Lets Stop Hiv Together: Hiv Testing
The HIV testing component of CDCs Lets Stop HIV Together campaignis designed to motivate all adults to get tested for HIV, making HIV testing part of everyones regular routine. It highlights the importance of everyone knowing their HIV status and knowing what their next steps should be depending on their status.
HASHTAGS:
Few Hiv Preventive Measures
Some HIV prevention programmes have been introduced in prisons in eastern Europe and central Asia. However, most countries in eastern Europe and central Asia offer few adequate HIV preventive measures in prisons, although they have been shown to be effective elsewhere, primarily in western European countries.Successful HIV preventive measures in prisons include provision of:
- HIV/AIDS education and information
- drug treatment and
- condoms.
Denying access to such measures places people in prisons at increased risk of HIV infection. It also places prisoners living with HIV at increased risk of declining health, coinfection with tuberculosis and hepatitis, and ultimately death.
The failure to implement comprehensive programmes known to reduce the risk of HIV transmission in prisons and to promote the health of prisoners living with HIV is often related to lack of political will, concerns about security and mistaken assumptions that such programmes will encourage injecting drug use and unsafe sexual behaviour. In addition, many governments lack the resources and technology to meet the overwhelming need. This public health crisis requires urgent attention and action.
How Hbv Is Spread
It is possible for the hepatitis B virus to be spread through the bodily fluids of an infected person, which is to say that the virus can be transmitted through the blood, sweat, tears, saliva, semen, vaginal secretions, menstrual blood, and breast milk of an infected person. That said, having hepatitis B does not necessarily mean that you are infectious only some people with HBV are actually contagious.
Opportunities for exposure can include sharing a syringe or getting tattoos or body piercings with infected tools. But it also means that it is possible to be exposed during childbirth as well as sexual contact and intercourse. In fact, nearly two-thirds of acute cases of hepatitis B in the United States are caused by sexual exposure.
Though HBV can be spread through blood, there is generally very little risk of contracting the virus through blood transfusions as most countries began screening for it by 1975.
Read Also: What Does It Mean To Have Hepatitis C Antibodies
What Is Ending The Hiv Epidemic In The Us
Ending the HIV Epidemic in the U.S. is a bold plan announced in 2019 that aims to end the HIV epidemic in the United States by 2030. Agencies across the U.S. Department of Health and Human Services developed an operational plan to pursue that goal accompanied by a request for additional annual funding.
The plan leverages critical scientific advances in HIV prevention, diagnosis, treatment, and outbreak response by coordinating the highly successful programs, resources, and infrastructure of many HHS agencies and offices. Initially, the initiative is focusing on areas where HIV transmission occurs most frequently, providing 57 geographic focus areas with an infusion of additional resources, expertise, and technology to develop and implement locally tailored EHE plans.
Mandatory Infection Prevention And Control Training For Hcp
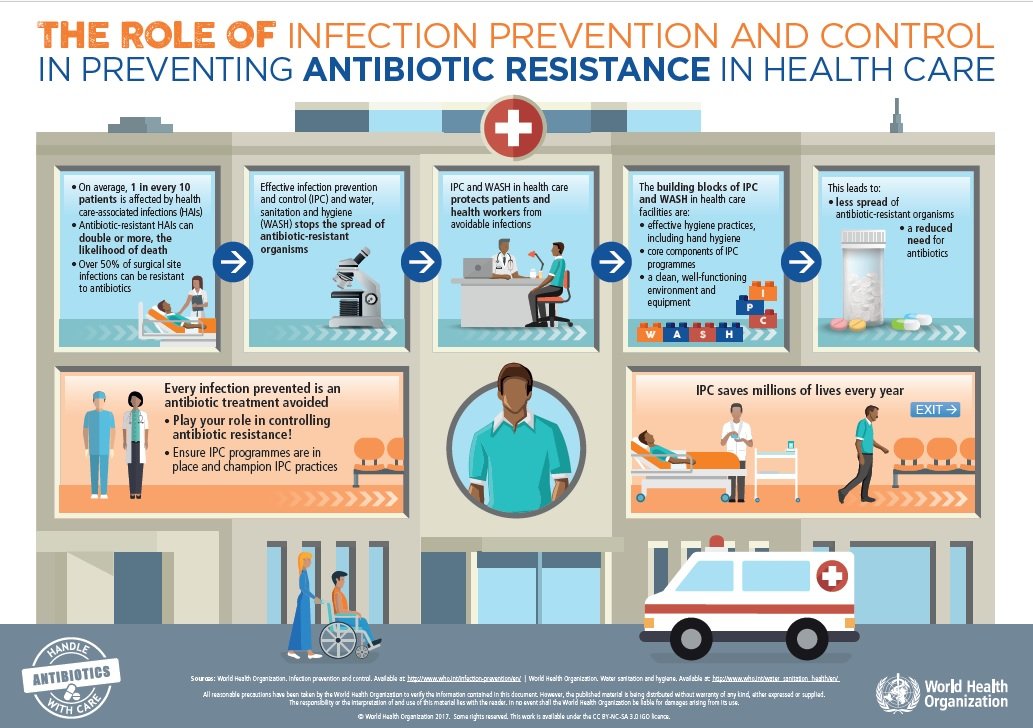
New York State regulation requires all licensed health care facilities to train their staff in infection prevention and control techniques, to provide appropriate equipment, and to enforce use of Standard Precautions in situations involving potential exposure to blood or other body fluids. The NYSDOH also provides detailed infection prevention and control guidelines to all physicians and dentists practicing in New York State and makes such guidelines publicly available on the NYSDOH website.
In addition, Public Health Law § 239 and Education Law § 6505-b require licensed health care professionals to complete a course in infection control and barrier precautions on or before July 1, 1994, and every four years thereafter. As of 2008, PHL § 239 also requires medical students, medical residents, and physician assistant students to complete coursework or training in infection control practices. Required courses, tailored to the infection prevention and control training needs of specific health care specialties, include work practices and engineering controls, safe injection practices, and disinfection and sterilization procedures. The NYSDOH or New York State Education Department must approve the course syllabus and course providers.
Also Check: Hepatitis C Contagious Through Urine
Risk To Healthcare Workers
Contaminated sharps exposure in UK healthcare work is confirmed by Health Protection Agency as the most common mode of occupational exposure to blood-borne viruses, though transmission rates remain low, as a proportion of reported incidents.
The overall risks of the three most common blood-borne viruses being transmitted by an infected patient to a healthcare worker have been estimated, as shown in the table below. Hepatitis B is the most readily transmitted virus and human immunodeficiency virus the least. Healthcare workers are at greater risk of infection from patients than vice-versa. The UK rates of transmission may appear to be higher than in other countries. This is probably as a result of the more active approach to surveillance and the identification of such cases taken in the UK.
Transmission From Infected Health Care Workers To Non
The first cases of transmission of HCV from infected HCWs to non-infected patients were recognized as soon as 1991. After the generalization of hepatitis B vaccination in HCWs, HCV has become the more prevalent blood-borne viral agent at risk to be transmitted occupationally by HCWs. Between 1991 and 2005, 20 HCWs were signified to have transmitted HCV to approximately 400 patients .2). The subject has been reviewed several times during the past 10 years. Schematically, two kinds of situations may be identified from the cases reported in Table Table2.2. The first group of HCV transmission occurred from surgeons performing exposure-prone procedures , with a majority of cardiothoracic specialists and gynecologist-obstetricians. The second group is represented by anesthesiologists or HCWs attending surgery wards who transmitted HCV following a poor respect of hygienic measures and notably of the non-use of gloves during invasive procedures a number of these providers were shown to consume illicit drugs, leading to the use of patients medications for their own use and to the direct contamination of a large number of patients via needle sharing .
Don’t Miss: Best Treatment For Hepatitis C
Studies On Hcv Infection In Healthcare Workers
The prevalence of anti-HCV positivity in healthcare workers ranges from 0% to 9.7% in different studies worldwide: 9.7% in the Philippines, 8% in Egypt, 3.2%-5.6% in three studies in Pakistan, 5% in Georgia, 0.14% in Denmark, 0.8% in Poland, 0.7% in the United States, 0.6% in Albania and 0.3% in Turkey .
Parenteral Routes: Transmission Of Hepatitis B Hepatitis D And Hepatitis C
Hepatitis B, C, and D viruses are all transmitted by what is known as the parenteral route. Parenteral simply means that these viruses can be introduced by all routes except through the intestinal tract, which leaves the door wide open in terms of possible exposure. Let’s look at the possible transmission routes for each of these types of hepatitis virus more closely.
You May Like: Hepatitis C Genotype 2b Treatment
Administration Of Blood Products
As shown in Table Table1,1, the administration of blood products, mainly labile but also stable ones, appears as a major risk factor for acquiring HCV infection in many parts of the world. In developed countries, this assessment is true for past infections contracted before the nineties when no specific test was available for screening the status of donors towards this agent. With the systematic implementation of HCV serology in blood donors in a great number of world areas together with the detection of HCV RNA by nucleic acid testing in several wealthy countries, the risk of acquiring HCV via blood products decreased dramatically. When both measures are associated, this risk becomes negligible, close to 0.1 per million of blood supplies. In resource-limited countries, the situation is more alarming: according to the WHO database on blood safety, 39 countries performed no routine screening of HCV in blood products in 2012 and 47% of donations were tested in settings without quality insurance. These figures show clearly that the eradication of HCV transmission by blood supplies depends mainly on the quality of the screening of both donors and products, which is still out of range for several developing countries due to financial constraints.
Identification Of Patients With Hepatitis C
Hepatitis C is a hidden disease. Most of acute HCV infections are asymptomatic and the chronic phase of hepatitis C is usually asymptomatic too, at least until the occurrence of complications linked to irreversible liver damages. It is important to keep in mind this observation in order to be very large with indications of HCV serology both in patients who can have been exposed to contaminating cares and in HCWs performing EPPs. The occurrence of a symptomatic acute hepatitis C is helpful for recognizing rapidly the contaminating episode and identifying retrospectively other patients exposed to the same risk but having developed an asymptomatic primary infection.
It is not recommended to screen systematically the patients that are submitted to at-risk cares with the aim of grouping all the HCV-infected patients at the end of the care episode this strategy is not cost-effective and could contribute to reduce the vigilance of HCWs when non at-risk patients are cured. In addition, the HCV-negative patients can be at the phase of silent window during HCV primary infection or harbor other infectious agents. The strict respect of Standard Precautions is sufficient for preventing the transmission of blood-borne pathogens .
Read Also: Hepatitis C From Drug Use
Protecting Hcp From Infection
All health care facilities should take the following steps to protect HCP from occupational exposure to bloodborne pathogens :
- All HCP should receive appropriate training for their job titles in infection prevention and control techniques, including engineering and work practice controls, Standard Precautions, and work practices that help prevent sharps or other injuries and splashes of blood and body fluids.
- All HCP should be provided a safe work environment, including protective equipment, clothing, and devices to reduce the risk of occupational exposure to blood and body fluids.
- All HCP whose job responsibilities involve contact with blood or sharp objects likely to be contaminated with blood should be offered and encouraged to receive the hepatitis B vaccine.
- All HCP should receive information about the risks associated with bloodborne pathogen transmission and the merits of knowing their status if they have personal or occupational risks so they may benefit from medical management.
- All HCP should be informed that if they have an impaired immune system, they are at risk of acquiring potentially life-threatening infections, including tuberculosis, from patients.
- Information on the availability of voluntary and confidential or anonymous counseling and testing for bloodborne pathogens should be made available to health care workers.
Enforcement Of Infection Prevention And Control Standards
All licensed health care facilities are responsible under existing regulations for monitoring and enforcing proper use of infection prevention and control practices and Standard Precautions by health care workers functioning under their jurisdiction. Failure to comply with this requirement will result in NYSDOH citation, potential fines, and other disciplinary action against the facility.
Any licensed health care worker who fails to use appropriate infection prevention and control techniques to protect patients or fails to ensure that health care workers under his or her supervision do so may be subject to charges of professional misconduct and disciplinary action 8 N.Y.C.R.R.§ 29.2).
Any patient or employee report regarding lax infection prevention and control practices in a private medical or dental office may prompt an investigation by the appropriate authorities. Substantiated lapses in infection prevention and control in a private practice setting may result in charges of professional misconduct against any licensed professional in the practice who was involved or who has responsibility for ensuring that office staff are adequately trained and follow patient protection measures.
The NYSDOH and NYSED have promulgated regulations and/or statutory amendments to implement these enforcement provisions.
Recommended Reading: Hepatitis A Is A Virus
Hospital Policies That Protect You From Hiv And Other Infectious Diseases
To prevent the spread of HIV, hospitals follow strict infection prevention and control guidelines. All blood and body fluids from patients are treated as potentially infectious:
- Syringes and needles are single use and disposed of in approved sharps containers.
- Reusable medical devices are decontaminated and sterilised after each patient use.
- Many medical devices are disposed of after single use.
- Healthcare workers wear protective equipment including gowns, gloves and eyewear when carrying out any procedures involving a patients blood or body fluids.
- All spilt blood and body fluids are cleaned up according to strict cleaning guidelines.
- Laundry is cleaned according to strict Australian Standards .
Lets Stop Hiv Together
CDCs evidence-based Lets Stop HIV Together campaign is aimed at stopping HIV stigma and promoting HIV testing, prevention, and treatment. The campaign is designed to reach a wide range of audiences, with resources created in both English and Spanish. The resources are designed for both consumers and health care providers. Details of the several campaign components are provided on this page.
HASHTAG:
Also Check: How Can You Catch Hepatitis A
What Is The Link Between Hcv And Hiv
Both HCV and HIV are bloodborne viruses that people can acquire from sharing injection drug equipment. Although sexual transmission of HCV is less common than the sexual transmission of HIV, it can happen if there is direct exposure to blood containing HCV.
A potential complication of HIV is a coinfection. This describes when more than one infection is active at the same time. Evidence indicates that roughly 21% of people living with HIV in the U.S. also have HCV. Other data suggests that approximately 4% of people with HCV have coinfection with HIV. Globally, nearly 2.3 million people are living with an HIV-HCV coinfection.
However, these rates can vary significantly depending on an individuals risk factors. A 2016 systematic review suggests that people living with HIV were six times more likely to have hepatitis C than people without HIV. Additionally, the CDC notes that HIV-HCV coinfection occurs in of people with HIV who use injection drugs.
Chronic liver disease represents a
Reasons For Informing Patients
There is no consensus on whether to inform patients of an infected health care worker of their risk, even when the infection is recognised and the infected health care worker continues to be allowed to practise. The American Medical Association has issued guidance that HIV-infected practitioners undertaking exposure-prone procedures must either disclose this to their patients, obtaining their informed consent prior to treatment or must withdraw from treatment., The New York State Department of Health issued contradictory guidance which did not require disclosure because of the very low risk of transmission of HIV. Similar statements have been made by other American medical authorities.
In the United Kingdom health care workers who are known to be seropositive for HIV or hepatitis B e antigen may not undertake exposure prone procedures, thus protecting patients from known infection risks. Canada’s Laboratory Centre for Disease Control has questioned the value of categorising procedures as exposure-prone in the absence of procedure-specific risk data and does not require health care workers to disclose their infective status.
Despite the similarity of the overall risk to patients from HIV and hepatitis B, UK guidance is less explicit as to whether patients should be informed following risk exposure to hepatitis B in a health care setting.
It may enable patients infected by disease transmitted from the health care worker to be identified.
You May Like: Side Effects Of Antiviral Drugs For Hepatitis B
Surveillance Of Hiv And Aids
HIV and AIDS are both nationally notifiable diseases. National notification is voluntary and data are reported by provincial or territorial public health authorities.
Provinces and territories have legislation for the reporting of priority infectious diseases within their jurisdictions. All provinces and territories collect data on diagnosed HIV infections and report to the Public Health Agency of Canada annually. However, not all provinces and territories have mandatory reporting of AIDS.
Provinces and territories report cases to the Public Health Agency of Canada if they meet the national case definition for HIV or AIDS.
The Public Health Agency of Canada, in partnership with provinces and territories, regional and/or local public health partners, coordinates the Tracks enhanced surveillance system at sentinel sites across Canada. The Tracks system monitors trends in the prevalence of HIV and hepatitis C and associated risk factors in key populations.
Studies On Hbv Infection In Healthcare Workers
The rates of HBsAg and anti-HBc positivity in healthcare workers reported in several studies published in the last three decades range from 0.1% to 8.1% and from 6.2% to 73.4%, respectively, depending on the age of the subjects investigated, the spread of HBV infection in their country of origin and on the prevention strategies used by the healthcare workers .
Also Check: What Is Acute Hepatic Porphyria
What Is Hepatitis C
Hepatitis is inflammation of the liver. Inflammation is swelling that happens when tissues of the body are injured or infected. Inflammation can damage organs.
There are different types of hepatitis. One type, hepatitis C, is caused by the hepatitis C virus . Hepatitis C can range from a mild illness lasting a few weeks to a serious, lifelong illness.
Hepatitis C can be acute or chronic:
- Acute hepatitis C is a short-term infection. The symptoms can last up to 6 months. Sometimes your body is able to fight off the infection and the virus goes away. But for most people, an acute infection leads to chronic infection.
- Chronic hepatitis C is a long-lasting infection. If it is not treated, it can last for a lifetime and cause serious health problems, including liver damage, cirrhosis , liver cancer, and even death.