Why Is Hepa Recommended
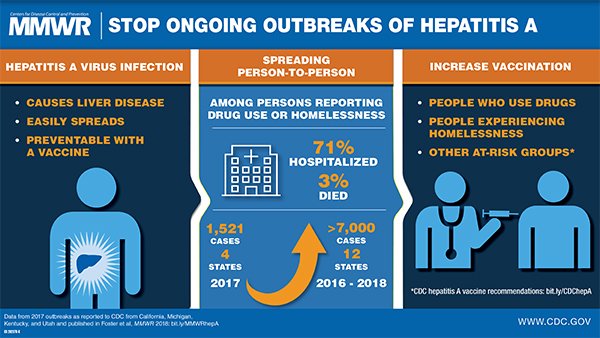
The HepA vaccine not only protects the kids who get it. It also can help prevent outbreaks. An outbreak is when a disease happens in greater numbers than expected in a particular area.
Childcare centers are a common site of hepatitis A outbreaks. Some kids can be infected and not have symptoms. But they can still spread the virus to others. Having many young kids vaccinated against hepatitis A can stop it from spreading in a community.
Who Is More Likely To Get Hepatitis A
People more likely to get hepatitis A are those who
- travel to developing countries
- have sex with an infected person
- are men who have sex with men
- use illegal drugs, including drugs that are not injected
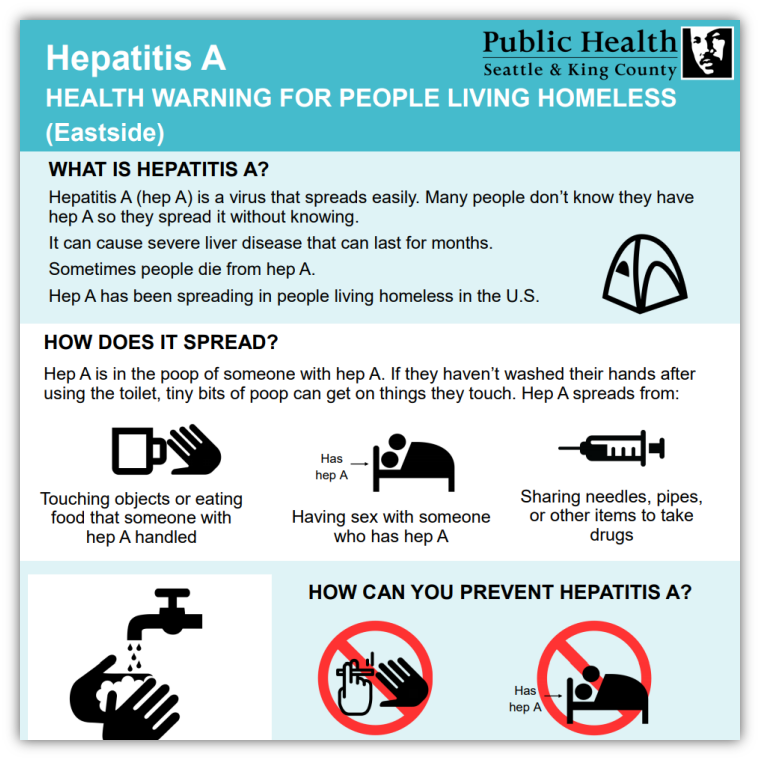
- experience unstable housing or homelessness
- live with or care for someone who has hepatitis A
- live with or care for a child recently adopted from a country where hepatitis A is common
Who Should Get Immunised Against Hepatitis A
Anyone who wants to protect themselves against hepatitis A can talk to their doctor about getting immunised.
Hepatitis A immunisation is recommended for:
- Aboriginal and Torres Strait Islander children who live in Queensland, the Northern Territory, Western Australia or South Australia, at 18 months and 4 years for free under the National Immunisation Program
- People who regularly provide care for Aboriginal and Torres Strait Islander children in Queensland, the Northern Territory, Western Australia or South Australia
- children at least 12 months old and adults who are travelling to areas where hepatitis A is common
- people who live or work with rural or remote Aboriginal and Torres Strait Islander communities
- people who work in early childhood education and care
- people with developmental disabilities, and their carers
- plumbers and sewage workers
Your doctor can tell you which vaccine they will use for your hepatitis A immunisation.
Also Check: Purina Pro Plan Hepatic Cat
Is Hepatitis A Vaccine Safe To Take If I’m Pregnant Or Breastfeeding
There are no adequate or well-controlled trials of hepatitis A vaccine use in pregnant women. Therefore, hepatitis A vaccine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
It is not known if the hepatitis A vaccine is excreted into human milk after administration to the mother. The manufacturer recommends caution when given it to nursing mothers.
What Are The Possible Side Effects Of Hepatitis A Immunisation
All medicines and vaccines can have side effects. Sometimes they are serious, most of the time theyre not.
For most people, the chance of having a serious side effect from a vaccine is much lower than the chance of serious harm if you caught the disease.
Talk to your doctor about possible side effects of hepatitis A vaccines, or if you or your child have possible side effects that worry you.
Common side effects of hepatitis A vaccines include:
- headache
- tiredness
- pain where the needle went in.
Also Check: Hepatitis C Treatment Guidelines 2017
Twinrix: The Vaccine For Hepatitis A And B
Both hepatitis A and B are identified by obtaining a blood sample, which you submit to a laboratory test. This test decides whether you have antibodies in the blood unique to those viruses. If the result is positive, you have been subjected to either hepatitis A or B.
To check whether anyone has hepatitis B, the test will see whether the individual has certain hepatitis B antigen levels.
What Causes Hepatitis A
The hepatitis A virus causes this type of hepatitis and spreads through contact with an infected persons stool. Contact can occur by
- eating food made by an infected person who did not wash his or her hands after using the bathroom
- drinking untreated water or eating food washed in untreated water
- placing a finger or an object in your mouth that came into contact with an infected persons stool
- having close personal contact with an infected person, such as through sex or caring for someone who is ill
You cannot get hepatitis A from
- being coughed on or sneezed on by an infected person
- sitting next to an infected person
- hugging an infected person
A baby cannot get hepatitis A from breast milk.4
Don’t Miss: Hepatitis C Ab W Reflex Hcv Rna Quant Rt Pcr
How Do Doctors Diagnose Hepatitis A
Doctors diagnose hepatitis A based on symptoms and a blood test. A health care professional will take a blood sample from you and send the sample to a lab. A blood test will detect antibodies to the hepatitis A virus called immunoglobulin M antibodies and show whether you have acute hepatitis A. If the blood test finds antibodies to the hepatitis A virus that are not IgM antibodies, then you are immune to hepatitis A, due to either past hepatitis A infection or hepatitis A vaccination.
Hepatitis A And B: Diseases Of The Liver
Hepatitis is an inflammation of the liver, most often caused by a viral infection. There are three common types of hepatitis caused by viruses: hepatitis A, hepatitis B, and hepatitis C. Vaccines have been developed that protect people from contracting hepatitis A and B. There is no vaccine for hepatitis C.
Hepatitis A and hepatitis B can be spread from person to person, although in different ways. They have similar symptoms, which include abdominal pain, fever, fatigue, joint pain, and jaundice .
Over the last 20 years, there has been a 90% decrease in cases of hepatitis A and an 80% decrease in hepatitis B cases in the U.S. Health experts believe that immunization efforts have led to this drop in rates of infection.
Read Also: How Is Hepatitis A Caused
Who Should Not Receive Hepatitis A Vaccine
There are a very few situations where the hepatitis A vaccine is not recommended. They include:
- If you have an illness causing a high temperature. In this situation, it is best to postpone vaccination until after you have fully recovered from the illness.
- If you have had an allergic reaction to the vaccine or to any of its components in the past.
- One type of vaccine should not be given to anyone who is known to be allergic to eggs.
- Children under the age of 1 year. However, the risk of hepatitis A in children under the age of 1 year is very low. The hepatitis A vaccine is not licensed for this age group.
The vaccine may be given if you are pregnant or breastfeeding and vaccination against hepatitis A is thought to be necessary.
Treatment And Manifestation Of Hepatitis A And B
Hepatitis A has an incubation time of two to six weeks. Hepatitis B only manifests after two to six months. Often patients with hepatitis A and B infection have moderate to no signs of the infection.
In persons who show symptoms, they will get flu-like symptoms, which will occur about three to ten days before symptoms of the liver develop.
Thereafter, the urine will darken, and jaundice may grow. With jaundice, the skin and the whites of a person’s eyes have a yellow hue. The inflamed liver cannot conduct its normal biochemical processes, so a material called bilirubin increases in the body.
Typically, you tend to feel healthy when you have jaundice, even though you keep looking worse.
In hepatitis A the jaundice stage only lasts for about one week. After that, you’ll continue to heal and usually feel like your usual self within a month. You are immune for life after recovering from hepatitis A.
In hepatitis B, the jaundice stage is about two weeks.
Don’t Miss: Where To Get A Hepatitis B Shot
Why Was The Hepatitis A Vaccine Recommended For All Children 2 To 18 Years Old After It Was Given To Only Certain Groups At First
When the hepatitis A vaccine first became available in the United States, it was only recommended for specific people who were at increased risk of getting hepatitis A. However, in 2006 the recommendation was extended to include all infants between 12 months and 23 months of age. The recommendation was updated again in 2020 to include vaccination of all children between 2 and 18 years of age who were not previously vaccinated against hepatitis A.
- Originally, the vaccine could only be given to children 2 years of age or older. In 2006, following additional studies, use of the vaccine was expanded to include infants between 12 months and 23 months of age.
- Disease rates had been controlled in parts of the country where the vaccine was recommended, yet cases of hepatitis A were still occurring, particularly in regions where children were not regularly getting the vaccine. So, the recommendation was expanded to protect children in all parts of the country.
Hepatitis A In Other Countries
Hepatitis A occurs worldwide. Developing countries with poor hygiene measures are at higher risk of hepatitis A infection and transmission.
In areas of high endemicity, such as parts of Africa, Asia, Central America and South America, up to 90% of children have been infected with hepatitis A.2
Hepatitis A is commonly reported in foodborne outbreaks.
Inactivated hepatitis A vaccines are prepared from hepatitis A virus harvested from human diploid cell cultures.
Different strains of HAV are in different vaccines, but there is only 1 known serotype. Immunity induced by a particular strain probably protects against all strains. 7
Recommended Reading: What Is Hepatic Flexure Cancer
The Above Policy Is Based On The Following References:
Hepatitis A Prevention In Virginia
In Virginia, local health departments, in conjunction with community partners, are working to prevent hepatitis A from spreading throughout the Commonwealth. Beginning in January 2019, a statewide hepatitis A vaccination campaign will focus on increasing the number of Virginians properly immunized for hepatitis A.
The vaccination campaign will focus specifically on individuals who are members of high risk groups such as those who are/have recently been incarcerated, persons who are experiencing homelessness, injection and non-injection drug users, and men who have sex with men . Although the campaigns focus is on those who at higher risk for hepatitis A infection, any Virginian who desires hepatitis A vaccine should receive the vaccine.
To learn more about Virginia’s Hepatitis A Prevention Campaign, click HERE.
Don’t Miss: Where Can I Get Hepatitis B Vaccine
Do I Need To Pay For Hepatitis A Immunisation
Vaccines covered by the NIP are free for people who are eligible. See the NIP Schedule to find out which vaccines you or your family are eligible to receive.
Eligible people get the vaccine for free, but your health care provider may charge a consultation fee for the visit. You can check this when you make your appointment.
If you are not eligible for free vaccine, you may need to pay for it. The cost depends on the type of vaccine, the formula and where you buy it from. Your immunisation provider can give you more information.
Should I Get The Hepatitis A Vaccine
Hepatitis A
Hepatitis A vaccination is recommended for:
- Travelers to countries that have high rates of hepatitis A
- Family members or caregivers of a recent adoptee from countries where hepatitis A is common
- Men who have sex with men
- People who use injection and non-injection drugs
- People with chronic liver diseases, such as hepatitis B or hepatitis C
- People who are teated with clotting-factor concentrates
- People who work with hepatitis A infected animals or in a hepatitis A research laboratory
- People who are experiencing homelessness
- People age 40 and older at increased risk for hepatitis A infection, or who are at increased risk for severe disease from hepatitis A infection who also have other risk factors
- People age 19 or older at increased risk for hepatitis A infection, or who are at increased risk for severe disease from hepatitis A infection who also have other risk factors
Health care providers recommend that all children receive a hepatitis A vaccination at around 1 year of age, but many adults have never received the vaccine because it only became available in 1995.
Health care personnel and patients with the following conditions should discuss the hepatitis A vaccination with their health care provider: pregnancy, immunocompromising conditions, HIV infection, heart disease, chronic lung disease, chronic alcoholism, asplenia, kidney failure.
You should NOT get the hepatitis A vaccination or you should wait, if you:
Recommended Reading: Hepatitis C Antibody Negative Means
How Can You Avoid Catching Hepatitis A Virus When Traveling
Anyone traveling to countries where hepatitis A virus infections are common should avoid the following:
- Ice and unbottled water
- Uncooked or unpeeled vegetables and fruit
- Food from street vendors
- Salads
Vaccination at least 2 weeks before travel is generally also recommended. Additional travel information is available in the CDC travel publication, Yellow Book.
Where To Find Hepatitis A Vaccine
Hepatitis A vaccine is available at a variety of locations across Virginia. Many doctor’s offices and pharmacies carry the vaccine and it is also available at local health departments across the state.
All images courtesy of the Centers for Disease Control.
Recommended Reading: Can You Die With Hepatitis C
Who Should Not Get The Hepatitis A & B Vaccine
- Anyone with a life-threatening allergy to any vaccine component should not get the vaccine. Tell your healthcare provider if you have any severe allergies.
- Anyone who has ever had a life-threatening allergic reaction to a previous dose of the hepatitis A and B combination vaccine should not get another dose.
- Anyone who is moderately ill should wait until they recover.
- Tell your healthcare provider if you are pregnant.
How Does One Administer Twinrix
Twinrix is given by injecting the liquid into the muscles. How many Twinrix shots do I need? It is provided as a sequence of three dosages. With the second dose given at least one month after the first. The final and third dose given at least six months after the first dosage.
A 4-dose rapid schedule is also accessible for individuals 19 years of age and over. It is safe to receive the hepatitis A and B vaccination in conjunction with other vaccines.
Read Also: What Is Hepatitis A And B And C
Talk With Your Health Care Provider
Tell your vaccine provider if the person getting the vaccine:
- Has had an allergic reaction after a previous dose of hepatitis A vaccine, or has any severe, life-threatening allergies.
In some cases, your health care provider may decide to postpone hepatitis A vaccination to a future visit.
People with minor illnesses, such as a cold, may be vaccinated. People who are moderately or severely ill should usually wait until they recover before getting hepatitis A vaccine.
Your health care provider can give you more information.
Persons New To Canada
Health care providers who see persons newly arrived in Canada should review the immunization status and update immunization for these individuals, as necessary. In many countries outside of Canada, HB vaccine is in limited use.
All persons from a country that is endemic for HB should be assessed and vaccinated against HB if not immune and not infected. Individuals born in developing countries are more likely to be carriers of HB, necessitating vaccination of their sexual and household contacts based on review of their serologic test results. HB vaccine is recommended for all household contacts whose families have immigrated to Canada from areas in which there is a high prevalence of HB and who may be exposed to HB carriers through their extended families or when visiting their country of origin.
Children adopted from countries in which there is a high prevalence of HB infection should be screened for HBsAg and, if positive, household or close contacts in the adopting family should be immunized before adoption or as soon as possible thereafter. Adults going to pick-up children from these countries should be vaccinated before departure. Refer to Immunization of Persons New to Canada in Part 3 for additional information.
Read Also: How Do I Know If I Have Hepatitis B
Persons With Chronic Diseases
Refer to Immunization of Persons with Chronic Diseases in Part 3 for additional general information about vaccination of people with chronic diseases.
Chronic renal disease and patients on dialysis
People with chronic renal disease may respond sub-optimally to HB vaccine and experience more rapid decline of anti-HBs titres, and are therefore recommended immunization with a higher vaccine dose. Individuals undergoing chronic dialysis are also at increased risk for HB infection. In people with chronic renal disease anti-HBs titre should be evaluated annually and booster doses using a higher vaccine dose should be given as necessary.
Neurologic disorders
People with conditions such as autism spectrum disorders or demyelinating disorders should receive all routinely recommended immunizations, including HB-containing vaccine.
Chronic liver disease
HB immunization is recommended for non-immune persons with chronic liver disease, including those infected with hepatitis C, because they are at risk of more severe disease if infection occurs. Vaccination should be completed early in the course of the disease, as the immune response to vaccine is suboptimal in advanced liver disease. Post-immunization serologic testing may be used to confirm vaccine response.
Non-malignant hematologic disorders
Persons with bleeding disorders and other people receiving repeated infusions of blood or blood products are considered to be at higher risk of contracting HB and should be offered HB vaccine.