Flow Diagram Of The Study Participants
Figure shows that of a total of 117,258 HIV-infected individuals who participated in the 2017 vaccination and screening campaign, 21,105 from 62 health facilities met the study criteria and were therefore included in the study, with the details of their selection explained earlier in section.
Fig. 1
Profibrogenic Effect Of Hiv
HIV tropism for hepatic stellate cells and hepatocytes
There is increasing evidence of a direct cytopathic effect of HIV on liver tissue, independent of viral hepatitis co-infection. HIV RNA and p24 antigen were detected in hepatocytes as early as the 1990s. Pathways of HIV pathogenic action are likely to be numerous and are not yet completely elucidated. One of these pathways is related to CCR5 and CXCR4, the two major co-receptors required for HIV entry into host cells. They are expressed on the surface of hepatocytes and hepatic stellate cells , involved in fibrogenesis. Recent data suggest that HIV and/or the HIV glycoprotein gp120 ligation of CXCR4 receptors present on hepatocytes selectively up-regulate tumour necrosis factor -related apoptosis-inducing ligand R2 expression and confer an acquired sensitivity to TRAIL-mediated apoptosis. According to the authors, HIV infection renders hepatocytes more susceptible to liver injury during disease states associated with enhanced TRAIL production, such as HBV infection. Recent experimental data suggested the ability of HIV to infect HSC and to promote their myofibroblastic differentiation leading to the production of -smooth muscle actin, collagen and monocyte chemoattractant protein 1.
Altered innate and adaptive immune response
Hbv Immune Restoration And Hbv Reactivation
Hepatic flares in the setting of HIV/HBV co-infection are caused by multifarious factors and are frequent, with an incidence rate of cytolysis over twice the normal value at 13.4 per 100 patient years , as observed in a cohort of 308 patients over a 3 year period. Immune restoration disease is a troubling complication of restoring the adaptive anti-HBV immune response while under antiretroviral treatment. Recent data suggest that IRD is mediated by proinflammatory and antiviral cytokines, such as TNF- and interferon- , which in turn can induce the production of several chemokines. These chemokines include CXCL-10, a protein whose concentration has been proved to be positively correlated with biochemical scores of liver fibrosis and liver enzymes levels in HIV/HCV co-infected patients.
HBV reactivation is another feared complication of either unplanned interruption of HIV drugs with HBV activity or emergence of HBV resistance, which might lead to major hepatic flares and increases the risk of fulminant hepatitis and the need for urgent orthotopic liver transplantation .,
You May Like: How Does Someone Get Hepatitis C
Hiv And Life Expectancy
If youâve been diagnosed with human immunodeficiency virus , youâre bound to wonder how it will affect your future, and how long the future might be.
Youâre in for good news. Research shows that people who start HIV treatment early can live as long as people who donât have the virus. Thatâs a big improvement over the figures from 2010, when studies said that HIV could cut your life short by 13 years.
But thereâs more to this story. If you have HIV, youâre more likely to have certain health challenges, and some of them can be serious. Some may be because of the virus and your treatment for it. Others will be due to things everyone faces, such as aging.
Also, some groups are less likely to benefit from improvements in life expectancy with the virus. Those most likely to face extra challenges:
- Are not white. Nonwhite people with HIV sometimes may not receive the same quality of care.
- Have a history of injecting drugs.
- Started HIV treatment later after getting HIV.
Impact Of Hbv And Hiv Cure Strategies
As in HIV, there has been recent increased interest in strategies that may lead to a cure for HBV. In contrast to HIV infection, there is a clear biomarker for HBV remission which is the development of antibodies to HBsAg ]. The main barriers to cure include the persistence of cccDNA and HBsAg . The use of currently available NRTIs can successfully suppress replication of HBV DNA and reduce but not eliminate HBsAg production but have little impact on cccDNA. Hence, in most individuals in the absence of HBsAg seroconversion, HBV DNA rebounds following cessation of NRTI . Furthermore, although suppression of plasma HBV DNA leads to decreased levels of fibrosis, cirrhosis and HCC, levels of HBsAg still remain elevated which may be related to the persistence of cccDNA.
Read Also: Can Hepatitis Cause Low Platelets
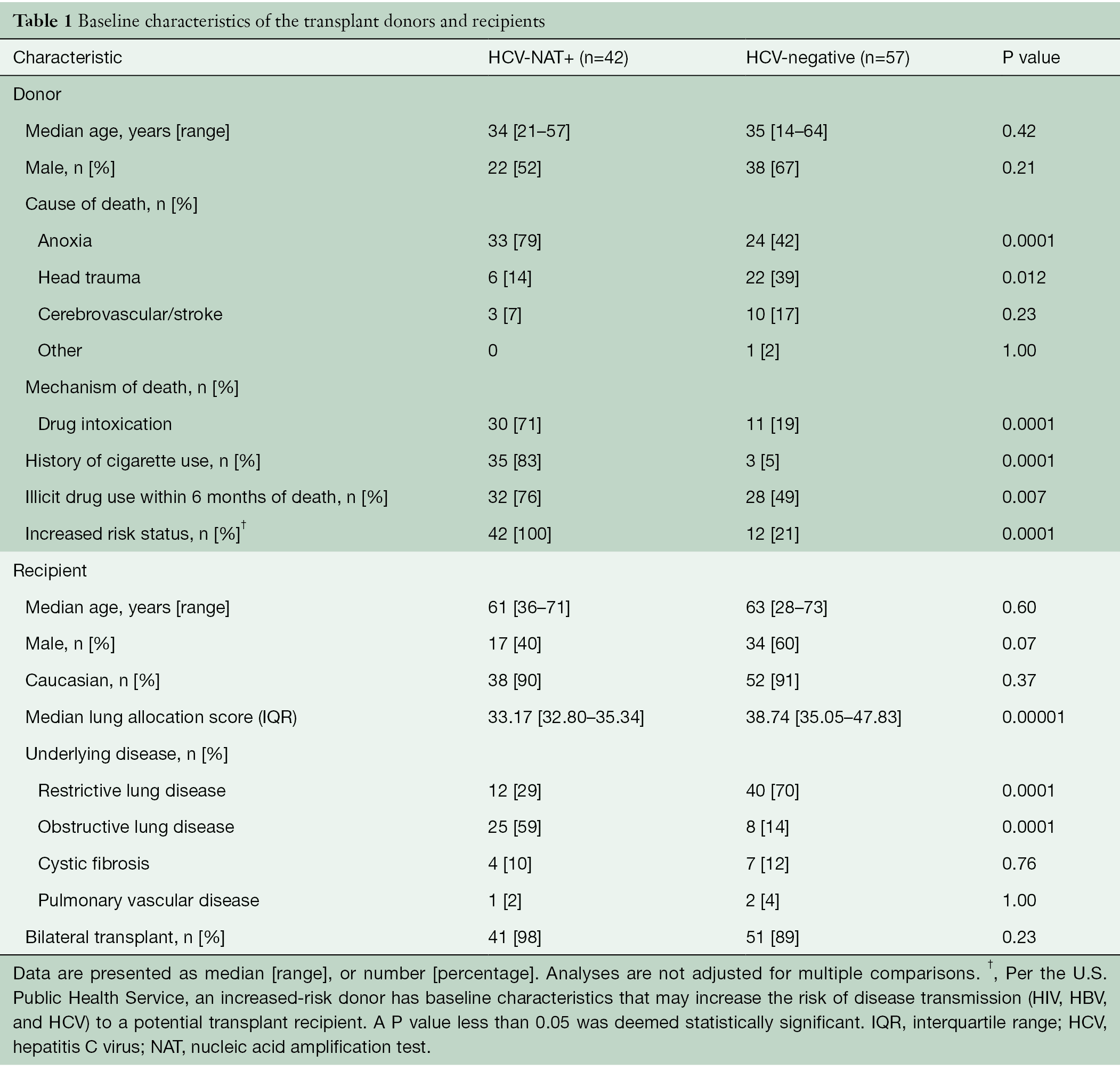
Data Processing And Data Collection
Data were collected using a predefined list of variables. This was developed and approved by the study committee after consultation of the literature on factors affecting survival of HIV-infected individuals. The unique patient identifier in the HBV vaccination and screening database and in the national EMR database for HIV-infected patients were matched, as the EMR did not contain HBV results. The HBV vaccination and screening database showed that as of 31 January 2016, HBV results were available for 59 health facilities and only 40 sites had EMR backups. To include all provinces, urban and rural district hospitals and health centers, we extended the period to 29 February 2016, and 62 of the 71 facilities including six district hospitals and 56 health centers were included and were visited to manually complete missing data, which resulted in 21,105 records for analysis. We considered these data sufficient to cover residence and geographic characteristics. Health care personnel involved in recording patient data received constant supervision and mentoring to ensure high quality data. In addition, data found to be incomplete or inconsistent were cross-checked on-site with patient files and patient registers. The principles of data protection and good scientific practice were strictly followed, both in Rwanda and in Germany, where the analysis was conducted and ethics committees in both countries approved the study .
Whats The Outlook For People Who Have Hiv And Hepatitis
HIV-hepatitis coinfections are treatable, but there are differences in the overall outlook depending on the severity and type.
For example, HCV may be cured within months, while HBV often requires lifelong treatment. If youre living with HIV, youll also need lifelong treatment for HIV, too. Complications may include cirrhosis or liver cancer.
Theres no medication available for HAV infections. If youre living with HIV and receive an HAV diagnosis, your doctor will monitor your condition carefully for complications, such as liver failure.
With treatment, HIV can become undetectable. When the virus is undetectable, it cant be transmitted to other people.
If youre living with HIV without a current hepatitis infection, your doctor may recommend regular testing to help detect hepatitis early on, depending on your risk factors. The earlier hepatitis is diagnosed and treated, the better the outcome.
Read Also: Hepatitis C Outside The Body
Hepatocellular Carcinoma In Hepatitis B And Human Immunodeficiency Virus Coinfection In Africa: A Focus On Surveillance
Qian Wan1Chimaobi Anugwom1,2Hailemichael Desalegn3Jose D. Debes1,4
1Department of Medicine, Division of Infectious Disease and International Medicine & Division of Gastroenterology, Hepatology and Nutrition, University of Minnesota, Minneapolis, MN 55455, USA.
2Health Partners Digestive Care, Saint Paul, MN 55130, USA.
3Millennium Hospital, Addis Ababa 1000, Ethiopia.
4Arusha Lutheran Medical Centre, Arusha, Tanzania.
Correspondence to: Dr. Jose D. Debes, Department of Medicine, Division of Infectious Disease and International Medicine & Division of Gastroenterology, Hepatology and Nutrition, University of Minnesota, 420 SE Delaware St., Minneapolis, MN 55455, USA. E-mail: debes003@umn.edu
Received: First Decision: Revised: Accepted: Academic Editors: Copy Editor: Production Editor:
© The Author 2022. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Access To Liver Transplantation And Innovative Procedures For Hcc Treatment
As highlighted by a recent retrospective cohort study conducted in France on 898 HIV-infected patients, of whom 15.4% died from a liver-related cause, HCC is rising as an aetiology of ESLD and is likely a harbinger of an emerging problem for persons living with hepatic co-infection in regions with access to potent ARV regimen.
Innovative procedures for HCC treatment and OLT should no longer be excluded from HIV-infected patients. As HIV disease is being more easily controlled than ever, patients with decompensated cirrhosis should be referred earlier for OLT because of the increased risk of death whilst waiting for a transplant . The outcome of OLT in HIV/HBV co-infected patients is very reassuring, with 100% survival at a median 3 year follow-up. For patients with HCC, systemic treatment, such as sorafenib, transarterial chemoembolization or radiofrequency thermal ablation, should be discussed similar to non HIV-infected patients, according to official recommendations., Sorafenib is the first oral multikinase inhibitor of the vascular endothelial growth factor receptor and the platelet-derived growth factor receptor. Its use has led to a significantly increased survival rate in patients with HCC and is currently being evaluated in the context of HIV because of its potential interactions with protease inhibitors.
Also Check: Ways You Can Get Hepatitis
Frequency Of Periodic Screening
There is an overall agreement among recommendations to screen HIV-monoinfected patients annually for the presence of serum HBsAg and to screen for this antigen in cases of hypertransaminasaemia. In HBsAg-negative patients without evidence of anti-HBc-positive serology, immunization schedules must be adapted to anti-HBsAb response. Isolated HBcAb seropositivity is common in HIV-infected patients and could be a marker of occult HBV infection, whose prevalence varies across subgroups of patients. HBV DNA and liver function tests should therefore be systematically assessed in patients with such a serologic pattern. If acute HBV infection is suspected, anti-HBc immunoglobulin M should also be tested.
Learning Objective Performance Indicators
- Explain the impact of HIV on coinfection with HCV
- Discuss sustained virologic response outcomes demonstrated in key studies using direct-acting antiviral agents to treat HCV in persons with HIV coinfection
- Differentiate HCV treatment duration for HCV monoinfection versus HCV-HIV coinfection
- Summarize recommendations for monitoring persons with HCV-HIV coinfection after initiating antiretroviral therapy
- Highlight drug interactions from the perspective of direct-acting antivirals and antiretroviral medication classes
DisclosuresReviewer:
You May Like: Patient Has Immunity To Hepatitis B Virus
Genotypes Viral Mutants And Long
Genotypes and mutations on one of the P, S and C genes constitutive of the HBV genome have recently been associated with differences in HBV disease evolution and treatment response. The peculiarity specific to HIV/HBV co-infection resides in the fact that most mutations are induced by long exposure to nucleosides that have been largely used to treat HIV.
Genotype distribution is linked to the geographical origin of patients and is not influenced by HIV or treatment . Cohort studies have found an association between some genotypes and the risk of severe liver fibrosis or HCC . Whether or not these results should elicit routine genotyping of HBV strains in daily practice still remains to be evaluated.
Pathogenesis Of Liver Diseases
HBx can also stimulate the expression of cyclooxygenase-2 , which is overexpressed in liver cirrhosis . Moreover, COX-2 expression can be activated by IL-8 through CREB and C/EBP . Accumulating evidence shows that HBV proteins activate IL-8 and COX-2 to maintain the inflammatory environment . The inflammatory hepatocytes secrete C-X-C motif chemokine 10 which linked to the severity of liver damage involving viral hepatitis . Once CXCL10 binds to its receptor, chemokine receptor 3 , immunocytes such as natural killer cells, and activated T cells and B cells are attracted to the inflammatory sites . Elevated CXCL10 was found in HBV/HIV coinfected patients but not in HBV mono-infected patients. This observation indicates that CXCL10/CXCR3 in the liver contributes to the acceleration of liver diseases .
Don’t Miss: What Hepatitis Is Not Curable
People Coinfected With Hiv And Viral Hepatitis
People with HIV/AIDS should be vaccinated against hepatitis A and B and tested for hepatitis B and hepatitis C.
Beginning in 2020, CDC and the Advisory Committee on Immunization Practices began recommending that all people with HIV who are 1 year of age be vaccinated against hepatitis A and receive postvaccination serologic testing 1 month after completing the hepatitis A vaccine series.
Further, CDC and ACIP recommend that unvaccinated people with HIV receive hepatitis B vaccination. Vaccination should be followed by serologic testing to confirm adequate immune response. CDC recommends that people with HIV be tested for hepatitis B.
CDC now also recommends one-time hepatitis C testing of all adults , including those with HIV. CDC continues to recommend people with risk factors, like people who inject drugs, be tested regularly.
People with HIV and Hepatitis A
People with HIV and Hepatitis B
People with HIV and Hepatitis C
F Immune Reconstitution Disease
IRD or Immune reconstitution Inflammatory Syndrome is defined as worsening symptoms related to an opportunistic infection or malignancy in an HIV-infected individuals following initiation of ART . In HIV-HBV co-infection, IRD is defined as a hepatic flare or a significant increase in hepatic transaminases following initiation of ART. We previously showed that in a cohort of HIV-HBV co-infected individuals initiating ART with advanced disease in Bangkok Thailand, 22% had a hepatic flare consistent with IRD. Our study confirmed the findings of others that a high pathogen load , high baseline alanine transaminase and a low CD4+ T-cell count were the biggest risk factors for developing HBV-related IRD . The immunological drivers of IRD are still unknown although may potentially be secondary to persistent elevation of the interferon stimulated gene CXCL10 leading to enhance T-cell recruitment to the liver following ART initiation .
The occurrence of hepatic flares has been linked to seroconversion in Hepatitis B monoinfection. In HIV-HBV coinfection, IRD may be reflecting a similar process and this may be the basis for the increased levels of HBsAg loss and seroconversion seen in HIV-HBV co-infecion. In three HIV-HBV infected individuals with hepatic flare following commencement of TDF-containing ART, a significant decline in qsAg levels was observed .
Also Check: How Do You Cure Hepatitis C
A Hiv Replication In The Liver
A number of studies have shown various cell types in the liver are permissive to HIV infection in vitro including HSC, Kupffer cells and hepatocytes . HIV infection of these cells has also been demonstrated in vivo in individuals naïve to ART and HIV sequences from the liver in individuals off ART have distinct compartmentalised sequences when compared to other tissue sites . There have been few studies to determine whether HIV persists in the liver on ART but studies of animal models, including SIV-infected macaques and HIV-infected humanized mouse models both suggest that HIV can persist in the liver on ART, primarily in Kupffer cells . Recently, infectious replication competent HIV was isolated from Kupffer cells obtained from liver at autopsy from three HIV-infected individuals who died on ART .
In the absence of virus replication on ART, HIV may also contribute to liver inflammation and fibrosis by binding of gp120 to CXCR4 which is expressed on hepatocytes and HSC . The effect of HIV infection and or HIV proteins in the liver has primarily been studied in the context of HIV-HCV co-infection in vitro but not in HIV-HBV co-infection. HIV infection alone, or in the presence of HCV, induced profibrotic processes in hepatocyte and HSC cell lines including increased chemokine production, HSC migration, hepatocyte apoptosis and expression of profibrotic genes .
Older Could Mean Healthier For People With Hiv
Statistician Caroline Sabin reviewed recent life expectancy data, including previous UK CHIC data. She emphasized that factors like late diagnosis, injecting drug use, and coinfection with hepatitis B or C all tended to depress life expectancy in people with HIV. This meant that crude comparisons between life expectancy in the HIV positive population and the HIV negative population consistently reported lower life expectancies for people with HIV: in the case of the U.K., by 12 to 13 years, and even lower in countries like the U.S. with more unequal access to healthcare.
However, injecting drug use could reduce life expectancy by 10 years and hepatitis C contributed 31.5% of the mortality seen in people with HIV. Although over a lifetime the impact of late diagnosis was limited, mortality in the first year after diagnosis was hugely greater than it is in any subsequent year. For instance, the likelihood that someone diagnosed with a CD4 count of 140 cells/mm3 at age 30 would be dead by the age of 50 was about 25%, but for someone diagnosed with a CD4 count of 430 cells/mm3 it was about 10%.
Don’t Miss: Hepatitis B Vaccine For Infants Schedule
How Are Hepatitis B And Hepatitis C Spread From Person To Person
Like HIV, the hepatitis B and hepatitis C viruses spread:
- Perinatally: Pregnant people can pass these infections to their infants. HIV-HCV coinfection increases the risk of passing on hepatitis C to the baby.
- Sexually: Both viruses can also be transmitted sexually, but HBV is much more likely than HCV to be transmitted sexually. Sexual transmission of HCV is most likely to happen among gay and bisexual men who have HIV.
A New Antivirals For Hbv
i) Tenofovir alafenamide
Tenofovir alafenamide is a prodrug of tenofovir that has activity against HIV-1, HIV-2 and HBV with higher intracellular concentrations in PBMCs and hepatocytes relative to plasma compared with TDF, thereby allowing for lower dosing and reduced toxicity . TAF has reduced adverse effects on renal function and bone mineral density seen while maintaining high rates of viral suppression in both HIV and HBV .
In HIV-HBV co-infection, switching from a TDF to a TAF-containing regimen demonstrated similar high levels of HBV virological control .
ii) HBV entry inhibitors and others
Don’t Miss: Where Can I Get A Hepatitis B Shot
Medications For Hepatitis B
Several drugs are currently available for treatment of hepatitis B. Most of these are antiviral drugs that directly stop hepatitis B from reproducing. Hepatitis B treatment may also include pegylated interferon, which stimulates the body’s immune response against the virus.
Most hepatitis B drugs are nucleoside or nucleotide analogues, similar to one class of drugs used to treat HIV. In fact, some commonly used anti-HIV drugs are also active against hepatitis B. This can make treatment of both viruses easier, since it requires fewer drugs, but it must be done carefully to avoid either virus becoming resistant. These are:
- emtricitabine .
- tenofovir disoproxil or TDF .
- tenofovir alafenamide or TAF .
Other antiviral drugs are used to treat hepatitis B but not HIV: