The Global Burden Of Hbv And Hiv Infections
UNAIDS has described AIDS as the most devastating disease humankind has ever faced, with HIV having infected more than 60 million people in the past 20 years . Out of the 42 million people currently living with HIV/AIDS, 29.4 million reside in sub-Saharan Africa . The only other region in the world where prevalence rates are above 1% is the Caribbean, with a prevalence of 2.4%. The global adult prevalence rate has been estimated at 1.2% .
| People living with HIV/AIDS | Adult HIV prevalence rate |
|---|
- HBV, hepatitis B virus HIV, human immunodeficiency virus.
- * Figures taken from UNAIDS, 2002 .
- Figures taken from CDC website, 2003 .
It is clear that the southern African countries are currently experiencing the worst of the pandemic, with the highest adult prevalence rates being reported in Botswana , Lesotho , Swaziland , and Zimbabwe . On the other hand, central and west African countries are still in the early stages of the HIV epidemic, with prevalence rates ranging from less than 1% to 12.9% . In East Africa, Uganda has already experienced the peak of its HIV epidemic , and has managed to bring prevalence rates down to 11.2% in 2000. The average adult prevalence rate for the entire sub-continent has been estimated at 8.8%, whereas that for North Africa and the Middle East is only 0.3% .
What Puts Me At Risk For Hepatitis C
Hepatitis C is usually spread when blood from a person infected with the Hepatitis C virus enters the body of someone who is not infected. Today, most people become infected with the Hepatitis C virus by sharing needles or other equipment to inject drugs. Hepatitis C was also commonly spread through blood transfusions and organ transplants prior to the early 1990s. At that time, widespread screening of the blood supply began in the United States, which has helped ensure a safe blood supply.
STDs
Hepatitis B Causes And Risk Factors
Itâs caused by the hepatitis B virus, and it can spread from person to person in certain ways. You can spread the hepatitis B virus even if you donât feel sick.
The most common ways to get hepatitis B include:
- Sex. You can get it if you have unprotected sex with someone who has it and your partnerâs blood, saliva, , or vaginal secretions enter your body.
- Sharing needles. The virus spreads easily via needles and syringes contaminated with infected blood.
- Accidental needle sticks.Health care workers and anyone else who comes in contact with human blood can get it this way.
- Mother to child.Pregnant women with hepatitis B can pass it to their babies during childbirth. But thereâs a vaccine to prevent newborns from becoming infected.
Hepatitis B doesnât spread through kissing, food or water, shared utensils, coughing or sneezing, or through touch.
Read Also: What Is The Treatment Of Hepatitis B
Also Check: Can You Donate Blood If You Had Hepatitis A
Prevent Infection After Contact With The Virus
If you think you have been in contact with the hepatitis B virus, see your doctor right away. Doctors typically recommend a dose of the hepatitis B vaccine to prevent infection. In some cases, doctors may also recommend a medicine called hepatitis B immune globulin to help prevent infection. You must get the vaccine dose and, if needed, HBIG shortly after coming into contact with the virus, preferably within 24 hours.
Read Also: Blood Test For Hepatitis C Virus
Should People With Hiv Get Tested For Hbv

CDC recommends that all people with HIV get tested for HBV. Testing can detect HBV even when a person has no symptoms of the infection.
There are several HBV blood tests. Results of different tests show different things. For example, a positive hepatitis B surface antigen test result shows that a person has acute or chronic HBV and can spread the virus to others.
Also Check: Hepatitis C Test Results Non Reactive
What Are The Treatments For Hepatitis B
If you think you may have been exposed to hepatitis B, its important to talk with a healthcare professional as soon as possible.
A doctor or other healthcare professional may administer the first dose of the hepatitis B vaccine and a shot of hepatitis B immunoglobulin. This is a combination of antibodies that provide short-term protection against the virus.
Though both can be given up to a week after exposure, theyre most effective at preventing infection if administered within 48 hours.
If you receive a diagnosis of acute hepatitis B, a doctor may refer you to a specialist. They may advise you to get regular blood tests to ensure you dont develop chronic hepatitis.
Many people with acute hepatitis B dont experience serious symptoms. But if you do, it can help to:
- get plenty of rest
- take over-the-counter pain mediation, like naproxen, when needed
Other lifestyle changes may also be needed to manage your infection, such as:
- eating a nutritious, balanced diet
- avoiding substances that can harm your liver, such as:
- certain herbal supplements or medications, including acetaminophen
If blood tests show you still have an active infection after 6 months, your doctor may recommend further treatment, including medications to help control the virus and prevent liver damage.
Changes In Disease Progression
There are a number of studies in this area of research from non-African countries. Some of these suggest that HIV immunosuppression may reduce liver damage as a result of a less aggressive HBV-specific immune response , and this is supported by reports of a reduction in icteric illness in acute HBV infections, in HIV-positive patients . However, HIV infection has been found to exacerbate liver disease, with an early study finding death from liver failure in four of five HIV-positive HBV carriers, compared with two of six HIV-negative HBV carriers . More recently, it was found that HIV and HBV co-infected patients have a significantly increased risk of dying from liver disease. This risk was found to increase after starting treatment for HIV using highly active antiretroviral therapy . In addition, there have been reports of hepatotoxicity and reactivation of HBV in co-infected individuals, when using HAART.
Conversely, there is no convincing evidence that HBV hastens progression to AIDS , in HIV and HBV co-infected patients, although there were early speculations that HBV infection may be a co-factor . Most of these speculations were based on very small studies, while larger studies have shown no association between HBV infection and progression to AIDS .
Read Also: Hepatitis C And Liver Transplantation
Increase In Carriers With Active Hbv
As discussed earlier, many studies have indicated a higher prevalence of HBV infection among HIV-positive individuals. This has been found to be true in non-African countries , as well as in some areas of sub-Saharan Africa . In sub-Saharan Africa , where most sexually active adolescents and adults have been exposed to HBV before being exposed to HIV, the association between HIV and HBV infection is not expected to be as strong as in countries of low HBV endemicity. For example, in the United States of America, up to almost seven-fold increases in HBV infections have been reported in HIV-positive patients , whereas most of the sub-Saharan studies that have found an association have reported increases less than two-fold , with only one reporting as much as a four-fold increase .
Recommendations For Preventing Transmission Ofhuman Immunodeficiency Virus And Hepatitis B Virus To Patientsduring Exposure
This document has been developed by the Centers for DiseaseControl to update recommendations for prevention oftransmission of human immunodeficiency virus and hepatitisB virus in the health-care setting. Current data suggestthat the risk for such transmission from a health-care worker to a patient during an invasive procedure is small aprecise assessment of the risk is not yet available. Thisdocument contains recommendations to provide guidance forprevention of HIV and HBV transmission during those invasiveprocedures that are considered exposure-prone.INTRODUCTION
Recommendations have been made by the Centers for DiseaseControl for the prevention of transmission of the humanimmunodeficiency virus and the hepatitis B virus inhealth-care settings . These recommendations emphasizeadherence to universal precautions that require that blood andother specified body fluids of all patients be handled as if theycontain blood-borne pathogens .
Previous guidelines contained precautions to be used duringinvasive procedures and recommendations forthe management of HIV- and HBV-infected health-care workers . These guidelines did not include specificrecommendations on testing HCWs for HIV or HBV infection, andthey did not provide guidance on which invasive procedures mayrepresent increased risk to the patient.
The recommendations outlined in this document are based onthe following considerations:
-
Infected HCWs who adhere to universal precautions and who
Exposure-Prone Procedures
Recommended Reading: Hepatitis B Vaccine For Newborns Pros And Cons
How Do I Get Hepatitis B Treatment
Usually for adults, hepatitis B goes away on its own and you wont need treatment. Your doctor might tell you to rest, eat well, and get plenty of fluids. You may also get medicines to help with any symptoms you might have but be sure to talk with your doctor or nurse before taking anything.
If you have chronic hepatitis, there are medicines you can take to treat it. Your doctor will tell you about your options and help you get whatever treatment you need.
Risks To Patients From Hiv And Hepatitis B
It was recognised in the early 1970s that patients were at risk of acquiring hepatitis B infection by iatrogenic transmission from an infected health care worker. Infection may be transmitted by either a chronic carrier of hepatitis B or an asymptomatic health care worker who is incubating the disease. Procedures such as injections, dental surgery and general and gynaecological surgery have all been implicated. There have been at least 12 clusters of hepatitis B infections associated with infected health care workers in England, Wales and Northern Ireland and at least 20 published reports of the transmission of hepatitis B from infected health care workers to their patients worldwide. Despite immunisation and screening of health workers, the transmission of hepatitis B from health care workers to patients has been reported recently.,
There have been only two reports of transmission of HIV from infected health care workers to their patients., This is consistent with HIV having both a lower seroprevalence and a lower infectivity than hepatitis B. The risk of transmission of HIV from a clinical care worker is approximately 100 times less than that of hepatitis B. However, the two infections pose a similar overall risk to patients because HIV carries a risk of death approximately 100 times greater than hepatitis B.
Table 1
Don’t Miss: Can Hepatitis B Kill You
Which Is Worse Hepatitis B Or C
The scary thing about liver conditions like hepatitis is that you may be living with it and not even be aware.
Less than half of the people living with hepatitis B or hepatitis C are diagnosed. If you are one of these people living with an undetected case of hepatitis, you may be at risk for developing liver failure or liver cancer and transmitting the illness to other people.
What are the most common hepatitis infections? Is hepatitis B worse than hepatitis C? How is hepatitis detected and treated? Michael D. Cook, certified physician assistant at Gastroenterology Associates of Southwest Florida answers these questions and can help you understand the risks of hepatitis.
Why Getting Tested Is Important
A blood test is one of the only ways to confirm a diagnosis of hepatitis C. Additionally, hepatitis C often has no visible symptoms for many years.
Because of this, its important to be tested if you believe youve been exposed to the virus. Getting a timely diagnosis can help ensure you receive treatment before permanent liver damage occurs.
Recommended Reading: What Is Hepatitis B Surface Ag
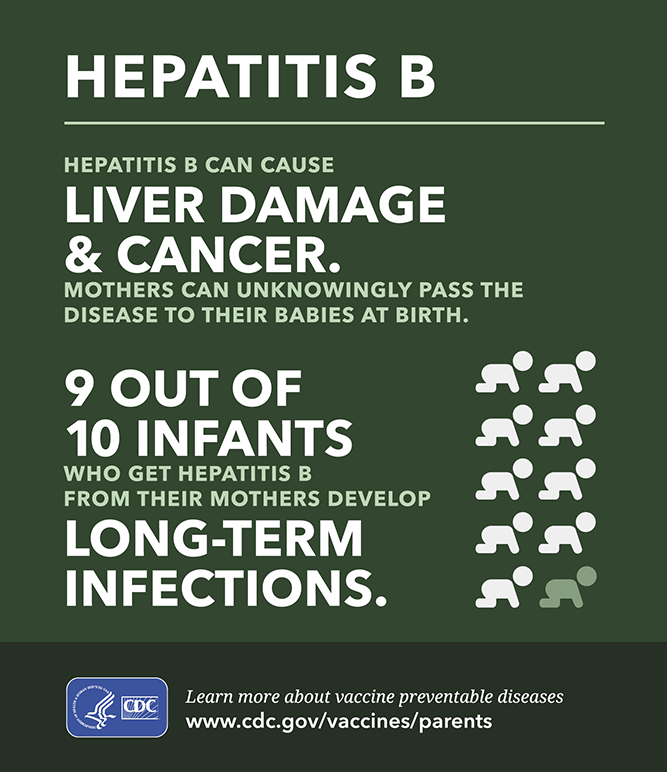
Hepatitis B And Pregnancy
If youâre pregnant, you might pass the virus to your baby at birth.
If your baby gets the virus and isnât treated, they could have long-term liver problems. All newborns with infected mothers should get hepatitis B immune globulin and the vaccine for hepatitis at birth and during their first year of life.
What Is The Outlook For People With Hepatitis B
The outlook for people with HBV is better now than ever before. You are certainly able to live a full life and help yourself stay healthy. You should make sure to have regular check-ups with a healthcare provider who is qualified to treat hepatitis B, possibly a liver doctor.
Make sure you are vaccinated against hepatitis A. Check with your healthcare provider or pharmacist before taking other medications or over-the-counter products, including supplements and natural products. These could interfere with your medication or damage your liver. For instance, taking acetaminophen in large doses may harm your liver.
Follow the usual guidelines for living a healthy life:
- Eat nutritious foods, choosing from a variety of vegetables, fruits and healthy proteins. It is said that cruciferous vegetables are especially good at protecting the liver.
- Exercise regularly.
- Dont smoke and dont drink. Both tobacco and alcohol are bad for your liver.
- Do things that help you cope with stress, like journaling, talking with others, meditating and doing yoga.
- Avoid inhaling toxic fumes.
You May Like: How Do People Get Hepatitis C
Hiv And Hepatitis B And Hepatitis C Coinfection
Hepatitis B and hepatitis C are liver infections caused by a virus. Because these infections can be spread in the same ways as HIV, people with HIV in the United States are often also affected by chronic viral hepatitis.
Viral hepatitis progresses faster and causes more liver-related health problems among people with HIV than among those who do not have HIV. Liver disease, much of which is related to HBV or HCV, is a major cause of non-AIDS-related deaths among people with HIV.
Given the risks of hepatitis B or hepatitis C coinfection to the health of people with HIV, it is important to understand these risks, take steps to prevent infection, know your status, and, if necessary, get medical care from a health care provider who is experienced in treating people who are coinfected with HIV and HBV, or HIV and HCV.
What Occupations Have Increased Risk Of Hepatitis B
In general, occupational groups with increased risk include:
- Health-care workers repeatedly exposed to blood or blood products or those who are at risk of needlestick injury.
- Pathologists, laboratory personnel, or embalmers.
- Dentists, dental assistants, and dental hygienists.
- Certain staff members of institutions for the developmentally handicapped.
- Staff of institutions where workers may be exposed to aggressive, biting residents.
Travellers to regions with intermediate or high rates of endemic HBV infection may also consider being vaccinated.
Recommended Reading: What Is Hepatitis 1 And 2
How Is It Treated
There is no specific treatment or cure for hepatitis B, but the infection often goes away on its own. Rest and a diet high in protein and carbohydrates help the liver repair itself. Most hepatitis cases are acute, and the infection lasts from 1 to 6 months, during which time the person is continually infectious. During this period of infection, alcohol and medications metabolized by the liver must be avoided and sexual activity is not recommended in order to prevent transmission to partner. And although 90% to 95% of adults with hepatitis B recover completely, 5% to 10% develop chronic cases of hepatitis B. This means that the infected person continues to be highly contagious. Alpha interferon and lamivudine are two drugs licensed for the treatment of persons with chronic hepatitis B. These drugs are effective in up to 40% of patients, however, approximately 15 to 25% of chronic cases develop severe liver disease and death.
Caregivers must also protect themselves from direct, ungloved contact with blood and other body fluids of infected individuals. If your sex partner or a member of your household is found to have hepatitis B, you should consult your medical provider to be vaccinated.
How Are Hepatitis B And Hepatitis C Spread From Person To Person
Like HIV, the hepatitis B and hepatitis C viruses spread:
- Perinatally: Pregnant people can pass these infections to their infants. HIV-HCV coinfection increases the risk of passing on hepatitis C to the baby.
- Sexually: Both viruses can also be transmitted sexually, but HBV is much more likely than HCV to be transmitted sexually. Sexual transmission of HCV is most likely to happen among gay and bisexual men who have HIV.
Recommended Reading: Hepatitis B Vaccine Rite Aid
Unresolved Issues And Recommendations
It is unclear at the moment whether or not the high prevalence of HIV in sub-Saharan Africa will increase the pool of highly viraemic HBV carriers, result in poor response to the HBV vaccine in HIV-positive babies, result in vaccine failures in babies born to HIV and HBV co-infected mothers, perhaps leading to the emergence of vaccine-escape mutants because of sub-optimal response to the HBV vaccine or perinatal transmission, modify HBV disease presentation or progression, complicate laboratory diagnosis of HBV infection, or complicate PEP and treatment for chronic HBV. This information can only be obtained through continuous surveillance of the effectiveness of immunisation programmes, as well as studies to monitor other prevention and control measures of HBV infection throughout the region. It is also important to monitor whether HIV immunosuppression may compromise the efficacy of the other vaccines within the EPI as well. This would provide added support for treatment of all AIDS cases with anti-retrovirals, and would increase the urgency of developing a vaccine for HIV.
Sport And Transmission Of Hiv And Hepatitis
The risk of transmission of HIV or hepatitis B or C from an infected player is:
- negligible for other athletes and players involved in contact sports
- negligible for first aid officers who follow infection control guidelines
- zero for coaches, trainers, officials and spectators.
HIV and hepatitis B and C cannot spread through:
- sweat or saliva from other sportspeople
- sharing drink bottles with team members
- hugging or shaking hands.
Recommended Reading: How You Know If You Have Hepatitis