How Is Viral Hepatitis Prevented
Prevention of hepatitis involves measures to avoid exposure to the viruses, using immunoglobulin in the event of exposure, and vaccines. Administration of immunoglobulin is called passive protection because antibodies from patients who have had viral hepatitis are given to the patient. Vaccination is called active protection because killed viruses or non-infectious components of viruses are given to stimulate the body to produce its own antibodies.
Avoidance of exposure to viruses
Prevention of viral hepatitis, like any other illness, is preferable to reliance upon treatment. Taking precautions to prevent exposure to another individual’s blood , semen , and other bodily secretions and waste will help prevent the spread of all of these viruses.
Use of immunoglobulins
Immune serum globulin is human serum that contains antibodies to hepatitis A. ISG can be administered to prevent infection in individuals who have been exposed to hepatitis A. ISG works immediately upon administration, and the duration of protection is several months. ISG usually is given to travelers to regions of the world where there are high rates of hepatitis A infection and to close or household contacts of patients with hepatitis A infection. ISG is safe with few side effects.
Hepatitis A
Individuals at increased risk of acquiring hepatitis A are:
Some local health authorities or private companies may require hepatitis A vaccination for food handlers.
Hepatitis B
Hepatitis B vaccine is recommended for:
What Are The Symptoms And Signs Of Viral Hepatitis
The period of time between exposure to hepatitis and the onset of the illness is called the incubation period. The incubation period varies depending on the specific hepatitis virus. Hepatitis A virus has an incubation period of about 15 to 45 days Hepatitis B virus from 45 to 160 days, and Hepatitis C virus from about 2 weeks to 6 months.
Many patients infected with HAV, HBV, and HCV have few or no symptoms of illness. For those who do develop symptoms of viral hepatitis, the most common are flu-like symptoms including:
Viral Hepatitis Definition And Overview
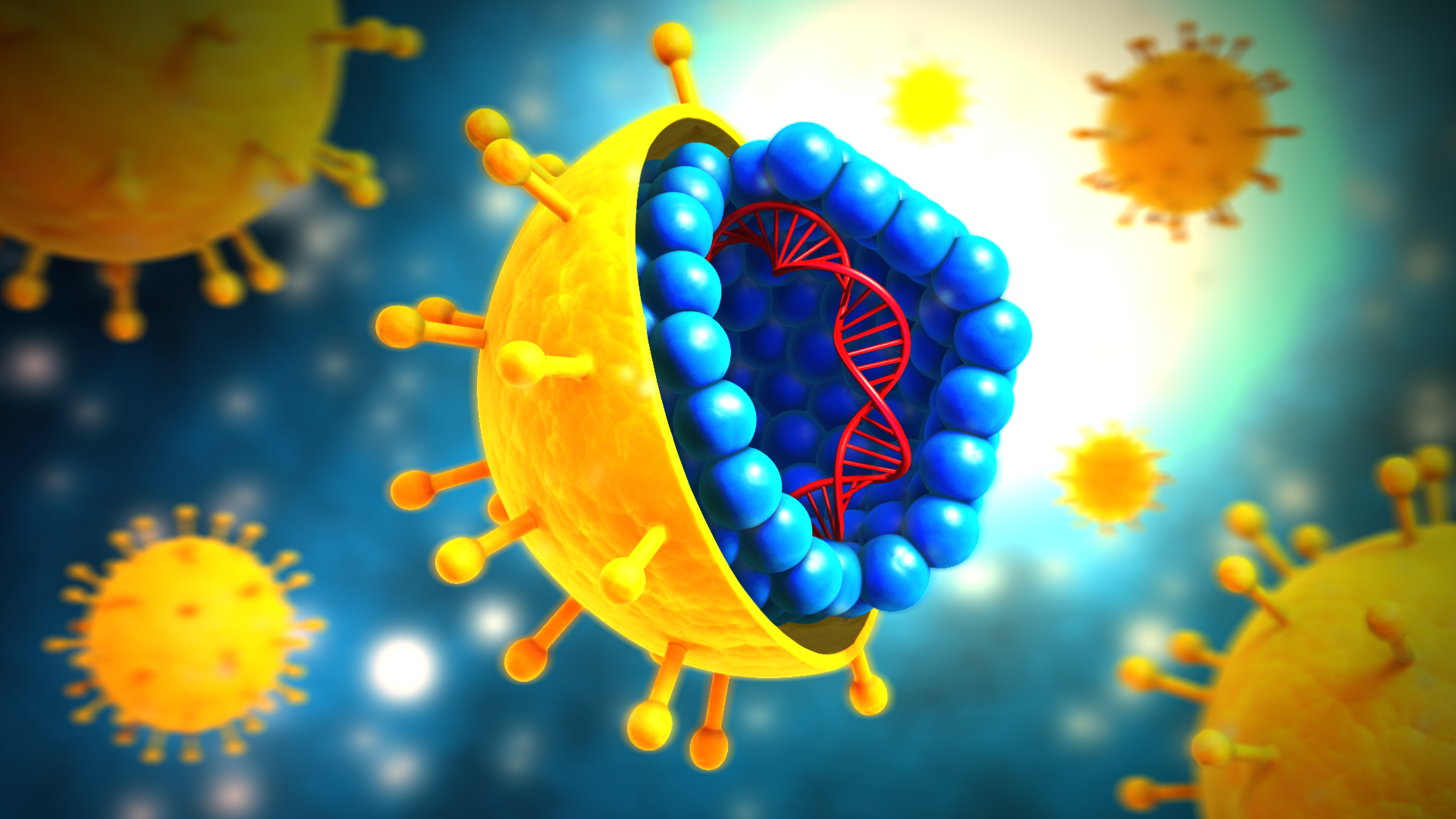
Hepatitis means inflammation of the liver. Many illnesses and conditions can cause inflammation of the liver, for example, drugs, alcohol, chemicals, and autoimmune diseases. Many viruses, for example, the virus causing mononucleosis and the cytomegalovirus, can inflame the liver. Most viruses, however, do not attack primarily the liver the liver is just one of several organs that the viruses affect. When most doctors speak of viral hepatitis, they are using the definition that means hepatitis caused by a few specific viruses that primarily attack the liver and are responsible for about half of all human hepatitis. There are several hepatitis viruses they have been named types A, B, C, D, E, F , and G. As our knowledge of hepatitis viruses grows, it is likely that this alphabetical list will become longer. The most common hepatitis viruses are types A, B, and C. Reference to the hepatitis viruses often occurs in an abbreviated form The focus of this article is on these viruses that cause the majority of human viral hepatitis.
Hepatitis viruses replicate primarily in the liver cells. This can cause the liver to be unable to perform its functions. The following is a list of major functions of the liver:
Don’t Miss: Hepatitis B Is More Infectious Than Hiv
What Is Chronic Hepatitis
Hepatitis is an inflammation of the liver. In chronic hepatitis, liver inflammation continues for at least six months. This condition may be mild, causing relatively little damage, or more serious, causing many liver cells to be destroyed. Some cases lead to cirrhosis and liver failure.
Chronic hepatitis from infection is most often caused by these viruses:
- Hepatitis B and C. Often the person infected is unaware of any initial symptoms. Or the symptoms were so mild that the person did not seek medical attention. This is especially true for chronic hepatitis C. Over time, perhaps a decade or more, both types may lead to the serious complication of cirrhosis due to ongoing destruction of liver cells and resultant scarring. A minority of patients with cirrhosis develop liver cancer over time.
- Hepatitis D. Hepatitis D infects only patients already infected with hepatitis B, and it generally results in a flare of active hepatitis.
This information helps to determine the best treatment and to assess your risk of developing cirrhosis and liver failure. A liver biopsy also can help to check for other disorders, such as alcoholic liver injury or fatty liver.
How Is Hepatitis C Spread

Hepatitis C spreads through contact with the blood of someone who has HCV. This contact may be through
- Sharing drug needles or other drug materials with someone who has HCV. In the United States, this is the most common way that people get hepatitis C.
- Getting an accidental stick with a needle that was used on someone who has HCV. This can happen in health care settings.
- Being tattooed or pierced with tools or inks that were not sterilized after being used on someone who has HCV
- Having contact with the blood or open sores of someone who has HCV
- Sharing personal care items that may have come in contact with another person’s blood, such as razors or toothbrushes
- Being born to a mother with HCV
- Having unprotected sex with someone who has HCV
Before 1992, hepatitis C was also commonly spread through blood transfusions and organ transplants. Since then, there has been routine testing of the U.S. blood supply for HCV. It is now very rare for someone to get HCV this way.
Read Also: Hepatitis C And Liver Disease
Acute Hepatitis C Vs Chronic Hepatitis C
Acute and chronic hepatitis C are caused by the same virus.
Acute hepatitis C develops after initial infection with the HCV. This stage can last up to 6 months. Many people have no symptoms during the acute stage and never find out that they have the infection.
According to the CDC, of people with acute hepatitis C develop chronic hepatitis C.
The World Health Organization states that 15 to 45 percent of people with acute hepatitis C spontaneously clear the virus within 6 months. This means that the virus goes away even though it hasnt been treated.
The 55 to 85 percent of people who dont clear the virus will develop a chronic HCV infection.
Chronic hepatitis C can be managed with medications and even cured, but its still a serious condition. According to the CDC,
How Do Doctors Treat Hepatitis C
Doctors treat hepatitis C with antiviral medicines that attack the virus and can cure the disease in most cases.
Several newer medicines, called direct-acting antiviral medicines, have been approved to treat hepatitis C since 2013. Studies show that these medicines can cure chronic hepatitis C in most people with this disease. These medicines can also cure acute hepatitis C. In some cases, doctors recommend waiting to see if an acute infection becomes chronic before starting treatment.
Your doctor may prescribe one or more of these newer, direct-acting antiviral medicines to treat hepatitis C:
You may need to take medicines for 8 to 24 weeks to cure hepatitis C. Your doctor will prescribe medicines and recommend a length of treatment based on
- which hepatitis C genotype you have
- how much liver damage you have
- whether you have been treated for hepatitis C in the past
Your doctor may order blood tests during and after your treatment. Blood tests can show whether the treatment is working. Hepatitis C medicines cure the infection in most people who complete treatment.
Hepatitis C medicines may cause side effects. Talk with your doctor about the side effects of treatment. Check with your doctor before taking any other prescription or over-the-counter medicines.
For safety reasons, talk with your doctor before using dietary supplements, such as vitamins, or any complementary or alternative medicines or medical practices.
You May Like: How Contagious Is Hepatitis C
Chronic Hepatitis B And Chronic Hepatitis C
CVH infections remain a major global public health concern. The number of people infected with both HBV and HCV are more than 240 and 70 million, respectively. The persistence of both viruses within infected hepatocytes always results in the development of liver fibrosis, cirrhosis, and HCC. Although HCV infection usually results in a vigorous activation of the innate immune system, the clinical symptoms of acute infection mostly go unnoticed and rather often subclinical.14 Nevertheless, HCV hepatitis induces attention deficits, chills, fatigue, malaise, sleep disturbances, irritability, numbness, and headaches with high impact on quality of life.15 In contrast, the accompanying symptoms of the acute HBV infection make it easily detectable.14 In general, both HBV and HCV infections remain a major issue in global health. Some of the clinical manifestations of HBV and HCV infections include acute hepatitis and various forms of chronic pathologies such as chronic hepatitis, cirrhosis, and HCC.3 In a clinical study involving HCC and liver cirrhosis patients, the administration of Korean red Ginseng extract induced a significant improvement in liver function tests with a significant decrease in both the tumor marker levels and viral titers in HCV patients.3,16
Stephen N.J. Korsman MMed FCPath, … Wolfgang Preiser MRCPath, in, 2012
Who Should Be Vaccinated
Children
- All children aged 1223 months
- All children and adolescents 218 years of age who have not previously received hepatitis A vaccine
People at increased risk for hepatitis A
- International travelers
- Men who have sex with men
- People who use or inject drugs
- People with occupational risk for exposure
- People who anticipate close personal contact with an international adoptee
- People experiencing homelessness
People at increased risk for severe disease from hepatitis A infection
- People with chronic liver disease, including hepatitis B and hepatitis C
- People with HIV
Other people recommended for vaccination
- Pregnant women at risk for hepatitis A or risk for severe outcome from hepatitis A infection
Any person who requests vaccination
There is no vaccine available for hepatitis C.
Also Check: Treatment To Cure Hepatitis C
Viral Hepatitis: Chronic Hepatitis C
Editors:Ozaras, Resat, Salmon-Ceron, Dominique
- Provides up-to-date information on epidemiology, diagnosis, treatment, and management of co-infections in chronic hepatitis C
- Features comprehensive and consistent coverage of topics
- International in scope in terms of both authorship and appeal
-
- ebooks can be used on all reading devices
- Immediate eBook download after purchase
- Softcover 93,59
-
- Free shipping for individuals worldwide
- Institutional customers should get in touch with their account manager
- Usually ready to be dispatched within 3 to 5 business days, if in stock
- The final prices may differ from the prices shown due to specifics of VAT rules
-
-
Global Epidemiology of Chronic Hepatitis C Virus Infection
Pages 1-24
-
Laboratory and Molecular Diagnosis of Hepatitis C and Resistance Testing
Pages 25-58
-
Pretherapeutic Evaluation of the Patients with HCV Infection
Pages 59-64
-
Current Therapy of Chronic Hepatitis C Virus in Treatment-Naive Patients
Pages 65-95
-
Treatment of Hepatitis C Virus-Infected Patients with Renal Failure
Pages 97-107
-
Treatment of Hepatitis C Virus in Special Populations
Pages 109-139
-
Management of Interferon-Free Direct-Acting HCV Antiviral Therapy Failure
Pages 159-165
-
Management of HCV Infection in Decompensated Cirrhosis in the Transplantation Setting
Pages 167-182
-
Extrahepatic Manifestations of Hepatitis C Virus Infection
Pages 183-195
-
Chronic Phase Of Hepatitis C
After six months 70% to 85% of those infected will have failed to clear the virus spontaneously. After this period the hepatitis C virus enters what is known as the chronic phase. This is when hepatitis C becomes a chronic or long-term infection. The diagnosis is confirmed when over a six month period hepatitis C RNA viral presence is detectable on at least two occasions.
A diagnosis of chronic hepatitis C means the battle between the virus and the immune system that occurs during the acute stage has finally been won by the virus. It is now highly unlikely that the virus can be cleared without treatment.
How the disease then progresses varies significantly from person to person. After many years some people will have minimal liver damage with no scarring while others can progress to cirrhosis within less than ten years. On average it takes about twenty years for significant liver scarring to develop. It is still not known whether chronic hepatitis C infection inevitably leads to cirrhosis. At present it is thought that this is a very likely outcome, although for some people it may take at least 50 years or more. They may well die of other unrelated diseases or conditions before cirrhosis develops. The rate of progression of liver damage cannot be accurately determined by liver enzyme levels, viral load or by genotype.
Liver damage and fibrosis during the chronic stage
Free Radicals and Fibrosis
Don’t Miss: What Is A Hepatitis Panel
Who Should Be Tested
Testing for hepatitis A is not routinely recommended.
CDC recommends hepatitis B testing for:
- Men who have sex with men
- People who inject drugs
- Household and sexual contacts of people with hepatitis B
- People requiring immunosuppressive therapy
- People with end-stage renal disease
- People with hepatitis C
- People with elevated ALT levels
- Pregnant women
- Infants born to HBV-infected mothers
CDC recommends hepatitis C testing for:
- All adults aged 18 years and older
- All pregnant women during each pregnancy
- About 24,900 new infections each year
- About 22,600 new infections in 2018
- Estimated 862,000 people living with hepatitis B
- About 50,300 new infections in 2018
- Estimated 2.4 million people living with hepatitis C
Getting Tested For Hepatitis C
Seek medical advice if you have persistent symptoms of hepatitis C or there’s a risk you’re infected, even if you do not have any symptoms.
A blood test can be carried out to see if you have the infection.
GPs, sexual health clinics, genitourinary medicine clinics or drug treatment services all offer testing for hepatitis C.
Early diagnosis and treatment can help prevent or limit any damage to your liver, as well as help ensure the infection is not passed on to other people.
Recommended Reading: Can Hepatitis C Spread Through Saliva
Interpreting Hcv Rna Test Results
It is essential that the provider understands how to interpret HCV RNA test results, especially during the course of HCV treatment.
| Result of HCV RNA Test | Interpretation |
|---|---|
| A quantified viral load — any exact number | Ongoing HCV infection |
| “Detected” | The HCV RNA is detectable but the number of international units is so low that it cannot be quantified accurately. This indicates extremely low level of virus is present. |
| “< 12 IU/mL” or “< 15 IU/mL” or “< 25 IU/mL” All of these are “less than the LLOQ” | HCV RNA is undetectable. No virus is detected at all in the patient’s serum specimen. |
Enzyme Immunoassays For Detection Of Hepatitis C Antibody
The HCV Ab test is used for initial screening for hepatitis C. The test is performed by enzyme immunoassays , which detect the presence of hepatitis C antibodies in serum. The result of the test is reported as positive or negative. Third-generation EIAs have a sensitivity/specificity of approximately 99%. However, the presence of HCV Ab does not indicate whether the infection is acute, chronic, or resolved. A positive antibody test result should be followed up with an HCV RNA test to confirm that viremia is present.
Don’t Miss: How To Get Rid Of Hepatitis C
What Is Viral Hepatitis
Hepatitis means inflammation of the liver. The liver is a vital organ that processes nutrients, filters the blood, and fights infections. When the liver is inflamed or damaged, its function can be affected. Heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by a virus. In the United States, the most common types of viral hepatitis are hepatitis A, hepatitis B, and hepatitis C.
How Serious Is It
- People can be sick for a few weeks to a few months
- Most recover with no lasting liver damage
- Although very rare, death can occur
- 15%25% of chronically infected people develop chronic liver disease, including cirrhosis, liver failure, or liver cancer
- More than 50% of people who get infected with the hepatitis C virus develop a chronic infection
- 5%-25% of people with chronic hepatitis C develop cirrhosis over 1020 years
Read Also: Hepatitis B Vaccine Side Effects
Stages Of Hepatitis C
The hepatitis C virus affects people in different ways and has several stages:
- Incubation period. This is the time between first exposure to the start of the disease. It can last anywhere from 14 to 80 days, but the average is 45
- Acute hepatitis C. This is a short-term illness that lasts for the first 6 months after the virus enters your body. After that, some people who have it will get rid of, or clear, the virus on their own.
- Chronic hepatitis C. For most people who get hepatitis C — up to 85% — the illness moves into a long-lasting stage . This is called a chronic hepatitis C infection and can lead to serious health problems like liver cancer or cirrhosis.
- Cirrhosis. This disease leads to inflammation that, over time, replaces your healthy liver cells with scar tissue. It usually takes about 20 to 30 years for this to happen, though it can be faster if you drink alcohol or have HIV.
- Liver cancer. Cirrhosis makes liver cancer more likely. Your doctor will make sure you get regular tests because there are usually no symptoms in the early stages.
Learn more about the stages and progression of hepatitis C.
Criteria To Distinguish A New Case From An Existing Case
All jurisdictions are encouraged to track negative HCV viral detection tests to document both spontaneous clearance of infection or sustained viral response to HCV treatment. Cases that have evidence of having cleared the infection at time of initial report or are considered false positive should not be reported to CDC.
If evidence indicating resolution of infection is received after a confirmed chronic case has been reported to CDC, the case report does not need to be modified as it was a confirmed case at the time of initial report. However, negative HCV viral detection test results received on confirmed chronic cases, subsequent to an initial positive result, should be appended to case reports, as feasible, and considered for the purpose of data analysis by each jurisdiction.
For probable chronic cases, the presence of a negative HCV viral detection test result, in the absence of criteria that would allow for confirmation, indicates that a case should not be classified as probable chronic and should not be reported to CDC.
A new chronic case is a newly reported case that does not have evidence of being an acute case of HCV infection. A confirmed acute case may be classified as a confirmed chronic case if a positive HCV viral detection test is reported one year or longer after acute case onset. A confirmed acute case may not be reported as a probable chronic case . For purposes of incidence and prevalence calculations, confirmed chronic HCV cases should be counted.
Also Check: Hepatitis A Vaccine At Cvs