Barriers To Eliminating Hbv
Persistence of cccDNA and its ability to self-replenish and the lack of direct effects of current therapies on cccDNA account for the difficulty in eliminating cccDNA. There are additional barriers to eliminating HBV. HBV DNA can be integrated into the host genome. Although integrated HBV DNA is often rearranged and/or partially deleted and there is no evidence that it supports the full cycle of HBV replication, recent studies suggest that integrated HBV DNA can be sufficiently intact to support translation of viral proteins, e.g., HBsAg. Elimination of integrated HBV DNA will likely require the removal of hepatocytes that harbor these DNA. Control of infections generally requires elimination of the infectious organisms coupled with activation of specific immune responses. Whereas patients who recover from acute HBV infection display rigorous immune responses to multiple HBV epitopes, patients with chronic HBV infection manifest weak immune responses to very few HBV epitopes.
D Viral Resistance Testing
Hepatitis B antiviral drug resistance mutations in treatment-naïve patients are rare. For patients on antiviral therapy, the first manifestation of antiviral resistance is virological breakthrough, which is defined as a 1-log10 increase in serum HBV DNA from nadir during treatment in a patient who had an initial virological response. Most antiviral-resistant mutants have decreased replication fitness compared with wild-type HBV. However, compensatory mutations that can restore replication fitness frequently emerge during continued treatment, leading to a progressive increase in serum HBV DNA that may exceed pretreatment levels. Genotypic resistance, measured with commercially available assays, evaluate sequence variations in specific positions in the polymerase. The current diagnostic methods include restriction fragment length polymorphism analysis, hybridization, and sequencing. Current assays typically require an HBV-DNA level > 1,000 IU/mL.
Guidance Statements on Use of Selected Serological and Virological Assays
World Health Organization Recommendations
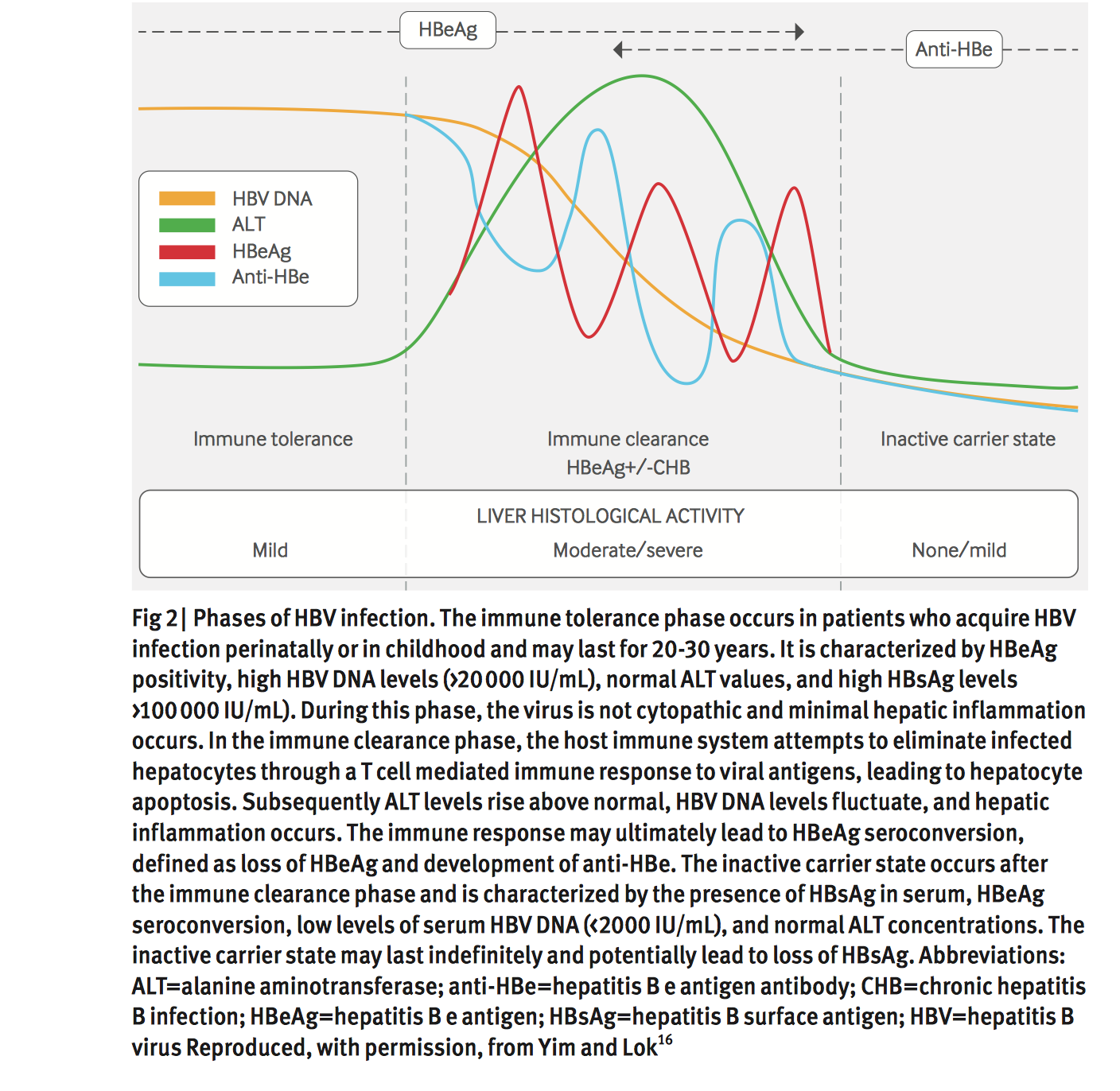
The 2015 WHO guidelines for the prevention, care, and treatment of persons with chronic hepatitis B infection indicates treatment priority for individuals of all ages who have chronic hepatitis B infection and clinical evidence of compensated/decompensated cirrhosis , regardless of their levels of ALT or HBV DNA, or their HBeAg status.
Treatment is recommended for adults with chronic hepatitis B infection without clinical evidence of cirrhosis , but who have all of the following features , and regardless of HBeAg status :
- Are older than 30 years
- Have persistently abnormal ALT levels
- Have evidence of high-level HBV replication .
In individuals with HBV/human immunodeficiency virus coinfection, the AASLD recommends initiating ART in all those with evidence of severe chronic liver disease, regardless of CD4 count, as well as those with a CD4 count of 500 cells/mm3 or below, regardless of their liver disease stage.
However, the AASLD does not recommend antiviral therapy, indicating it can be deferred, in individuals with all of the following , regardless of HBeAg status or age :
- No clinical evidence of cirrhosis
- Persistently normal ALT levels
- Low levels of HBV DNA replication . ]
Read Also: How Do You Get Hepatitis C Antibodies
Hepatitis B Causes And Risk Factors
Itâs caused by the hepatitis B virus, and it can spread from person to person in certain ways. You can spread the hepatitis B virus even if you donât feel sick.
The most common ways to get hepatitis B include:
- Sex. You can get it if you have unprotected sex with someone who has it and your partnerâs blood, saliva, semen, or vaginal secretions enter your body.
- Sharing needles. The virus spreads easily via needles and syringes contaminated with infected blood.
- Accidental needle sticks.Health care workers and anyone else who comes in contact with human blood can get it this way.
- Mother to child.Pregnant women with hepatitis B can pass it to their babies during childbirth. But thereâs a vaccine to prevent newborns from becoming infected.
Hepatitis B doesnât spread through kissing, food or water, shared utensils, coughing or sneezing, or through touch.
Prognosis Improvement After Hbsag Clearance
These related studies provide clear recommendations that patients who achieve HBsAg clearance have favourable clinical outcomes compared to patients who achieve only HBV DNA suppression and HBeAg seroconversion. HBsAg clearance leads to biochemical, virological and liver histological improvements, and it significantly reduces the risk of HCC. However, HCC may occur after HBsAg seroclearance despite it being the ultimate treatment endpoint recommended by current guidelines. The risk factors associated with HCC include the presence of cirrhosis, male sex, and age50 years at the time of HBsAg clearance . Closer attention should be given to patients with one or more of these risk factors.
These high-risk patients should be re-examined in a timely manner even if HBsAg clearance is obtained. These results also suggest that achieving a functional cure early in the absence of cirrhosis results in a better prognosis .
Also Check: How Do You Get Hepatitis A B C
American Association For The Study Of Liver Diseases Recommendations
The 2016 AASLD guidelines for the treatment of chronic hepatitis B as well as select recommendations from the 2018 AASLD guidance update on the prevention, diagnosis, and treatment of chronic hepatitis B are outlined below and in the Guidelines section.
Adults with immune-active chronic hepatitis B infection
Administer antiviral therapy to lower the risk of morbidity and mortality associated with chronic hepatitis B infection.
The recommended initial agent for adults is PEG-IFN, entecavir, or tenofovir.
Adults with immune-tolerant chronic hepatitis B infection
Antiviral therapy is not recommended.
The AASLD suggests obtaining ALT levels at least every 6 months to monitor for potential transition to immune-active or -inactive chronic hepatitis B.
For select patients older than 40 years, the AASLD suggests antiviral therapy in the setting of normal ALT levels, elevated HBV DNA , and significant necroinflammation or fibrosis on liver biopsy specimens.
Adults with HBeAg-positive immune-active chronic hepatitis B who seroconvert to anti-HBe on nucleoside analog therapy
After a period of treatment consolidation , consider discontinuing NA therapy in noncirrhotic HBeAg-positive adults who seroconvert to anti-HBe while on NA treatment. If antiviral therapy is stopped, monitor the patient every 3 months for a minimum of 1 year for recurrent viremia, ALT flares, seroreversion, and clinical decompensation.
Adults with HBeAg-negative immune-active chronic HBV infection
Inpatient care
B Hepatitis D Infection
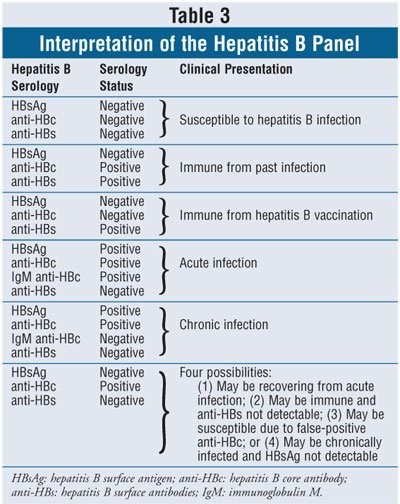
The AASLD 2016 HBV Guidelines recommend testing of HBsAg-positive persons at risk for HDV, including those with HIV infection, persons who inject drugs, men who have sex with men, and immigrants from areas of high HDV endemicity, . Additionally, HBsAg-positive patients with low or undetectable HBV DNA but high ALT levels should be considered for HDV testing. Given the importance of HDV to the long-term management of the HBsAg-positive patient, if there is any uncertainty regarding the need to test, HDV screening is recommended. The recommended screening test is anti-HDV, and if this test result is positive, it should be followed by HDV-RNA testing to diagnose active HDV infection. A high degree of heterogeneity in sensitivity and specificity has been identified across HDV assays, and the availability of the first international external quality control for HDV quantification by the World Health Organization has led to improvements in HDV diagnostics.
| ⢠Persons born in regions with reported high HDV endemicitya This list is incomplete, because many countries do not report HDV rates. |
|
Africa Asia Pacific Islands |
|
Lack access to entecavir or tenofovir |
Access to entecavir or tenofovir |
- Abbreviation: LT, liver transplant.
Guidance Statements for Treatment of Liver Transplant Recipients With Hepatitis B
HBIG monotherapy should not be used.
Also Check: Blood Donation Hepatitis B Antibodies
How Is It Transmitted
Hepatitis B is highly infectious, and is spread from one person to another through exposure to infected blood and body fluids . It can be spread through:
- blood transfusions or organ transplantation in countries where blood or blood products have not been properly screened for hepatitis B and other viruses transmitted through blood
- unprotected sex with an infected person
- sharing needles or equipment for injecting drugs
- unsterilized medical/dental equipment and shared/contaminated materials or equipment used for tattooing, body piercing or acupuncture
- sharing toothbrushes or razors
- childbirth
- household contact between family members
What Treatments Are Available For Chronic Hepatitis B If Medications Dont Work
If you have advanced hepatitis B, you might also become a candidate for a liver transplant. This path does not always result in a cure because the virus continues in your bloodstream after a transplant. To prevent being infected again after your transplant, you may be prescribed hepatitis B immunoglobulin with an antiviral agent.
Recommended Reading: Can Hepatitis B Cause Meningitis
Treatment For Acute Hepatitis B
If you’re diagnosed with hepatitis B, your GP will usually refer you to a specialist, such as a hepatologist .
Many people do not have any troublesome symptoms, but if you do feel unwell, it can help to:
- get plenty of rest
- take over-the-counter painkillers, such as paracetamol or ibuprofen, for tummy pain
- maintain a cool, well-ventilated environment, wear loose clothing, and avoid hot baths or showers if itching is a problem
- take medication, such as metoclopramide, to stop you feeling sick, and chlorphenamine to reduce itching your doctor can give you a prescription for these if necessary
Most people recover completely in a couple of months, but you’ll be advised to have regular blood tests to check that you’re free of the virus and have not developed chronic hepatitis B.
What Do I Need To Know About Having Hepatitis B
If you have chronic hepatitis B, getting the right medical care can help you stay healthy. Taking good care of your liver is important. Talk with your doctor before you take any prescription medication, over-the-counter drugs, vitamins, or nutritional supplements to make sure they wont hurt your liver. You should also stay away from alcohol, because drinking can damage your liver.
Read Also: What Does Hepatitis B Core Antibody Positive Mean
C Patients Who Have Achieved Hbsag Loss Spontaneously Or With Therapy
Spontaneous HBsAg loss has been reported to occur at the rate of roughly 1% per year, but this rare event does not occur at a linear rate., In a study of 1,076 patients with CHB in Taiwan, cumulative probabilities of spontaneous HBsAg loss were 8.1% after 10 years and increased to 44.7% after 25 years. HBsAg loss can also occur in response to antiviral therapy, being more common with IFN than with NAs. Although progression of liver disease to cirrhosis or hepatic decompensation generally stops when patients lose HBsAg unless other causes of liver injury are present , the risk of HCC persists, particularly if HBsAg loss occurred in patients older than 50 years or in those with cirrhosis or coinfection with HCV or hepatitis D virus ., – Loss of HBsAg with acquisition of anti-HBs has been termed functional cure. This is distinguished from true cure, in which HBsAg and cccDNA are eliminated.
Guidance Statements for Monitoring Patients With Chronic HBV Infection Who Are Not Currently on Treatment
What Other Problems Can Hepatitis B Cause
In rare cases, acute hepatitis B can cause liver failure.
Chronic hepatitis B can develop into a serious disease that causes long-term health problems such as cirrhosis , liver cancer, and liver failure.
If you have ever had hepatitis B, the virus may become active again, or reactivated, later in life. This could start to damage the liver and cause symptoms.
Recommended Reading: Drinking Alcohol With Hepatitis C
How Is Hepatitis B Spread
You can become infected with hepatitis B through exposure to blood, semen and other bodily fluids of an infected person. You can get the infection by:
- Having unprotected sex.
- Sharing or using dirty needles for drug use, tattoos or piercing.
- Sharing everyday items that may contain body fluids, including razors, toothbrushes, jewelry for piercings and nail clippers.
- Being treated medically by someone who does not use sterile instruments.
- Being bitten by someone with the infection.
- Being born to a pregnant woman with the infection.
Hepatitis B is not spread by:
- Kissing on the cheek or lips.
- Coughing or sneezing.
- Hugging, shaking hands or holding hands.
- Eating food that someone with the infection has prepared.
- Breastfeeding.
How Do I Get Hepatitis B Treatment
Usually for adults, hepatitis B goes away on its own and you wont need treatment. Your doctor might tell you to rest, eat well, and get plenty of fluids. You may also get medicines to help with any symptoms you might have but be sure to talk with your doctor or nurse before taking anything.
If you have chronic hepatitis, there are medicines you can take to treat it. Your doctor will tell you about your options and help you get whatever treatment you need.
Also Check: Hepatitis A Is It Contagious
How Can I Avoid Getting Hepatitis B
There is a safe and effective vaccine that can protect you from getting hepatitis B. The vaccine is usually given in three doses over a six month period. The vaccine will give you long-lasting protection. A combined vaccine for hepatitis A and hepatitis B is also available.
Other ways to protect yourself or your loved ones include:
- Adopt safe sex practices.
- Avoid sharing personal hygiene items
- If you have been exposed to the hepatitis B virus , an injection of hepatitis B immune globulin may help protect you.
- If you are pregnant, make sure you are screened for hepatitis B. If the test result shows that you have the virus, make sure your baby receives the free hepatitis B vaccine. If you have hepatitis B, breastfeeding is safe if the baby has received both protective antibody called immune globulin, and the first dose of hepatitis B vaccine within the first 12 hours of life. Talk to your doctor about having your newborn immunized .
- If you decide to have a tattoo, piercing, manicure or pedicure, ensure that the facility uses single-use needles and inks and/or follows proper sterilization procedures.
Who Are Hepatitis B Carriers
Hepatitis B carriers are people who have the hepatitis B virus in their blood, even though they dont feel sick. Between 6% and 10% of those people whove been infected with the virus will become carriers and can infect others without knowing it. There are over 250 million people in the world who are carriers of HBV, with about 10% to 15% of the total located in India. Children are at the highest risk of becoming carriers. About 9 in 10 babies infected at birth become HBV carriers, and about half of children who are infected between birth and age 5 carry the virus. A blood test can tell you if you are a hepatitis B carrier.
Recommended Reading: Hepatic Metastasis From Colorectal Cancer
Update On Prevention Diagnosis And Treatment Of Chronic Hepatitis B: Aasld 2018 Hepatitis B Guidance
Division of Gastroenterology/Hepatology, University of California San Francisco, San Francisco, CA
ADDRESS CORRESPONDENCE AND REPRINT REQUESTS TO:
Norah Terrault, M.D., M.P.H.
Division of Gastroenterology/Hepatology, University of California San Francisco
513 Parnassus Avenue
Kyong-Mi Chang
Division of Gastroenterology, Corporal Michael J. Crescenz VA Medical Center & University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
Division of Gastroenterology/Hepatology, University of California San Francisco, San Francisco, CA
ADDRESS CORRESPONDENCE AND REPRINT REQUESTS TO:
Norah Terrault, M.D., M.P.H.
Division of Gastroenterology/Hepatology, University of California San Francisco
513 Parnassus Avenue
Kyong-Mi Chang
Division of Gastroenterology, Corporal Michael J. Crescenz VA Medical Center & University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
Potential conflict of interest: Dr. Hwang received grants from Merck and Gilead. Dr. Chang advises Arbutus. Dr. Lok received grants from Gilead and Bristol-Myers Squibb. Dr. Jonas consults for Gilead and received grants from Bristol-Myers Squibb and Roche. Dr. Brown consults and received grants from Gilead. Dr. Bzowej received grants from Gilead, Allergan and Cirius. Dr. Terrault received grants from Gilead and Bristol-Myers Quibb. Dr. Wong is a member of the United States Preventive Services Task Force . This article does not necessarily represent the views and policies of the USPSTF.
Classification Of Chronic Hepatitis
Cases of chronic hepatitis were once classified histologically as chronic persistent, chronic lobular, or chronic active hepatitis. Current classification specifies the following:
-
Etiology
-
Intensity of histologic inflammation and necrosis
Inflammation and necrosis are potentially reversible fibrosis usually is not.
Recommended Reading: Does Hepatitis C Ever Go Away
A Coinfection With Hcv
As with any patient with CHB, the treatment goals are to reduce risk of progression to cirrhosis- and liver-related complications, including HCC. In HBV-HCVâcoinfected patients, the viral activity responsible for liver disease can be determined by measuring HCV-RNA and HBV-DNA levels. If HCV RNA is detectable, treatment of HCV should be undertaken. If HBV DNA is detectable, treatment is determined by the HBV DNA and ALT levels . Importantly, treatment of one virus may lead to changes in the activity of the other virus, and thus monitoring during and after treatment is necessary to assess for viral activity.
In the IFN era, the treatment of choice for patients coinfected with HBV and HCV infections was peg-IFN and ribavirin for 24-48 weeks, depending on the HCV genotype. Moderate-to-high rates of HCV eradication and HBV suppression were reported with this combination., However, a rebound in serum HBV DNA after an initial decline and increased HBV replication in patients with undetectable HBV DNA before treatment have been reported with peg-IFN and ribavirin., , Similarly, direct-acting antiviral HCV therapy has been reported to increase HBV-DNA levels in HBsAg-positive patients and to elevate ALT concurrently with HBV reactivation, though the frequency of liver decompensation and liver failure are very low.- The majority of reported reactivation events occurred between 4 and 12 weeks of DAA treatment.