistance programs that offer free or reduced-cost medications for people who meet their criteria.
- Patient advocacy groups. These groups provide assistance with all aspects of HCV treatment. For instance, if your insurer denies treatment, you can appeal the decision with help from one of these groups. Your doctor can also help in this situation.
Drug companies and patient advocacy groups are a great place to start when looking for help paying for HCV medications. Heres a list to get you started.