Drawbacks To Screening For Hepatitis C
A patient’s worry or anxiety while waiting for test results, concerns about insurance coverage of evaluation and treatment, adverse effects of treatment, and complications associated with liver biopsy can limit screening for hepatitis C. However, the accuracy of HCV RNA testing, the availability of medication assistance programs for uninsured patients, and improved treatments with fewer side effects and shorter duration should allay some of the anxiety associated with the screening process.
Take An Active Approach To Testing
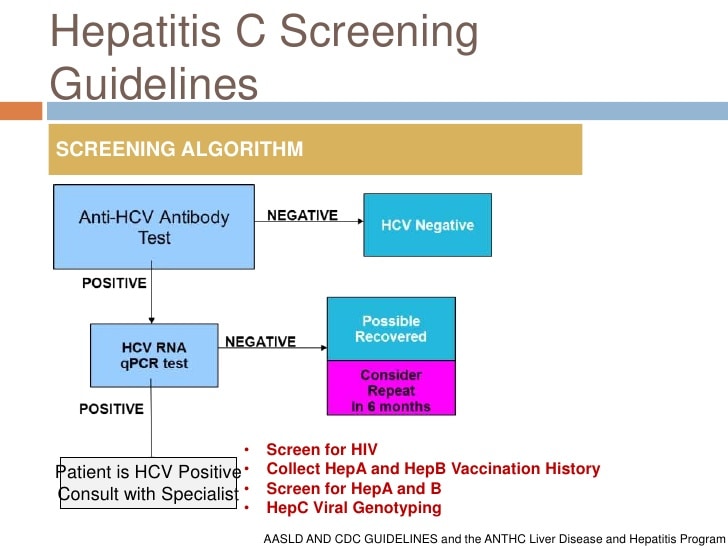
Testing for HCV: the diagnosis of HCV infection requires 2 tests.
Time For Processing Hcv Ab Test Results
The turnaround time for 3rd-generation EIAs is at least 1 day. Many labs do not perform the tests on site and must send specimens to another lab for processing, which may further increase the turnaround time.
A point-of-care test is also available. The OraQuick® HCV Rapid Antibody Test is an FDA-approved test that can be performed with a fingerstick . It is also a CLIA-waived test and therefore can be used in clinic offices and outreach facilities. Results are reported as reactive or nonreactive within 20 minutes. Just as for the standard HCV Ab test done in the lab, a positive OraQuick® test must be confirmed by an HCV RNA test. The sensitivity and specificity of the test is similar to that of the laboratory-based assays.
Also Check: Can You Get Hepatitis C Sexually
Clinical Features And Natural History
Persons with acute HCV infection are typically either asymptomatic or have a mild clinical illness like that of other types of viral hepatitis . Jaundice might occur in 20%30% of persons, and nonspecific symptoms might be present in 10%20% of persons. Fulminant hepatic failure following acute hepatitis C is rare. The average time from exposure to symptom onset is 212 weeks . HCV antibodies can be detected 410 weeks after infection and are present in approximately 97% of persons by 6 months after exposure. HCV RNA can be detected as early as 12 weeks after exposure. The presence of HCV RNA indicates current infection .
Benefits Of Early Detection Or Treatment
The USPSTF found no direct evidence on the benefits of HCV screening vs no screening on health outcomes or the effects of prenatal HCV screening on the risk of vertical transmission.1 Treatment studies focused on populations without cirrhosis who are more likely to be asymptomatic and identified by screening. Of the trials of DAA regimens , 14 were multinational 11 were conducted in the US or Canada and the remainder were conducted in New Zealand, Egypt, France, or Asia. In 29 trials, 60% to 100% of patients were white.1 The trials evaluated a variety of DAA regimens recommended in current guidelines. Treatment duration was 12 weeks in all but 2 trials, which allocated patients to either 8 or 12 weeks of treatment. Eleven trials were of good quality and 22 were of fair quality. Forty-nine trials found DAA regimens to be associated with pooled SVR rates ranging from 95.5% to 98.9% across genotypes. Evidence was greatest for genotype 1 infection , the most frequent genotype in the US.1 Sustained virologic response rates were similar in trials that stratified patients according to age, sex, race/ethnicity, or treatment experience with non-DAA regimens.1
Recommended Reading: How Is Hepatitis B And C Transmitted
Prevention Of Hcv Disease
Compared with no screening scenario, 1Yr-Risk, 1Yr-All, 5Yr-All and 10Yr-All scenarios would prevent 5500 , 8000 , 10 900 and 12 700 new HCV infections, respectively, in the next 30 years. Of these cases prevented by prison screening programs, 89%â92% of averted infections would have occurred in the general population . For all scenarios, infections averted would peak between years 2020 and 2024 and decline afterwards . Interventions in prisons would reduce the number of HCV-infected people in prisons over time, and the benefits of screening would peak around year 2035 and decline afterwards . Furthermore, compared with no screening, HCV screening in prisons could prevent 4200â11 700 liver-related deaths, 300â900 liver transplants, 3000â8600 cases of hepatocellular carcinoma and 2600â7300 cases of decompensated cirrhosis in the next 30 years. Of note, among liver-related deaths averted, 80% would have occurred in the outside community.
Projected Reduction of Hepatitis C Virus Transmission and Hepatitis C Virus -Associated Costs
Recommendation For Linkage To Care
RECOMMENDED RATING All persons with active HCV infection should be linked to a healthcare provider who is knowledgeable in and prepared to provide comprehensive management. IIa, C
Improved identification of active HCV infection and treatment advances will have limited impact on HCV-related morbidity and mortality without concomitant improvement in linkage to care. All patients with current HCV infection and a positive HCV-RNA test should be evaluated by a healthcare provider with expertise in assessment of liver disease severity and HCV treatment. Subspecialty care and consultation may be required for persons with HCV infection who have advanced fibrosis or cirrhosis , including possible referral for consideration of liver transplantation in those with evidence of hepatic decompensation.
Only an estimated 13% to 18% of HCV-infected persons in the US had received treatment by 2013 . Lack of appropriate clinician assessment and delays in linkage to care can result in negative health outcomes. Furthermore, patients who are lost to follow-up fail to benefit from evolving evaluation and treatment options.
Commonly cited patient-related barriers to treatment initiation include contraindications to treatment lack of acceptance of treatment and lack of access to treatment .
Table 2. Common Barriers to and Misconceptions Regarding HCV Treatment and Potential Strategies
Also Check: Colloidal Silver And Hepatitis C
Hepatitis C Virus Infection In Adolescents And Adults: Screening
Recommendations made by the USPSTF are independent of the U.S. government. They should not be construed as an official position of the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.
| Adults aged 18 to 79 years | The USPSTF recommends screening for hepatitis C virus infection in adults aged 18 to 79 years. | B |
- View the Clinician Summary in PDF
Pathophysiology And Natural History
There are six known genotypes of HCV. The most common genotypes in the United States, comprising 97% of all U.S. HCV infections, are 1 , 2, and 3.9
The mechanism of hepatocyte damage induced by HCV infection is not completely understood but may involve direct cell injury and a local immune-mediated mechanism that causes a chronic inflammatory state.10,11 Acute HCV infection progresses to chronic disease in 50% to 80% of patients and clears spontaneously in 20% to 50% of patients.10 Of persons with chronic disease, 20% will develop cirrhosis, end-stage liver disease, and/or hepatocellular carcinoma.12
Figure 1 illustrates the natural history of HCV infection.10
Figure 1.
Natural history of hepatitis C virus infection.
Reprinted with permission from Pawlotsky JM. Pathophysiology of hepatitis C virus infection and related liver disease. Trends Microbiol. 2004 12:97.
Figure 1.
Natural history of hepatitis C virus infection.
Reprinted with permission from Pawlotsky JM. Pathophysiology of hepatitis C virus infection and related liver disease. Trends Microbiol. 2004 12:97.
Don’t Miss: Can A Hepatitis B Carrier Get Vaccinated
Interpreting Hcv Rna Test Results
It is essential that the provider understands how to interpret HCV RNA test results, especially during the course of HCV treatment.
| Result of HCV RNA Test | Interpretation |
|---|---|
| A quantified viral load — any exact number | Ongoing HCV infection |
| “Detected” | The HCV RNA is detectable but the number of international units is so low that it cannot be quantified accurately. This indicates extremely low level of virus is present. |
| “< 12 IU/mL” or “< 15 IU/mL” or “< 25 IU/mL” All of these are “less than the LLOQ” | HCV RNA is undetectable. No virus is detected at all in the patient’s serum specimen. |
What Type Of Information Should I Provide A Patient With A Non
- Explain the meaning of the non-reactive antibody test, ensuring that the patient understands a negative antibody test does not protect him/her from future infection in the event of risk-taking behaviors.
- Discuss that if the patient was recently exposed , he/she may be in a window period and recommend repeat screening in 6 months, and provide information on hepatitis C prevention, risk and harm reduction.
- Encourage the patient to make healthy choices and to get vaccinated against hepatitis A and B, if appropriate.
Also Check: Is Hepatitis Ca Sexually Transmitted Disease
Does The Law Require Insurance Companies To Pay For The Hepatitis C Test What If The Patient Doesn’t Have Insurance
No, the law does not require insurance companies to pay for the test. However, the U.S. Preventive Services Task Force issued a B grade on screening for hepatitis C among persons born between 1945 and 1965. The USPSTF recommendation signifies that hepatitis C screening among this population will be covered by most public and private insurance. This is because the Affordable Care Act requires that private insurance plans cover USPSTF A or B recommended services without cost sharing. Medicaid Managed Care plans must also cover these services. Currently, hepatitis C testing is not covered by Medicare.
If a patient accepts the offer of a test but lacks insurance or has insurance that may not pay for the test, clinicians should follow their normal protocol for any other test that might be ordered and may not be covered.
In addition, there are a number of free hepatitis C rapid testing sites throughout the state. For a complete list of those sites, go to:
- the DOH web site at: or
Hepatitis C Screening: Questions For The Doctor
Hepatitis C is a serious liver disease caused by the hepatitis C virus . The most common way to get hepatitis C is by coming into contact with the blood of someone who has it.
Everyone ages 18 to 79 needs to get tested for hepatitis C at least once.
Many people who have hepatitis C live for years without feeling sick. But the virus can still damage your liver even when there arent any symptoms. You could also spread the virus to others without knowing it.
The only way to know for sure if you have hepatitis C is to get a blood test. Medicine can cure most cases of hepatitis C.
Read Also: Can Hepatitis B Cause Meningitis
Budget Impact On Prison System
The first year cost of HCV screening, treatment and chronic HCV management in 2015 under risk-based screening and opt-out screening would be $900 million and $1146 million, respectively, spread over the prison systems in all states. The corresponding costs would decrease below 66 million after 15 years . The first-year budget needed to implement universal opt-out screening followed by treatment with DAAs would require an additional 12.4% over the current healthcare budget of state and Federal prisons . However, after 15 years, prisons would need only an additional 0.7% of the current healthcare budget because of decrease in HCV prevalence in both prisons and society.
Total cost of HCV screening and treatment in prisons from 2015 to 2029
The budget needed to screen, treat HCV infection, and manage chronic hepatitis C in prisons under 1-time opt-out universal screening of currently incarcerated inmates and entrants for 10 years . The annual budget decreased substantially from 2015 to 2029 due to decrease in prevalence and discounting of future expenditures at 3% annually.
Why Test All Your Adult Patients
- New cases of hepatitis C are on the rise, particularly among reproductive age adults. Rates of new HCV infections increased by more than 60% from 2015 to 2019. And in 2019, more than 63% of HCV infections occurred among adults 20-39 years of age.
- Your patients arent aware of their risk. Almost half of people with hepatitis C are unaware of their infection. Testing is the first step to accessing curative treatment. Without treatment, approximately 15-20% of adults with chronic HCV infection will develop progressive liver fibrosis and cirrhosis.
- Hepatitis C can be cured. Over 90 percent of people infected with HCV can be cured with 8-12 weeks of oral therapy. Treatment of hepatitis C is associated with reductions in mortality among persons with chronic hepatitis C.
Also Check: Is Hepatitis A Sexually Transmitted Disease
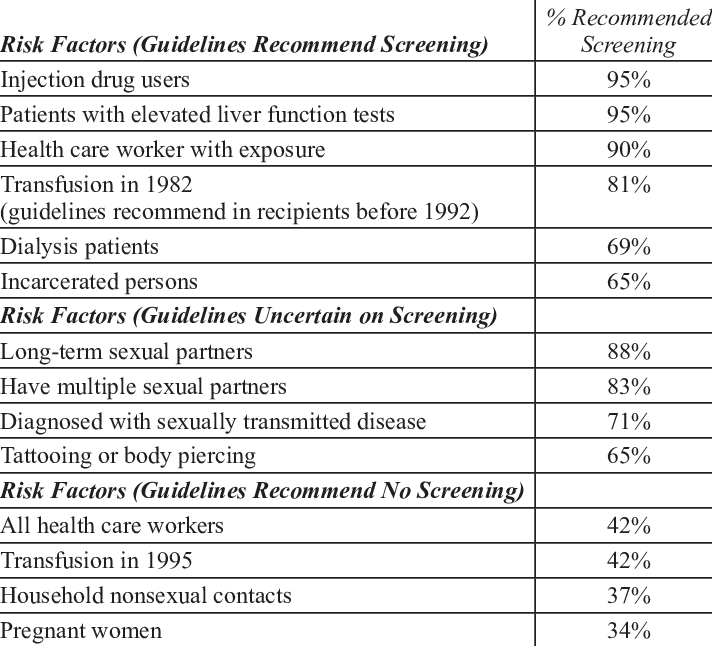
Under The New Law Do All Patients At
Under the new law, only those patients born between 1945 and 1965 are required to be offered a hepatitis C screening test. Although the new law requires the offer of a test only for those born between 1945 and 1965, CDC recommends hepatitis C testing be offered to all persons at risk for hepatitis C, such as injection drug users, those that received a blood transfusion or organ donation before 1992, persons living with HIV, anyone with abnormal liver tests, health and safety workers who have been exposed to blood on the job and persons on long term dialysis.
All Adults Pregnant Women And People With Risk Factors Should Get Tested For Hepatitis C
Most people who get infected with hepatitis C virus develop a chronic, or lifelong, infection. Left untreated, chronic hepatitis C can cause serious health problems, including liver damage, cirrhosis, liver cancer, and even death. People can live without symptoms or feeling sick, so testing is the only way to know if you have hepatitis C. Getting tested is important to find out if you are infected so you can get lifesaving treatment that can cure hepatitis C.
Don’t Miss: How Does Someone Catch Hepatitis C
Over 250000 Canadians Believed To Be Infected But Many Unaware They Have Blood
Canadians born between 1945 and 1975 should be tested for the potentially liver-destroying virus hepatitis C, a new set of guidelines recommends.
More than 250,000 Canadians are believed to be infected with hepatitis C, but an estimated 40 to 70 per cent are unaware they harbour the blood-borne virus because it can take decades before symptoms become evident. Chronic infection can lead to cirrhosis of the liver or liver cancer.
The Canadian Association for the Study of the Liver, a national group of health-care providers and researchers, published its guidelines on testing and treating hepatitis C in Monday’s edition of the CMAJ.
A key recommendation is that people be tested based on their age not only possible risk factors, said Dr. Jordan Feld, a liver specialist at Toronto’s University Health Network and a co-author of the guidelines.
“And the reason we’ve done this is it just happens that somewhere between two-thirds and three-quarters of people with hepatitis C were born between 1945 and 1975 in Canada,” he said.
“So just the way someone gets a blood pressure check or a cholesterol check or a colonoscopy based on their age, we would recommend that they get a hepatitis C test if they’re born between those years.
“And if we do that, we hopefully diagnose the vast majority of people living with hepatitis C.”
Does The Referral For Follow
The law does not specify the clinician specialty but does specify that the referral must be for follow-up hepatitis C care. The patientâs medical record should reflect the name of the provider/facility to whom the referral appointment was made. The Departmentâs website includes contact information for providers of hepatitis C care and treatment.
Don’t Miss: What Is The Treatment For Hepatitis C
Discussing Screening Results With Clients
The medical personnel who ordered or arranged the screening test, not counselors, usually explain the results. Hepatitis screening should be part of the intake physical examination in an opioid treatment program, and medical personnel may report the results. However, the client may want to discuss the results with the counselor or ask the counselor questions.
Anxiety might interfere with some clients ability to comprehend or retain information, which might need to be repeated.
Suggestions for conversations with clients when the test results are negative include the following:
- Explain results clearly and simply: So the HCV screening result was negative? This means that, as of 6 months ago, you did not have .
- Emphasize that a negative result to an HCV test does not indicate to and that the client should take precautions to avoid . If a relapse to drug use occurs, advise clients to avoid sharing any drug paraphernalia or equipment. Specify that this includes cookers, cotton, water, needles, syringes, pipes, and straws.
- Emphasize the importance of getting HAV and HBV vaccinations. Provide information about the availability of low- or no-cost vaccinations.
Clients whose screening test results are positive for will need additional tests and examinationsusually with doctors who specialize in diseases of the liver to get accurate diagnoses and to determine their health status and the extent of liver damage. These tests are described in .
Uspstf Hcv Screening Recommendations
In March 2020, the U.S. Preventive Services Task Force issued updated recommendations regarding screening for HCV. The USPSTF now recommends routine screening for all adults in the United States 18-79 years of age, including pregnant women . The 2020 USPSTF recommendation for HCV screening was categorized as a grade B recommendation, which means that the USPSTF concludes with moderate certainty that screening for HCV in adults 18-79 years of age has substantial net benefit and that health care providers should offer this service . The USPSTF notes that most adults will require HCV screening only once, but those with ongoing risk of acquiring HCV will need periodic screening. For persons younger than 18 or older than 79 years of age, screening for HCV can be considered if the individual is considered at high risk for having acquired HCV. The 2020 USPSTF recommendations for HCV screening is clearly a major change from the prior 2013 USPSTF recommendations to screen adults born during 1945-1965 and those with known risk.
Don’t Miss: Hepatitis C And Liver Disease