Hepatitis B In The United States
In the United States, about 862,000 people have chronic hepatitis B.6 Asian Americans and African Americans have higher rates of chronic hepatitis B than other U.S. racial and ethnic groups.10 Researchers estimate that about half of the people living with chronic hepatitis B in the United States are Asian Americans and Pacific Islanders.11 Chronic hepatitis B is also more common among people born in other countries than among those born in the United States.7
The hepatitis B vaccine has been available since the 1980s and, in 1991, doctors began recommending that children in the United States receive the hepatitis B vaccine. The annual rate of acute hepatitis B infections went down 88.5 percent between 1982 and 2015.12 In 2017, the annual number of hepatitis B infections rose in some states.13 Experts think the rise was related to increases in injection drug use. Injection drug use increases the risk of hepatitis B infection.
Natural History Of Hepatitis Co
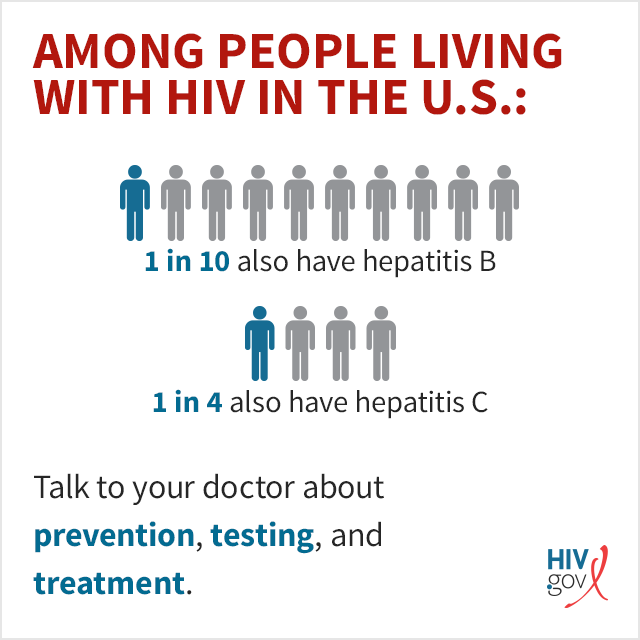
HBV and HIV
Approximately 350 million people worldwide are infected by HBV. In general, HBV is not directly cytopathic. Damage to hepatocytes is related to host immunological activity against HBV inside the hepatocytes. Among Asian patients who acquire the infection at infancy, the natural history of chronic HBV is divided into three phases. In the immune tolerance phase, there is little host immune response to HBV. This usually occurs during childhood and teenage. The liver enzymes are normal despite high HBV DNA level and positive hepatitis B e-antigen . The immune clearance phase occurs in early adulthood when host immunity starts to clear HBV-infected hepatocytes. This is reflected by elevated liver enzymes and fluctuating HBV DNA. Successful viral suppression is manifested as HBeAg-seroconversion and undetectable HBV DNA. These fortunate individuals would then enter the quiescent phase and have good overall prognosis. In patients who fail to achieve successful viral suppression, chronic or intermittent inflammation of the liver parenchyma may result in cirrhosis and possibly hepatocellular carcinoma.
HCV and HIV
Genomic Structure And Organization
Morphologically, HIV is a single spherical particle with a diameter ranging from 90 to 120 nm. The virion has a spiky envelope and a dense nucleocapsid, sometimes trapezoidal or bar-shaped.
Structurally it is described as follows .
Figure 1.
HIV structure (from HIV genetic diversity and its consequences, .
The viral body comprises two identical RNA molecules three viral enzymes protease and integrase ] and three internal proteins .
The viral envelope, emanation of the cellular cytoplasmic membrane, carries two viral glycoproteins essential in the virus-host cell interaction. This is the gp41 and the gp120 .
HIV has gag, pol, and env as structural genes that encode internal proteins, viral enzymes, and envelope glycoproteins, respectively , and it has six regulatory genes: tat, rev, nef, alive, vpr, vpu , and vpx .
Figure 2.
Genomic organisation of HIV-1 and HIV-2 .
You May Like: New Drugs For Hepatitis B
Management Of Hepatitis Co
Initial assessment
Since HBV, HCV and HIV share common routes of transmission, initial assessment of an HIV infected patient should include a detailed history and physical examination looking for symptoms and signs of viral hepatitis and chronic liver disease. Liver function tests should be routinely checked together with viral serology including IgG anti-hepatitis A virus, HBsAg, anti-HBc and anti-HCV. Occult HBV and/or HCV infection is not uncommon in HIV-infected patients. If a patient has negative hepatitis serology but unexplained impairment in liver function, HBV DNA and HCV RNA should be checked as well.
In patients confirmed to have HBV-HIV or HCV-HIV co-infection, further assessment is necessary because the risk of advanced liver disease is increased. Complete blood count should be performed to look for thrombocytopaenia, and ultrasound scan should be arranged to rule out cirrhosis. Liver biopsy should be considered when a decision of treatment needs to be based on the severity of liver fibrosis. This is particularly important for genotype 1 HCV infection which is less likely associated with sustained virological response. Alpha-fetal protein should be performed every 6 months to screen for hepatocellular carcinoma. In patients confirmed to have liver cirrhosis, upper gastrointestinal endoscopy to screen for varices is recommended.
Hepatitis vaccinations
Prevalence Of Hiv In The World
In 2015, the number of HIV-related deaths ranged from 930,000 to 1,300,000 worldwide . According to Global AIDS in 2016, approximately, 37 million people live with HIV and 21 million are under treatment.
The distribution of HIV infection is not equitable in the world, sub-Saharan Africa is the most affected region. In 2015, it alone counted 25,600,000 people living with HIV or nearly 70% of the worlds PLHIV. The overall prevalence in this part of the world is 5.0% , with 1,900,000 new infections per year.
Also Check: Can You Die With Hepatitis C
Dealing With Spillages Of Body Fluids:
- Wear disposable gloves if possible.
- Use absorbent paper towels to cover the spillage.
- Pour diluted bleach on to the paper towels and leave it for at least 2 minutes before wiping up. Where it is not appropriate to use bleach , hot soapy water is a reasonable alternative.
- Waste disposal: small soiled items such as tissues and tampons can be flushed down the toilet. Larger items soiled with material which may be infected should be sealed securely in plastic bags and disposed of as clinical waste.
- Disposable gloves should be washed with soap and hot water to remove all traces of blood before they are removed and then disposed of. The hands should then be washed again.
- Clothing or linen soiled with blood or body fluids can be washed in the washing machine on a hot cycle.
Treatment For Chronic Hepatitis B Infection
Most people diagnosed with chronic hepatitis B infection need treatment for the rest of their lives. Treatment helps reduce the risk of liver disease and prevents you from passing the infection to others. Treatment for chronic hepatitis B may include:
- Antiviral medications. Several antiviral medications including entecavir , tenofovir , lamivudine , adefovir and telbivudine can help fight the virus and slow its ability to damage your liver. These drugs are taken by mouth. Talk to your doctor about which medication might be right for you.
- Interferon injections. Interferon alfa-2b is a man-made version of a substance produced by the body to fight infection. Itâs used mainly for young people with hepatitis B who wish to avoid long-term treatment or women who might want to get pregnant within a few years, after completing a finite course of therapy. Interferon should not be used during pregnancy. Side effects may include nausea, vomiting, difficulty breathing and depression.
- Liver transplant. If your liver has been severely damaged, a liver transplant may be an option. During a liver transplant, the surgeon removes your damaged liver and replaces it with a healthy liver. Most transplanted livers come from deceased donors, though a small number come from living donors who donate a portion of their livers.
Other drugs to treat hepatitis B are being developed.
You May Like: Is Hepatitis C And Herpes The Same Thing
You May Like: Hepatitis B Surface Antibody Interpretation
What Therapy To Start When Haart Does Not Need To Be Started
If HIV treatment is not initiated, anti-HBV treatment options are more limited due to the dual activity of many nucleoside analogs and the risk of developing drug-resistant HIV. The only current options are adefovir, peginterferon-alfa, and telbivudine. Of the three agents, telbivudine is the most potent, but it is limited by development of drug-resistant HBV in the monoinfected patient. Although telbivudine has not been studied in vivo in the setting of high levels of HIV RNA, in vitro evidence suggests that it is not active against HIV. In a single-round replication assay, telbivudine did not affect HIV replication . Peginterferon-alfa has the advantage that drug-resistant HBV will not emerge, so it is a reasonable option if the patient can tolerate the injections and the side effects. It is possible that a combination of one or more of these three agents may be effective in this situation, but it has not been studied. Thus, each of these approaches to anti-HBV therapy in HIV-infected individuals who do not receive concurrent HAART therapy is suboptimal. For these reasons, an additional option is to initiate HAART earlier than is required by HIV guidelines. Early initiation of HAART may be an increasingly attractive option, especially because HIV increases the rate of liver disease progression and earlier HIV treatment is now being advocated even in HIV monoinfection.
Effects Of Chronic Hepatitis On The Treatment Of Hiv Infection
Current data do not suggest that chronic hepatitis B or C affect the natural course of HIV infection. However, hepatotoxicity secondary to HIV treatment is more common among patients with chronic viral hepatitis, especially among females with high baseline CD4 counts. The incidence of hepatotoxicity secondary to HAART has been reported to be between 2-18% among the major series., Invariably, HBV or HCV is among the factors associated with drug-induced liver injury. Regular monitoring of liver function tests is required during HAART.
Furthermore, a number of drug interactions are noteworthy. For the treatment of HCV-HIV co-infection, ribavirin should not be used together with nucleoside reverse transcriptase inhibitors didanosine and stavudine because of the risk of mitochondrial toxicity. This may lead to acute pancreatitis, lactic acidosis, hepatic steatosis and liver failure. Zidovudine should be avoided during HCV treatment because it increases the risk of anaemia and neutropaenia. Subgroup analysis of one study showed that protease inhibitors may reduce the treatment efficacy of PEG-IFN and ribavirin in HCV-HIV co-infected patients, but this needs further confirmation.
Read Also: What Is Hepatitis C And What Are The Symptoms
Types Of Work Where There May Be Contact With Blood/body Fluids:
- Custodial services
- Tattooing, ear and body piercing
- Vehicle recovery and repair
Specific legislation on hazards that arise from working with biological agents such as BBVs is contained in the Control of Substances Hazardous to Health Regulations 1999 . Under COSHH you have a legal duty to assess the risk of infection for employees and others affected by your work.
What Is Viral Hepatitis
Hepatitis means inflammation of the liver. The liver is a vital organ that processes nutrients, filters the blood, and fights infections. When the liver is inflamed or damaged, its function can be affected. Heavy alcohol use, toxins, some medications, and certain medical conditions can cause hepatitis. However, hepatitis is often caused by a virus. In the United States, the most common types of viral hepatitis are hepatitis A, hepatitis B, and hepatitis C.
Donât Miss:Hepatitis B Symptoms In Females
Read Also: How To Tell If I Have Hepatitis
Other Body Fluids And Tissues
Synovial fluid , amniotic fluid, cerebrospinal fluid, and peritoneal fluid can contain the hepatitis B virus, but the risk of transmission to workers is not known.
Feces, nasal secretions, sputum, sweat, tears, urine, and vomit have not been implicated in the spread of hepatitis B. Unless they are visibly contaminated with blood, the risk of contracting hepatitis B from these fluids in the workplace is very low.
Hepatitis B is not transmitted by casual contact. For example, hospital employees who have no contact with blood, blood products, or blood-contaminated fluids are at no greater risk than the general public. However, the virus can spread through intimate contact with carriers in a household setting, possibly because of frequent physical contact with small cuts or skin rashes. The virus can also spread through biting and possibly by the sharing of toothbrushes or razors. It is not spread through sneezing, coughing, hand holding, hugging, kissing, breastfeeding, sharing eating utensils, water or food.
Whats The Hiv Window Period
As soon as someone contracts HIV, it starts to reproduce in their body. The persons immune system reacts to the antigens by producing antibodies .
The time between exposure to HIV and when it becomes detectable in the blood is called the HIV window period. Most people develop detectable HIV antibodies within 23 to 90 days after transmission.
If a person takes an HIV test during the window period, its likely theyll receive a negative result. However, they can still transmit the virus to others during this time.
If someone thinks they may have been exposed to HIV but tested negative during this time, they should repeat the test in a few months to confirm . And during that time, they need to use condoms or other barrier methods to prevent possibly spreading HIV.
Someone who tests negative during the window might benefit from post-exposure prophylaxis . This is medication taken after an exposure to prevent getting HIV.
PEP needs to be taken as soon as possible after the exposure it should be taken no later than 72 hours after exposure but ideally before then.
Another way to prevent getting HIV is pre-exposure prophylaxis . A combination of HIV drugs taken before potential exposure to HIV, PrEP can lower the risk of contracting or transmitting HIV when taken consistently.
Timing is important when testing for HIV.
Read Also: What Medicine Do You Take For Hepatitis C
Study Settings And Patients
A cross-sectional study involving 345 CLD patients was conducted between Dec. 2018 and Mar. 2019. The patients were recruited at the gastroenterology clinics of four selected referral hospitals , two specialized private health care institutions during routine clinical practices. The four Hospitals and Adera Medical Center are located in Addis Ababa, the capital of Ethiopia, whereas Yanet specialized clinic is found in Hawassa, in southern Ethiopia. The CLD patients were included in the study in two groups: HCC and non-HCC patients. The non-HCC groups comprised patients with advanced liver disease and chronic hepatitis .
Who Are Hepatitis B Carriers
Hepatitis B carriers are people who have the hepatitis B virus in their blood, even though they dont feel sick. Between 6% and 10% of those people whove been infected with the virus will become carriers and can infect others without knowing it. There are over 250 million people in the world who are carriers of HBV, with about 10% to 15% of the total located in India. Children are at the highest risk of becoming carriers. About 9 in 10 babies infected at birth become HBV carriers, and about half of children who are infected between birth and age 5 carry the virus. A blood test can tell you if you are a hepatitis B carrier.
Recommended Reading: Does Hepatitis B Have A Cure
Treatment Options For Hiv
Treatment should begin as soon as possible after a diagnosis of HIV, regardless of viral load.
The main treatment for HIV is antiretroviral therapy, a combination of daily medications that stop the virus from reproducing. This helps protect CD4 cells, keeping the immune system strong enough to take measures against disease.
Antiretroviral therapy helps keep HIV from progressing to AIDS. It also helps reduce the risk of transmitting HIV to others.
When treatment is effective, the viral load will be undetectable. The person still has HIV, but the virus is not visible in test results.
However, the virus is still in the body. And if that person stops taking antiretroviral therapy, the viral load will increase again, and the HIV can again start attacking CD4 cells.
Hepatitis B And Pregnancy
If youâre pregnant, you might pass the virus to your baby at birth. Itâs less likely to happen during your pregnancy.
If your baby gets the virus and isnât treated, they could have long-term liver problems. All newborns with infected mothers should get hepatitis B immune globulin and the vaccine for hepatitis at birth and during their first year of life.
Don’t Miss: Does Hepatitis C Weaken Your Immune System
What Are The Symptoms Of Chronic Hepatitis B
About 1 in 20 people who get hepatitis B as adults become carriers, which means they have a chronic hepatitis B infection. Carriers are more likely to pass hepatitis B to other people. Most carriers are contagious meaning they can spread hepatitis B for the rest of their lives.
Hepatitis B infections that last a long time may lead to serious liver diseases like cirrhosis and liver cancer. About 1 in 5 people with chronic hepatitis B die from it. There are medicines that can help treat chronic hepatitis B infections.
Most babies who get hepatitis B develop chronic infection, unless they get treated right away. But treatments almost always work if your baby gets them quickly. Thats why its important for pregnant people to get tested for hepatitis B.
Rash Related To Medication
While rash can be caused by HIV co-infections, it can also be caused by medication. Some drugs used to treat HIV or other conditions can cause a rash.
This type of rash usually appears within a week or 2 weeks of starting a new medication. Sometimes the rash will clear up on its own. If it doesnt, a change in medications may be needed.
Rash due to an allergic reaction to medication can be serious.
Other symptoms of an allergic reaction include:
- trouble breathing or swallowing
Stevens-Johnson syndrome is a rare allergic reaction to HIV medication. Symptoms include fever and swelling of the face and tongue. A blistering rash, which can involve the skin and mucous membranes, appears and spreads quickly.
When 30 percent of the skin is affected, its called toxic epidermal necrolysis, which is a life threatening condition. If this develops, emergency medical care is needed.
While rash can be linked with HIV or HIV medications, its important to keep in mind that rashes are common and can have many other causes.
Don’t Miss: Can You Get Hepatitis A From Sex
Approaches By Virus Life Cycle Stage
consist of a and sometimes a few stored in a capsule made of , and sometimes covered with a layer . Viruses cannot reproduce on their own and instead propagate by subjugating a host cell to produce copies of themselves, thus producing the next generation.
Researchers working on such ââ strategies for developing antivirals have tried to attack viruses at every stage of their life cycles. Some species of mushrooms have been found to contain multiple antiviral chemicals with similar synergistic effects.Compounds isolated from fruiting bodies and filtrates of various mushrooms have broad-spectrum antiviral activities, but successful production and availability of such compounds as frontline antiviral is a long way away. Viral life cycles vary in their precise details depending on the type of virus, but they all share a general pattern:
Before cell entry
This stage of viral replication can be inhibited in two ways:
Uncoating inhibitor
Inhibitors of uncoating have also been investigated.
During viral synthesis
Transcription