Who Gets Anemia From Hepatitis C
Drugs used to treat hepatitis C, particularly interferon and ribavirin, can cause anemia.
Interferon suppresses the production of new red blood cells in bone marrow. Ribavirin destroys red blood cells by causing them to break open, or rupture.
Newer hepatitis C drugs, such as boceprevir , also have anemia as a side effect. Taking boceprevir with interferon and ribavirin can lead to even more severe drops in hemoglobin levels.
Youre also more likely to develop anemia if you have one of these conditions:
- bleeding in the GI tract from a peptic ulcer
- blood loss from an injury
- cirrhosis of the liver
Baseline Characteristics Of Studied Population
Totally, 946 males and 357 females were included in the present study, with a mean age of 49.64±8.15 years and 48.87±7.65 years, respectively. Among them, 454/946 males were diagnosed as NAFLD, which was significantly higher than those in females . As the results shown, the mean platelet count in the NAFLD and non-NAFLD subjects was 220.6±42.22 and 213.2±43.26 at baseline, respectively. There was a statistical difference between two groups . In addition, NAFLD and non-NAFLD subjects differed significantly in many parameters, such as BMI, ALT, AST, LDL-C, HDL-C and TG. Clinical and biochemical characteristics of study population were summarized in Table .
Table 1 Baseline characteristics of the study participants stratified by NAFLD
Joint And Muscle Pain
A condition called arthralgia causes joint pain and is common in people with hepatitis C. Itâs different from arthritis, which causes pain and swelling in joints. But infected people can also get hepatitis C-related arthritis.
Fibromyalgia, which causes body aches and muscle pain, is also common in people with hepatitis C.
You May Like: What Is Hepatitis B And C Virus
Trapped Platelets By Enlarged Spleen Causing Low Platelets In Circulation
The platelets made inside bone marrow and face their fate in the spleen, a number of diseases can enlarge our spleen:A child with Infection mononucleosis will suffer from spleen enlargement splenomegaly and show such blood count results:Total leukocyte count TLC 17,000,Plt 100 cells/cumm Monocyte count 20% Lymphocyte count 60%EBV IgM Positive 2.5 .A 50 years old man with liver cirrhosis or cystic fibrosis, can have his spleen to be enlarged and harbor too many platelets which causes platelets test to show decreased number.To recognize such a case you may show some of these results in your testing report:Liver enzymes SGOT 20 SGPT 25, albumin 2.5 , High liver enzyme count explainedHemoglobin 10.0 g/dL,Platelets 70,
Thrombocytopenia In The Hospitalized Patient
Thrombocytopenia may complicate the course of the hospital stay of patients with a variety of medical and surgical problems. In one study, thrombocytopenia was observed in approximately 1% of adult inpatients in an acute care hospital. However, less than 30% of these patients presented with bleeding manifestations. As expected, thrombocytopenia is much more common in ICUs, where it is found in in 8%-68% of patients on admission, and in 13%-44% of patients during the stay in the unit. Many potential etiologies are often concomitant in the acute care setting , and it is not always possible to elucidate the cause of the thrombocytopenia. However, because of its frequency, consideration should always be given to DITP. The frequency of DITP in critically ill patients is approximately 20%. Antibiotics in this setting are a frequent etiology., Tests for the detection of drug-dependent antiplatelet Abs are not widely available, are time-consuming, and are not sensitive enough to be incorporated in a diagnostic algorithm for the urgent management of patients with severe thrombocytopenia. The decision to discontinue a potential causative drug in such cases should rely solely on clinical criteria.
Read Also: Is There A Vaccine For Hepatitis B
Baseline Characteristics Of The Subjects In The Community
The basic demographic and clinical characteristics of the 11,239 study participants are shown in Table 1. Eighty-four subjects were positive for both HBsAg and anti-HCV. The prevalence of HBsAg and anti-HCV were 13.7% and 6.3% , respectively. The prevalence of obesity, abnormal ALT and low platelet count was 21.9%, 20.3% and 4.2%, respectively. After being recalled, 642 anti-HCV-positive subjects received further tests for serum HCV
How To Diagnose Low
Diagnosing thrombocytopenia may be a multi-step process that starts with a visit to the doctor. You may have visited the doctor to address another issue, or perhaps were noticing symptoms like unexplained bruising or rashes.
First, the doctor will ask you about any over-the-counter medicines or herbal supplements you may be using, or if you regularly drink beverages containing quinine.
They will likely continue to ask questions regarding eating and drinking habits, as well as assess your HIV/AIDS risk. You can also expect the doctor to feel around your abdomen for signs of an enlarged spleen, and take note of other symptoms that could signal an infection .You may be required to see a hematologist to analyze blood samples via a couple of different testsblood smears and marrow healthto provide a proper diagnosis.
Essentially, you will not be able to diagnose thrombocytopenia on your own you will need a medical healthcare professional.
Don’t Miss: Natural Ways To Cure Hepatitis C
Causes During Cancer Treatment
The most common cause of thrombocytopenia in people with cancer is bone marrow suppression related to chemotherapy. Chemotherapy destroys rapidly dividing cells, such as those in the bone marrow which become platelets.
In addition to thrombocytopenia, bone marrow suppression from chemotherapy may result in a low red blood cell count and a low level of the type of white blood cells known as neutrophils which defend against bacterial infections.
Reasons Accelerate Breakdown Of Platelets By Spleen And Cause Shortage Of Platelets In Your Blood
Examples of such conditions include:Low platelets count in Pregnancy : pregnant woman consume nutrients more than the normal female, thus the body uses more vitamins and proteins inside cells to enrich fetus, the reasons behind high destruction of platelets and platelets to be low during pregnancy, but its mild and improves after delivery of baby.blood results may come like this:Beta sybunit HCG hormone 150,000, do you know what is B-HCG?Hemogobin 9.4Total leucocyte count shows mild leucocytosis and absolute neutrophilia
Don’t Miss: Where To Get Hepatitis B Titer
Treatment Of Low Platelets
It is important to identify the cause of low platelets. When the cause is clear, treatment can usually help your levels return to normal.
If you are receiving therapies that affect your platelet count, such as cancer treatment, your platelets should return to normal once the treatment ends. Keep in mind that the timeline is different for everyone.
In some cases, a platelet transfusionmay be needed. This is a procedure where you receive platelets from a donor through a vein. A transfusion can help prevent complications from bleeding.
Autoimmune conditions can be treated with drugs that suppress your immune system. This will help stop the destruction of platelets.
When low platelets are caused by medication, the solution is often just switching medications. Your doctor will help you find the right alternative drug.
Inf Based Antiviral Therapy
Although IFN based antiviral therapy is uncommonly used in developed countries nowadays, the prohibitive cost of DAA may require the use of INF based therapy along with the addition of thrombopoietin mimetics, if required, in economically disadvantaged areas. Additionally, in chronic hepatitis C cases treated with pegylated INF plus ribavirin, single nucleotide polymorphisms at or near the IL-28B gene have been shown to be a predictor of SVR., The American Gastroenterological Association recommends dose reduction of INF with a platelet count between 25,000â50,000 and withdrawal of INF-based treatment with a count below 25,000. This is important because the antiviral therapy itself may cause a further drop in platelet count. Studies have shown IFN-based therapy to cause severe thrombocytopenia in up to 13% of patients, with the incidence higher in patients with lower baseline platelet count., The modifications in IFN-based therapy have potential to lower the chances of attaining SVR. The increased risk of bleeding may also impede the initiation and maintenance of different invasive diagnostic and therapeutic procedures such as liver biopsy, variceal banding, paracentesis and thoracentesis, central line insertion, endoscopy and elective surgery.
Don’t Miss: What Are The Signs Of Hepatitis
Who Should Not Get The Hepatitis B Vaccine
Generally seen as a safe vaccine, there are some circumstances in which doctors advise against receiving the HBV vaccine. You shouldnt have the hepatitis B vaccine if:
- youve had a serious allergic reaction to a previous dose of the hepatitis B vaccine
- you have a history of hypersensitivity to yeast or to any other vaccine components
- youre experiencing a moderate or severe acute illness
If youre currently experiencing an illness, you should postpone receiving the vaccine until your condition has improved.
Impact On Clinical Management
Although thrombocytopenia in chronic HCV infection is typically low grade and not life-threatening, it represents an obstacle to different diagnostic or therapeutic modalities and may preclude the use of anti-viral treatment.
The greatest challenge in the care of chronic HCV patients with thrombocytopenia is the difficulty in initiating or maintaining IFN containing anti-viral therapy. Although this challenge can be avoided with the use of sole DAAs as the primary treatment modality, thrombocytopenia remains of particular interest, especially in cases of advanced liver disease. In a study by Wang et al., baseline thrombocytopenia increased the risk of drug cessation. Patients with baseline thrombocytopenia actually exhibited compromised sustained virologic response rates while those with acquired thrombocytopenia did not. Thus, use of growth factors to maintain SVR rate would be beneficial in those with baseline thrombocytopenia rather than in those who acquire it during therapy as dose reduction doesnât decrease SVR in such cases.16
Read Also: What Are The First Signs Of Hepatitis C
Incorporation Of World Health Organization And Macrobiotic Diet Recommendations
Incorporating elements of the macrobiotic diet and nutritional guidelines from the World Health Organization may increase platelet count. The macrobiotic diet and World Health Organization guidelines have been used to prevent and treat disease.
Nutrient recommendations include an adequate intake of calories and fresh whole foods. This includes plant-based proteins, healthy fats, fruits, and vegetables. Fewer animal products are consumed, while sugar, sodium, and saturated and trans fats are avoided.
Chemical pesticides, herbicides, additives, and preservatives may lower platelet counts. These diet recommendations incorporate foods without these compounds.
Read Also: Where To Get A Hepatitis B Shot
Observation Of The Peripheral Blood Smear
In the era of genomic medicine and widespread molecular testing, examination of the peripheral blood film still remains the most important investigation guiding our diagnostic approach to thrombocytopenia . All 3 blood cell lineages should be assessed carefully . From a practical perspective, when we are investigating thrombocytopenia in a critically ill patient, the immediate information we need to obtain is whether it is thrombotic microangiopathy or acute leukemia . Even a short delay in making these diagnoses may prove fatal for the patient if appropriate treatment is not initiated promptly.
Recommended Reading: Hepatica Herbal Liquid Extract Supplement
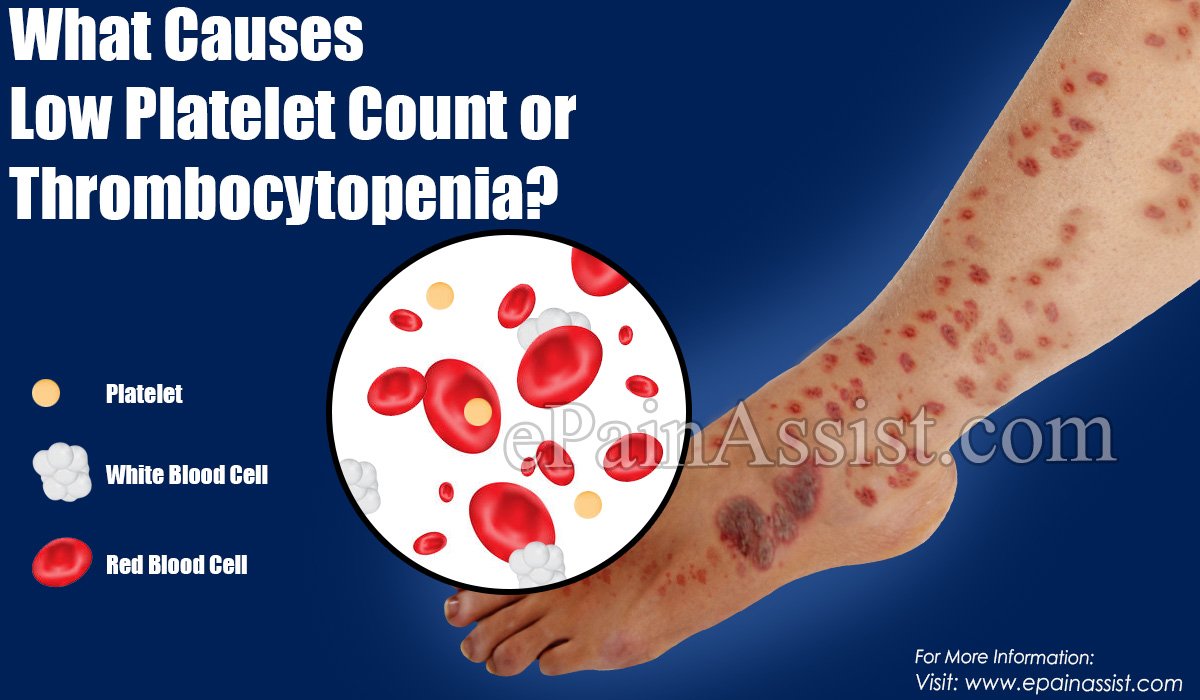
What Does Low Blood Platelets Count Mean
When you receive your blood test results and platelets count comes low in CBC test, that means:You dont have enough platelets in your blood which makes your body to be unable to form clots properly, you will have a tendency of bleeding upon injury more than the healthy person,Mild low platelets count is less significant and means transient state, pre-recovery, or variation of laboratories.However, in severe platelets deficiency you may show superficial bleeding in the skin that appears as a rash of tiny-sized purple spots , usually seen on the lower legs and forearms as well as excessive bruising Low Blood Platelet count doesnt necessarily mean you have a cancer, more blood tests for cancerso that please carefully read the possible reasons to understand your platelets level then you have the right to ask about your results.
purpura looks like on hand foot skin
What To Do If Bleeding Starts
Bleeding can be a serious concern in someone with a low platelet count. If you begin bleeding, contact your doctor at once. Follow these steps to minimize bleeding:
- Sit or lie down. Try to stay calm.
- Apply pressure to the wound if you can see it.
- Apply an ice pack to the site to slow the bleeding.
- If the wound is on an arm or leg, raise the limb above the level of your heart.
- If you see blood in your urine, increase your fluid intake and call your doctor at once.
- If you notice blood in your vomit, call your doctor. Take anti-nausea medications and antacids as instructed by your doctor.
- If you are bleeding vaginally, do not use tampons. Keep track of how many sanitary pads you are using. Note any clots.
Read Also: Hepatitis B And Liver Cancer
Sampling Of Eligible Subjects In The Community
From June 2002 to September 2005, we conducted a community survey project among the general population of the Kaohsiung area, a major metropolitan region located in southern Taiwan described previously . Of the 159,348 residents aged 4065 years, this project was planed to enroll 11,300 tested subjects. The study conformed to the ethical guidelines of the Declaration of Helsinki and was performed with the approval of the local research Ethics Committee.
Medications That Stimulate Platelet Formation
Medications are sometimes used to stimulate the bone marrow to make more platelets, though these are used infrequently in people who have thrombocytopenia due to chemotherapy, and there is currently little evidence to support their routine use.
The drug most commonly used is Neumaga , though the medications Nplate and Promacta are sometimes used, though approved for low platelet counts due to autoimmune conditions.
Don’t Miss: Ok Google What Is Hepatitis C
Blood And Vessel Problems
People with hepatitis C often get a condition called cryoglobulinemia. This happens when certain proteins in your blood stick together in cold weather. They can build up in vessels and block blood flow, which causes swelling and damage. The condition can affect your skin, organs, nerves, and joints.
Hepatitis C also can cause problems with blood itself. You may not make enough white blood cells, which fight infections, or platelets, which help your blood clot.
The infection can also make you bruise easily or get red or purple spots under your skin. Those are signs of a bleeding disorder called immune thrombocytopenic purpura.
The Increase Of The Platelet Count In Chronic Hepatitis C
Common causes of the increase of the platelet count in chronically HCV-infected patients are splenectomy, ribavirin treatment, and liver transplantation . But clinically evident thrombocytosis, usually defined as > 45×104/mm3, is rare in HCV patients receiving splenectomy or ribavirin monotherapy.
A platelet count augmentation can be observed after splenectomy in HCV-chronic infected patients and this increase persists for a long time.27 An increase of platelet count can be found in patients with chronic hepatitis C treated with ribavirin, which induces haemolytic anaemia followed by a rise in serum erythropoietin. A higher endogenous erythropoietin stimulates not only the erythrocytes production but also that of platelets. Such an augmentation was shown after 4 weeks of ribavirin monotherapy while TPO did not increase.28 IFN-related thrombocytopenia diminished in patients treated not only with IFN, but also with ribavirin, due to its thrombocytotic response.29 It was shown that rs1127354 and rs7270101 produce ITPase deficiency and defend against ribavirin-induced haemolytic anaemia. However, a platelet count reduction appeared in these patients.29 A reactive thrombocytosis , which begins within 8 weeks after LT, was observed especially when LT was made after a seronegative fulminant hepatic failure and was negatively associated with HCV-related liver cirrhosis. This thrombocytosis had a median duration of 25 days and did not raise the hepatic artery thrombotic risk.30
You May Like: How Do You Get Hiv And Hepatitis
Thrombocytopenia In The Cardiac Patient
Several mechanisms can induce thrombocytopenia in patients undergoing open heart surgery. Cardiopulmonary bypass may result in mechanical destruction of platelets, hemodilution in the bypass circuit, and drug-induced platelet destruction. More rare causes include sepsis, intra-aortic balloon pumping, and posttransfusion purpura. The nadir platelet count is typically seen on the second or third day after surgery, with a rapid platelet count recovery thereafter.
Severe thrombocytopenia is observed in 0.1%-2% of patients after exposure to GPIIb/IIIa inhibitors during percutaneous coronary intervention. The peculiarity of this DITP is its rapid onset, usually within a few hours after surgery. This phenomenon has been attributed to the presence of naturally occurring Abs against neoepitopes exposed by alteration of the GPIIb/IIIa molecule. In typical cases, thrombocytopenia resolves within 10 days. Delayed development of thrombocytopenia 3-6 days after treatment with abciximab has been described in a few patients. The mechanism of the thrombocytopenia in these cases is the production of Abs against murine peptide sequences of abciximab, which react with other target epitopes on abciximab-coated platelets.
Current Therapies For Hcv Infection
Approved treatments for HCV include IFN-2a and IFN-2b monotherapy, pegylated IFN-2a and PEG-IFN-2b monotherapy, and IFN-2b, PEG-IFN-2b, or PEG-IFN-2a in combination with ribavirin . Although IFN- monotherapy was the first approved treatment, results of randomized, controlled trials subsequently indicated that the addition of Rbv to IFN- produces improved sustained virologic response rates . An SVR is defined as the absence of HCV RNA 6 months after treatment. In 2 large, multicenter trials, the SVR rates for IFN- monotherapy at 24 and 48 weeks were 6% and 13%19%, respectively, whereas SVR rates with the combination of IFN- and Rbv at 24 and 48 weeks were 31%35% and 38%43%, respectively . In addition, preliminary evidence suggests that IFN-/Rbv combination therapy is effective for patients who experience relapse or do not respond to IFN- monotherapy . Combination therapy also produces a greater reduction in liver fibrosis than does IFN- monotherapy .
The current dosing practice for Rbv is weight based. Retrospective analysis has determined that maintenance of Rbv dosages > 10.6 mg/kg/day was associated with more-optimal SVR rates . Preliminary analysis from a prospective study of PEG-IFN-2a and Rbv demonstrated a higher SVR rate for patients infected with HCV genotype 1 who were randomly assigned to receive 10001200 mg/day Rbv than for those receiving 800 mg/day Rbv for 48 weeks .
You May Like: Blood Donation Hepatitis B Antibodies