Additional File : Table S1
The influence of primary tumour location on survival in liver metastatic colorectal cancer, stratified by stage. Cox regression model adjusted for: age, sex, synchronous versus metachronous, size of largest liver metastasis , number of liver metastases, liver resection, lung metastases and stratified by stage.
Role Of Systemic Therapy
These patients could be defined as those with multiple and bilobar disease, which prevents obtaining a R0 resection by maintaining adequate FLR. Due to the increasing efficacy of systemic therapy, patients with CRClm only must be considered definitively unresectable after receiving 24 months of optimal treatment.
The choice of a systemic treatment strategy is based on patient-related factors, the mutational profile of the tumor, and the differing toxicity profiles of the constituent drugs .
The chemotherapy options for the treatment of patients with metastatic CRC are typically a cytotoxic doublet such as FOLFOX, CAPOX or FOLFIRI or, in selected patients, the triplet FOLFOXIRI or fluoropyrimidine monotherapy in unfit patients.
All patients considered for systemic therapy should be stratified according to RAS and BRAF mutations .
RAS mutant Bevacizumab has demonstrated its effectiveness independent of the state of RAS therefore, the treatment of choice in these patients is the combination of chemotherapy plus bevacizumab in those who can tolerate an intensive treatment .
Brief Overview Of Coding Genes
Malignant tumor causes serious harm to human health, and its occurrence is the result of the joint action of multi-factors, multi-stages and multi-genes, which is closely related to the disturbance of cell cycle and apoptosis regulation. In the occurrence and development of tumor, when various environmental factors and genetic pathogenic factors cause DNA damage, thus activating proto-oncogenes and inactivating tumor suppressor genes, resulting in disturbance of cell cycle regulation and imbalance of apoptosis regulation, resulting in abnormal cell growth, is the most fundamental cause of tumorigenesis. We sorted out the coding genes and their products that have been found in the research of colorectal cancer liver metastasis in recent years, and briefly worked out the mechanism in Table 1.
|
Table 1 Coding Genes in Liver Metastasis of Colorectal Cancer |
Also Check: Hepatitis C Antibody Negative Means
Width Of Resection Margin
Contrary to the historic 1-cm rule, several large series showed as long as R0 resection is achieved, extra margin width does not add DFS/OS advantage. From observations that survivals were similar between R0 and R1 resections if tumour showed optimal radiological or pathological response to neoadjuvant chemotherapy most recurrences occurred outside the surgical margin in a disseminated manner and margin re-resection from R1 to R0 did not improve long-term outcomes, positive margin status could just be a surrogate of aggressive tumour biology. The latter is increasingly recognized as the most important prognostic determinant. While an expected close margin is not a contraindication to surgery, surgeons should aim at wider margins to ensure a R0 resection.
Controversy 4: Role of surgery in the presence of extrahepatic disease: Management of CRLM in this setting remains controversial. Albeit defined as a poor prognostic factor, limited extrahepatic disease does not contraindicate liver surgery the prerequisite is all diseases including the primary CRC, LM and EHD can be completely resected or controlled. Resection of CRLM together with concurrent EHD significantly improved the 5-year OS from 0% to 28%, with a median survival of 31 mo.
Hub Genes Identification With Survival Analysis
The Cancer Genome Atlas colorectal cancer cohort were divided into two groups according to median gene expression level. Gene Expression Profiling Interactive Analysis 2.0 was used to evaluate the difference in disease-free survival between the groups . MantelCox test value < 0.05 was set to determine hub genes associated with poor prognosis of colorectal cancer. Comparisons of hub genes expression between LM and PC from GSE41258 were analyzed using Wilcoxon rank sum test with continuity correction p< 0.05 were considered as statistically significant.
Read Also: Hepatitis B And C Can Be Spread By
Gene And Potential Drugs Interaction
Protein expression level in different stages of CRC was curated from the Clinical Proteomic Tumor Analysis Consortium by UALCAN. The immunohistochemical images of the hub genes in advance and early stages were also identified using Human Protein Atlas . The Drug Gene Interaction Database was used to predict the potential drugs targeting hub genes . Drugs with combined value of query score and interaction score > 10 were selected for docking. Homologous structures of gene-encoded protein were downloaded from the Protein Data Bank and three-dimension structures of drug from PubChem . Autodock software was used to preprocess and define the proteins and drugs to receptors and ligands, respectively . The docking grid box was set to envelop the whole receptors docking parameters was set as genetic algorithm with short maximum number of evaluations. The docking results were ranked by energy, and the first model was exported to Pymol for visualization .
Identification Of Hub Genes Related To Liver Metastasis Of Colorectal Cancer By Integrative Analysis
- 1Research Laboratory of Cancer Epigenetics and Genomics, Department of General Surgery, Frontiers Science Center for Disease-Related Molecular Network, State Key Laboratory of Biotherapy and National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University, Chengdu, China
- 2Research Laboratory of Cancer Epigenetics and Genomics, Department of General Surgery, Frontiers Science Center for Disease-related Molecular Network, West China Hospital, Sichuan University, Chengdu, China
Also Check: Hepatitis C Genotype 3 Treatment
Epidemiology Of Colorectal Cancer
Colorectal cancer is among the leading malignant tumours both by incidence and by death rate . Globally, in the year 2012, it was the 3rd most frequent cancer in men and the 2nd in women . The incidence and mortality is higher in males . The highest incidence rates are found in Australia and New Zealand, Europe and North America contrasting with low incidence in Africa and South Central Asia. As shown in Table 2, the incidence is generally higher in more developed countries . The decrease in colorectal cancer incidence in USA reflects successful screening and removal of colorectal adenomas. The incidence growth, recently observed in Western Asia and Eastern Europe , reflects increased prevalence of risk factors as diet, obesity and smoking.
| Gender |
Global incidence and mortality attributable to colorectal cancer by Globocan data
1 Among all cancers.
ASR, age-standardised ratio per 100,000.
| Gender and welfare status |
Incidence and mortality caused by colorectal cancer by regional welfare
1Includes Europe, North America, Australia, New Zealand and Japan.
2Includes Africa, Asia , Latin America, Melanesia, Micronesia and Polynesia.
ASR, age-standardised ratio per 100,000.
Maximizing Regional Treatment Of Colorectal Cancer Liver Metastasis To Decrease Intrahepatic Recurrence
The role of hepatic arterial infusion for patients with resected CRLM initially was tested without concurrent systemic therapy, which at the time of the initial trials did not include modern systemic agents such as oxaliplatin and irinotecan. To date, there have been no prospective randomized controlled trials comparing adjuvant HAI with modern systemic therapy vs modern systemic therapy alone in patients with resected CRLM. In 2016, Kemeny et al reported on an analysis of 4 consecutive HAI adjuvant trials for patients with resected CRLM from 1991 to 2009 . The patients were divided into 2 groups: those treated before and after 2003, corresponding to the incorporation of modern systemic oxaliplatin or irinotecan-containing regimens. With a median follow-up period of 11 years, the investigators reported that patients treated after 2003 had a 5- and 10-year OS of 78% and 61%, respectively, with the median survival not being reached. Patients treated before 2003 had a 3- and 5-year DFS of 42% and 41%, respectively. Taken together, these data support that properly selected patients with CRLM can have hepatic resection of their disease followed by adjuvant systemic therapy plus HAI and achieve a 5-year survival as high as 78%. However, similar to toxicity associated with systemic therapy, treatment with HAI has risks, including biliary sclerosis in less than 5% of patients, that needs to be balanced with the anticipated benefit of treatment.
Recommended Reading: Hepatitis B Surface Antibody Positive
Expert Review And References
- Alexander HR Jr, Berlin J, Moeslein F. Metastatic cancer to the liver. DeVita VT Jr, Lawrence TS, Rosenberg SA. Cancer: Principles and Practice of Oncology. 9th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins 2011: 149:2177-2191.
- BC Cancer Agency . Cancer Management Guidelines: Secondary Neoplasms of the Liver. BC Cancer Agency 2006: .
Management Of Rectal Cancer And Liver Metastatic Disease: Which Comes First
Georgios Tsoulfas
11st Surgical Department, Aristotle University of Thessaloniki, Papageorgiou General Hospital, 56429 Thessaloniki, Greece
24th Surgical Department, Aristotle University of Thessaloniki, Papanikolaou General Hospital, 57010 Thessaloniki, Greece
Abstract
In the last few decades there have been significant changes in the approach to rectal cancer management. A multimodality approach and advanced surgical techniques have led to an expansion of the treatment of metastatic disease, with improved survival. Hepatic metastases are present at one point or another in about 50% of patients with colorectal cancer, with surgical resection being the only chance for cure. As the use of multimodality treatment has allowed the tackling of more complicated cases, one of the main questions that remain unanswered is the management of patients with synchronous rectal cancer and hepatic metastatic lesions. The question is one of priority, with all possible options being explored. Specifically, these include the simultaneous rectal cancer and hepatic metastases resection, the rectal cancer followed by chemotherapy and then by the liver resection, and finally the liver-first option. This paper will review the three treatment options and attempt to dissect the indications for each. In addition, the role of laparoscopy in the synchronous resection of rectal cancer and hepatic metastases will be reviewed in order to identify future trends.
1. Introduction
5. The Role of Laparoscopy
Read Also: What Are The Symptoms Of Hepatitis C Infection
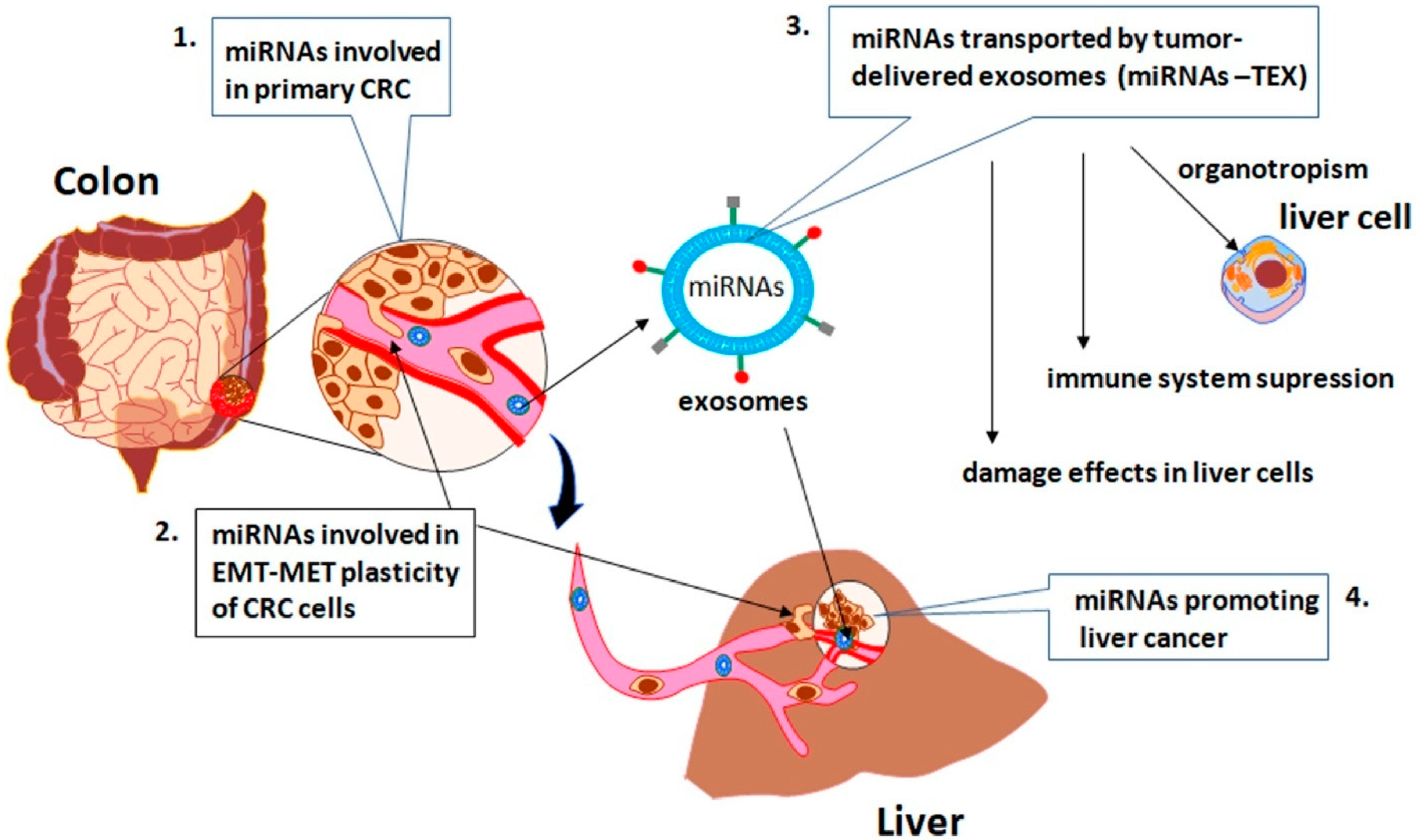
The Role Of Oncogenes In Liver Metastasis Of Colorectal Cancer
Proto-oncogenes exist in the genomes of normal biological cells. Like tumor suppressor genes, proto-oncogenes play an important role in the regulation of cell growth and proliferation. Under normal circumstances, the ability is that the proto-oncogenes in the genome are in a state of low expression or non-expression, but when they encounter certain conditions, such as viral infection, chemical carcinogens or radiation, the proto-oncogenes will be abnormally activated and converted to oncogenes to induce cell carcinogenesis. In Table 2, we sorted out the abnormally expressed oncogenes found in the study of CRLM in recent years.
|
Table 2 Non-Coding RNAs in Liver Metastasis of Colorectal Cancer |
MACC1
The MACC1 gene is located on human chromosome 7 , there are about 76,762 base pairs, including 7 exons and 6 introns. Its cDNA has a sequence of 2559 nucleotides and encodes a protein of 852 amino acids. MACC1 protein is a protein complex composed of multiple domains, including ZU5, SH3 and two C-terminal death domains . It has been found that transfection of MACC1 containing SH3 domain and proline-rich sequence into colon cancer cell lines that do not express MACC1 can enhance cell viability and proliferation, while MACC1 mutants without this domain lack these abilities, indicating that SH3 domain and SH3 binding motif are essential to maintain the biological function of MACC1.
SNCG
Chemokine and Its Receptor
Radiologic Imaging Techniques In The Diagnostics Of Liver Metastases Of Colorectal Cancer
The radiologic techniques of liver examination comprise computed tomography, magnetic resonance imaging, ultrasound evaluation and fluorodeoxyglucose positron emission tomography . CT and MRI represent the cornerstone in the diagnostics of liver metastases of colorectal cancer . US has the benefits of wide accessibility and lack of irradiation. However, it is considered a historical method in developed countries as USA due to lower sensitivity and specificity. These parameters can be improved by contrast-enhanced US . Positron emission tomography has certain indications.
MRI is characterised by the highest specificity and sensitivity, especially regarding metastases smaller than 1 cm in diameter . The imaging technology is based on different physical status of water and fat protons . To identify liver metastases, MRI routinely includes T1, T2 and diffusion-weighted sequences before and after administration of gadolinium-containing contrast agent. The CRC metastases are hypointense on T1 but hyperintense on T2 and diffusion-weighted imaging sequences. The contrasting reveals metastasis as a hypovascular focus with an irregular rim of enhancement .
MRI is contraindicated in patients having incompatible implants, e.g., pacemakers affected by claustrophobia or impaired glomerular filtration rate, or unable to hold the breath for longer than 20 seconds. CT should be performed in these patients .
You May Like: Does Hepatitis C Affect The Brain
Controversy : Optimal Surgical Sequencing For Resectable Synchronous Disease
To date, there has been no randomized trial on the surgical approach to synchronous disease. The optimal strategy remains controversial. Decision should be individualized taking into consideration of patients fitness and tumour status whether the primary CRC is symptomatic or obstructive , as well as the extent of CRLM and magnitude of liver resection required. Treatment strategy is best determined in multi-disciplinary setting, which has been associated with greater likelihood of simultaneous resection.
The conventional approach comprises of resection of the primary CRC followed by liver metastasectomy, commonly with chemotherapy applied between the two surgeries. This avoids potential complications of the primary tumour, but carries significant risk of CRLM progression beyond resectability less than 30% patients completed the whole treatment and underwent liver resection.
A meta-analysis comparing the classical, synchronous and liver-first approaches did not show any difference in surgical outcomes or survival advantage. Because of the limited evidence available, the optimal treatment strategy is unclear. Choice of procedure should be personalized and based on expertise available in different institutions.
Patient Selection And Prognostic Prediction
Although hepatic resection gives the best results on a population level, not everyone with technically operable disease benefits from surgery. Appropriate patient selection ensures the offered intervention, surgical or systemic, is optimal to each particular patient.
Resectability of a particular CRLM should be determined in a multidisciplinary setting, with input from hepatobiliary surgeons, oncologists, radiologists and pathologists. Apart from pure technical considerations, there is a growing emphasis placed on oncological resectability. The former focuses on whether a margin-negative resection can be achieved while preserving a liver remnant comprised of two contiguous segments with adequate volume, function, vascular inflow and outflow, as well as biliary drainage. Oncological/prognostic evaluation aims to select patients with higher likelihood of cure or sustained disease remission taking tumour biology , mutation status, intra-hepatic tumour burden and extent of EHD into consideration. Resection criteria based on the number, maximal size and distribution of tumours no longer apply instead resectability should be defined case-by-case based on different prognostic factors. With continued advancement in surgical technology, systemic therapies and multimodality treatment, the definition of resectability will continue to evolve and expand to cover advanced diseases once deemed non-resectable.
Don’t Miss: Chronic Hepatitis C Without Hepatic Coma
How A Multidisciplinary Team Treats Colon And Liver Cancer
A multidisciplinary approach to colon and liver cancer treatment means that youll get an optimized plan based on your individual medical history, tumor type and genes. Several types of cancer specialists work together on your team so you can benefit from their combined expertise.
The center where you have your treatment should have access to multiple types of doctors who communicate regularly, says Dr. Adrian Murphy, instructor of oncology at the Johns Hopkins University School of Medicine. This is extremely important because one type of specialist alone is not able to manage your care. This truly requires collaboration.
There are generally six types of specialists on a multidisciplinary cancer team:
Treating Colon Cancer That Has Spread To The Liver: A Team Approach
If you or a loved one has a colon cancer diagnosis, there is also the chance that the cancer will spread to other organs, most commonly the liver. However, according to Dr. Richard Burkhart, a Johns Hopkins cancer surgeon and researcher, advancements in the treatment of liver tumors caused by colon cancer have improved survival rates drastically. In fact, 40-60 percent of patients treated for isolated colon cancer liver metastasis are still alive five years after treatment.
At Johns Hopkins, researchers such as Dr. Burkhart are conducting clinical trials to find ways to slow or prevent the spread of colon cancer. These trials, coupled with a multidisciplinary, or team, approach using molecular testing, surgical techniques, chemotherapy and radiation, have greatly improved life expectancy for patients in the last 10 years.
Also Check: What Is Included In A Hepatitis Panel
Recurrence After Surgical Resections For Hepatic And Pulmonary Metastases
Among 30 patients who underwent surgical resections for hepatic and pulmonary metastases, 25 developed recurrences when recurrence was defined as the first recurrent disease after at least one resection each for hepatic and pulmonary metastases. Locations of recurrences were as follows: lung in 11 patients, liver and lymph node in four each, both liver and lung in three, peritoneum, local recurrence and brain in one each. Re-resection could be performed in 15 of the 25 patients. Of the remaining 10 patients, eight received systemic chemotherapy, one each received radiation therapy and best supportive care.
Systemic Therapy For Treatment Of Crlm
Advances in systemic chemotherapy as well as biologic agents have significantly improved the OS of patients with CRLM and other metastatic disease in CRC treatment. Based on current evidence, possible first line chemotherapy for treating CRC with CRLM include: fluorouracil, leucovorin and oxaliplatin , fluorouracil, leucovorin, irinotecan , capecitabine plus oxaliplatin and fluorouracil, leucovorin, oxaliplatin and irinotecan . They can also be complimented with biological agents such as bevacizumab or cetuximab in the course of treatments. The RAS and BRAF status are crucial in deciding if these biologic agents will be useful in the treatment strategies as discussed above. Fakih summarised very nicely the recommendations based on the RAS and BRAF mutation status. FOLFOXFIRI with or without bevacizumab, FOLFOX or FOLFIRI with anti-EGFR are favoured for downstaging for resection. However, bevacizumab must be avoided in patients with high risk of bowel perforation or thrombotic events. These regimens have been shown to have good response rate of > 50% with improvement of OS by around 30 months .
You May Like: How Do You Catch Hepatitis C