The Difference Between Active And Latent Acute Porphyria
It is important to know that ~80% of people who have changes in their Porphyria genes never have symptoms of the acute Porphyrias. These people are said to have latent acute Porphyria.
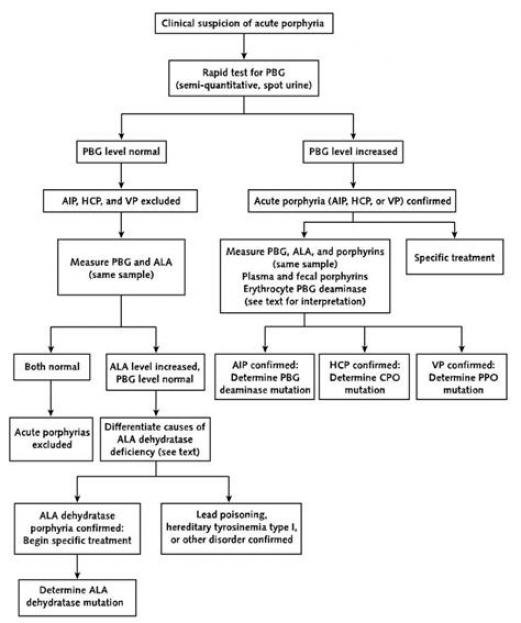
If someone has a mutation in an acute Porphyria gene and reports symptoms similar to an acute attack, their urine PBG level should be checked. If the urine PBG level is normal then there is likely another cause to this persons symptoms. Acute attacks are distinguished from other conditions that cause abdominal pain by very high PBG levels.
Acute Hepatic Porphyria Is A Rare Disease That Can Manifest Itself Differently From Person To Person It Has A Wide Range Of Debilitating Symptoms That Are Often Similar To Those Of Other Diseases Making Diagnosis Difficult
Knowing how to recognise certain signs and being aware that there are people more at risk of falling ill, as well as preventive remedies and treatment centres to rely on, is an important step in combating this disease.
On livingwithporphyria.eu/en you can find a lot of useful information to understand the complex nature of this disease and the ideal path to a timely diagnosis and a better quality of life.
Diagnosing Acute Hepatic Porphyria
The type of test that should be done depends on whether the person is having symptoms at the time. When a person is having symptoms from AHP, a spot urine test for porphobilinogen , a porphyrin, may be used. This test simply involves urinating in a specimen container, often a small cup. The sample is then tested in the lab for PBG levels. If PBG levels are high, a healthcare provider can tell that a person has AHP.
Other tests that may be done include a urine test for aminolevulinic acid as well as testing for total porphyrins in the urine, blood, or stool. If someone has severe kidney disease, a blood test for PBG may also be done. This is due to the kidney being unable to properly filter urine. As AHP is caused by a gene defect, genetic testing can also be used to diagnose the condition. Unlike the urine tests mentioned above, the genetic test can be done when a patient is not experiencing symptoms. Genetic testing is also helpful for diagnosing the condition in family members of those with known AHP. The genetic test looks for problems in 4 different genes and can diagnose the specific type of AHP that one may have .
Don’t Miss: How Do You Get Hiv And Hepatitis
Ner With Your Dedicated Support Team
A dedicated Alnylam Case Manager
When you and your healthcare provider choose to begin treatment with GIVLAARI, you will be partnered with a dedicated Alnylam Case Manager. Case Managers are experienced in helping individuals get started on treatment and providing ongoing support. They will tailor their level of contact based on your personal needs.
A dedicated Alnylam Patient Education Liaison
Our Patient Education Liaisons have backgrounds in nursing and are experienced in educating people and their families about matters related to AHP. Your PEL can help you in a variety of ways, such as:
The purpose of the Alnylam Patient Education Liaisons is to provide education to patients, their families, and caregivers. PELs are employees of Alnylam Pharmaceuticals. They are not acting as healthcare providers and are not part of your healthcare team. PELs do not provide medical care or advice. All diagnosis and treatment decisions should be made by you and your doctor.
Do not use GIVLAARI if you have ever had a severe allergic reaction to GIVLAARI.
GIVLAARI can cause:
-
Severe allergic reaction
Tell your doctor or nurse right away if you experience any of the following signs or symptoms of a severe allergic reaction during treatment:
- Swelling mainly of the lips, tongue or throat which makes it difficult to swallow or breathe
- Breathing problems or wheezing
Liver problems
Your doctor will check your liver function by doing blood tests:
What Are The Different Types Of Acute Hepatic Porphyria
The different types of AHP represent different enzymes that are missing. They fall under the sub-type of acute hepatic porphyria because they begin in your liver and because theyre characterized by sudden attacks of symptoms. In order of most common to least common, they are:
- Acute intermittent porphyria . A mutation in the HMBS gene causes a deficiency in the enzyme hydroxymethylbilane synthase , also known as porphobilinogen deaminase . It can be a new mutation or inherited as an autosomal dominant trait.
- Variegate porphyria . A mutation in the PPOX gene causes a deficiency in the enzyme protoporphyrinogen oxidase . It can be a new mutation or inherited in an autosomal dominant pattern.
- Hereditary coproporphyria . A mutation in the CPOX gene causes a deficiency in the enzyme coproporphyrinogen oxidase . It can be a new mutation or inherited in an autosomal dominant pattern.
- ALAD-deficiency porphyria . A mutation in the ALAD gene causes a deficiency of the enzyme delta-aminolevulinic acid dehydratase . Its inherited as an autosomal recessive trait.
How does acute hepatic porphyria affect me?
Who does acute hepatic porphyria affect?
How common is acute hepatic porphyria?
Recommended Reading: What Happens If You Have Hepatitis C
How To Diagnose Acute Hepatic Porphyria
Many of the signs and symptoms of Acute Porphyria Hepatica are strikingly similar to those of other more common conditions, such as irritable bowel syndrome, Crohns disease, endometriosis, fibromyalgia and certain psychiatric disorders.
These similarities very often make it difficult to obtain a correct diagnosis quickly, with the risk of intercepting different specialists and accumulating delays in treatment, or worse, running into incorrect treatment that can lead to serious consequences for the patient.
Improving the diagnosis of the disease is, however, possible by relying on a specialised centre so as to overcome the problems associated with the initial phase of the diagnostic process, as well as speeding up the time taken to perform examinations, surveillance and treatment of porphyria.
Most Common Symptoms Of Acute Hepatic Porphyria
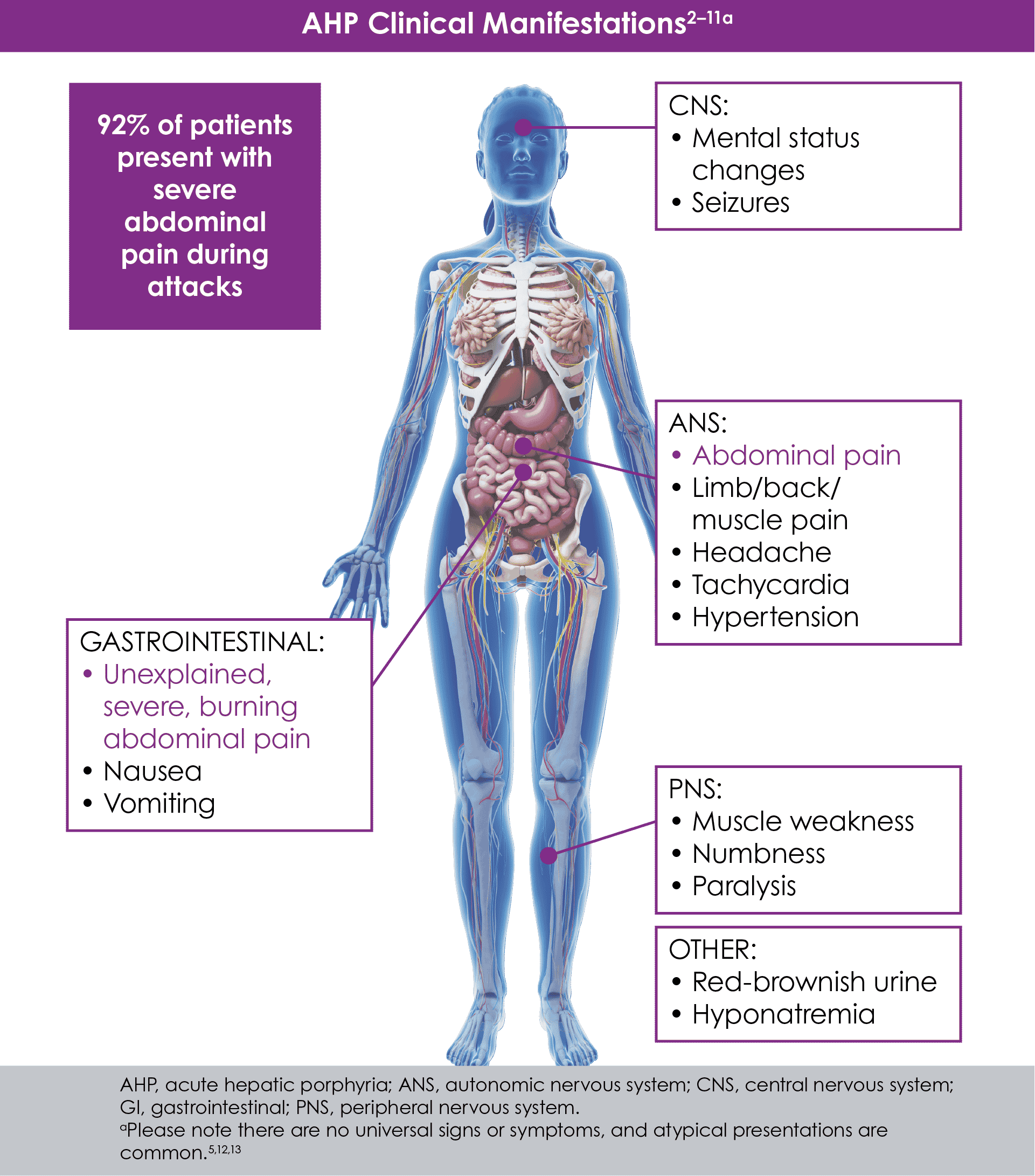
People with AHP can experience gastrointestinal, neurologic, psychiatric, cardiovascular, or skin symptoms. The most common symptom is abdominal pain which can be severe and last several hours.
Those with AHP can also experience chronic symptoms. These are symptoms that last a long time and may include:
- fatigue- feeling overly tired or having low energy
- nausea- feeling of sickness in the abdomen, stomach, chest, or head with feeling an urge to vomit
- pain physical discomfort and/or suffering in the body
Recommended Reading: What Is Non Reactive Hepatitis C
What Are The Symptoms Of Acute Hepatic Porphyria
Symptoms of AHP are often baffling to those who experience them as well as to their healthcare providers. They can strike suddenly and severely and seem to be unconnected to each other. Symptoms can include pain in different areas of the body, problems with your digestive system and severe skin reactions to sunlight. They can also include cognitive and sensory changes related to your nervous system.
Nerve pain may affect different areas of your body, including:
People with variegate porphyria or hereditary coproporphyria may develop skin reactions to sunlight, such as:
Finally, porphyria can change the color of your urine. Leftover porphyrin precursors that build up in your body and pass through your pee may give it a reddish-purple color. .
What is an acute hepatic porphyria attack?
Most people with symptomatic AHP experience their symptoms as occasional acute attacks. These may be more or less frequent or severe for different people. They usually last a few days and get progressively worse before getting better. Severe and frightening symptoms may bring you to the emergency room, and some of these can be medical emergencies. For example, respiratory paralysis can make breathing difficult.
What are the most common symptoms of an AHP attack?
How Should I Take Care Of Myself While Living With Ahp
- Avoid common triggers. Alcohol, smoking and drugs should be at the top of your list to avoid. You might need to consult your doctor about alternatives to certain prescription medications.
- Maintain a healthy, well-balanced diet. Avoid extreme dieting and low-carb diet plans. Consult your doctor before fasting for a medical test or procedure.
- Get your regular checkups. Even if you dont have symptoms, your healthcare provider will need to check on your liver, kidneys and blood pressure periodically.
A note from Cleveland Clinic
Acute hepatic porphyria is rare, and general awareness of the condition is low. When acute symptoms strike in a sudden attack, they can be confusing and frightening. Some people spend years trying to find out what might be wrong with them and what might help. If you suspect you might have AHP, genetic testing can confirm it. Once you know, youll be in a better position to prevent and manage attacks.
Last reviewed by a Cleveland Clinic medical professional on 08/30/2022.
References
Recommended Reading: Hepatitis C Symptoms In Males And Females
How Ahp Is Diagnosed
People who may be experiencing symptoms can discuss AHP testing with their healthcare provider. The technique a doctor can use to determine if a person has AHP is the random urine test, to determine if there are elevated PBG and ALA levels. A genetic test is not required for diagnosis, though it is recommended to specify the type of AHP.1-3
Acute Hepatic Porphyria: Pathophysiological Basis Of Neuromuscular Manifestations
- Division of Neuromuscular Diseases, Department of Neurology and Neurosurgery, Federal University of São Paulo , São Paulo, Brazil
Acute hepatic porphyria represents a rare, underdiagnosed group of inherited metabolic disorders due to hereditary defects of heme group biosynthesis pathway. Most patients have their definite diagnosis after several years of complex and disabling clinical manifestations and commonly after life-threatening acute neurovisceral episodes or severe motor handicap. Many key studies in the last two decades have been performed and led to the discovery of novel possible diagnostic and prognostic biomarkers and to the development of new therapeutic purposes, including small interfering RNA-based therapy, specifically driven to inhibit selectively delta-aminolevulinic acid synthase production and decrease the recurrence number of severe acute presentation for most patients. Several distinct mechanisms have been identified to contribute to the several neuromuscular signs and symptoms. This review article aims to present the current knowledge regarding the main pathophysiological mechanisms involved with the acute and chronic presentation of acute hepatic porphyria and to highlight the relevance of such content for clinical practice and in decision making about therapeutic options.
Don’t Miss: How Long Does Hepatitis B Last
What Are Some Symptoms Of Ahp
AHP can cause a wide range of symptoms that mimic those of other diseases, and some people with a defective gene associated with AHP may not have any symptoms whatsoever. People with AHP who experience symptoms can suffer from severe attacks that are often unpredictable and include very painful abdominal pain. Some people may also experience chronic symptoms such as pain in between attacks. Most people have at least one other symptom in addition to the belly pain. Some of these symptoms may include:
- Nausea and vomiting
- Skin blistering
The various symptoms of AHP can lead to physical and emotional suffering and exhaustion. This can affect every aspect of life, including overall physical comfort the ability to work consistently and maintaining a healthy level of social connectedness with others.
Clarification Of Testing Results
It has come to our attention that some patients who have been diagnosed clinically as having Acute Intermittent Porphyria or another Acute Hepatic Porphyria could not be confirmed by either biochemical or DNA testing. Biochemical testing is the demonstration of increased urinary ALA and PBG, and these values are highest during an acute attack when patients are symptomatic. Some patients can have high levels in between attacks as well, but not all. Positive diagnostic values should be increased greater than 5 times normal, not just a slight increase which can occur with dehydration. Most commercial laboratories and in particular the Porphyria Lab at the University of Texas Medical in Galveston which is run by Dr. Karl Anderson, will perform these tests properly. It is important that the doctor order urinary ALA and PBG and not a “porphyrin profile.”
Recommended Reading: What Is The Cure For Hepatitis A
The Erythropoietic Cutaneous Porphyrias
The erythropoietic cutaneous porphyrias, congenital erythropoietic porphyria and EPP, and its recently recognized X-linked form, XLP, are characterized by elevations of porphyrins in bone marrow and erythrocytes and usually present with cutaneous photosensitivity in infancy or early childhood,, or in the case of CEP, even in utero as nonimmune hydrops fetalis.
Acute Motor Axonal Neuropathy
Acute flaccid paralysis presenting as acute to subacute symmetric proximal quadriparesis due to motor axonal polyradiculopathy or neuronopathy represents the most common neuromuscular presentation of AHP in the Emergency Department and Intensive Care Unit , resembling clinical and neurophysiological features of GuillainBarré syndrome and representing one of the main factors for medical and financial burden of AHP .
Classically, the peripheral neuropathy in AHP usually starts with muscle pain and weakness commonly preceded by abdominal pain and psychiatric disturbances that may further progress over a 2-week period for tetraplegia or death, with some patients requiring mechanical ventilation due to paresis of respiratory and bulbar muscles. The acute motor axonal neuropathy can occur in up to 68% of patients and is usually symmetric and starts in the upper limbs with frequent association with autonomic disturbances. Cranial nerve involvement is more rarely observed, and sensory neuropathy is usually identified by mild distal lower limb paresthesias or with a painful bathing suit proximal distribution. Some patients may disclose permanent quadriplegia after severe acute attacks, even after proper early therapy introduction .
The motor symptoms in the context of a chronic motor axonal neuropathy in AHP are associated with irreversible damage or severe compromise to the axonal compound of the peripheral nerve after acute decompensation .
Don’t Miss: Can Hepatitis C Cause Low Platelets
Deterrence And Patient Education
During an acute attack, potentially harmful medications should be discontinued whenever possible. It is strongly advised for clinicians to consult the websites of the American Porphyria Foundation and the European Porphyria Network , which list many medications, including those that are not classified with certainty provide evidence for these classifications, and are regularly updated. Also, these websites should be consulted to avoid prescribing harmful medications in treating concurrent illnesses or symptoms.
Potentially harmful lifestyle factors include smoking and alcohol use. Patients should be counseled to avoid or discontinue smoking, including the use of marijuana, and to avoid alcohol intake. Smoking and alcohol use can both exacerbate acute hepatic porphyrias via induction of hepatic cytochrome P450 enzymes , which, in turn, can diminish the pool of hepatic heme and directly induce enzymes in the porphyrin pathway, leading to increased synthesis of toxic heme precursors.
Acute attacks are also associated with sex hormones , decreased caloric or carbohydrate intake , and metabolic stress due to infections or other illnesses.
How Is Acute Hepatic Porphyria Treated
Treatment for AHP is focused on preventing and managing symptom attacks. During an attack, you may need hospital care. You may need various medications to reduce your different symptoms. Between attacks, you may need different medications to keep your triggers in check. Treatment is more effective when you and your healthcare provider are able to identify which triggers affect you the most.
Treatment for an acute attack may include:
- Hemin injection. During a severe attack, a doctor may give you hemin through an injection into your vein to help reduce the porphyrins in your blood. Hemin is a salt derived from red blood cells that inhibits porphyrin production in your body.
- Pain relief. You may need strong pain relievers, such as opioids, during an acute attack.
- Phenothiazines. These drugs can control severe nausea and vomiting.
- IV fluids and nutrition. Symptoms such as abdominal pain, nausea, vomiting, diarrhea and constipation may deprive your body of calories and hydration during an attack. AHP can also cause deficiencies in sodium and magnesium. You may receive IV fluids containing carbohydrates and electrolytes.
- Seizure medications. Up to 20% of people may need treatment for seizures during an attack.
Long-term treatment options may include:
Read Also: When Should You Get Hepatitis A Vaccine
What Is Acute Hepatic Porphyria
Acute hepatic porphyria is a group of rare genetic disorders that begin in your liver and go on to affect your nervous system, causing symptoms throughout your body. Symptoms occur when toxic compounds build up in your liver and then pass into your bloodstream, where they come into contact with your nerves. There are four different types of AHP, representing half of the eight types of porphyria that affect different organs.
Porphyria is a deficiency in one of the enzymes that your body needs to make heme . During the process of making heme, the absence of specific enzymes causes other compounds to go unused and build up in your body tissues. These leftover compounds called porphyrin precursors are toxic when they build up. In acute hepatic porphyria, they build up in your liver first.
Blood Testsplasma Or Serum
Plasma total porphyrins is a very useful and underutilized test when a Porphyria is suspected as a cause of photosensitivity. Normally there are only trace amounts of porphyrins in plasma, and the amounts increase markedly in patients with cutaneous Porphyrias. Being both sensitive and specific, plasma porphyrin concentrations are increased in any patient with skin problems related to any type of Porphyria and are seldom increased in other conditions.
The preferred method, at least for screening, involves diluting plasma with a nonacid, neutral buffer and measuring the porphyrins directly by fluorescence scanning. This can serve not only as a rapid screening method for all cutaneous Porphyrias but can determine whether a patient has VP rather than PCT and other Porphyrias that can cause blistering skin lesions. This method also detects some cases of latent VP.
Plasma porphyrin measurements may be less useful for detecting EPP than other cutaneous Porphyrias. One reason for this may be that protoporphyrin is very light sensitive, and the concentration in the sample can decrease rapidly if it is exposed to light during processing. Therefore, erythrocyte porphyrins should be measured if EPP is strongly suspected.
Also Check: What Is Hepatitis C Antibody Test