What Is The Role Of A Liver Biopsy In Chronic Hepatitis B
During a liver biopsy, a small sample of liver tissue is collected and examined under the microscope. This test is valuable because this sample reflects the health of the liver. It can show the amount of liver injury . Liver biopsy is not routinely needed to diagnose hepatitis B, but it is used for monitoring the progression of liver damage in people with chronic hepatitis and helping to choose or evaluate treatment options.
Hepatitis B Vaccine Challenge Dose And Laboratory Testing
After written informed consent was obtained, information on demographics, height, weight, risk factors for HBV exposure , and vaccination history were collected from each participant. Blood was drawn for serologic testing immediately before and 2 weeks after a challenge dose of hepatitis B vaccine was administered by injection into the deltoid muscle with a standard-size needle. Serum specimens were frozen and shipped to the CDC Hepatitis Reference Laboratory for testing. Baseline specimens were tested for antibody to anti-HBsAg and total antibody to hepatitis B core antigen with the VITROS ECi Immunodiagnostic System . Specimens positive for anti-HBcAg were tested for HBsAg and HBV DNA. Postchallenge specimens were tested for anti-HBsAg only. A response to the challenge dose was defined as a postchallenge anti-HBsAg level of 10 IU/liter among persons with a baseline anti-HBsAg level of < 10 IU/liter. The results of serologic testing were not available for the investigators or participants until after completion of the study.
Chronic Hbv Carriers At Greatest Risk Of Hepatic Sequelae
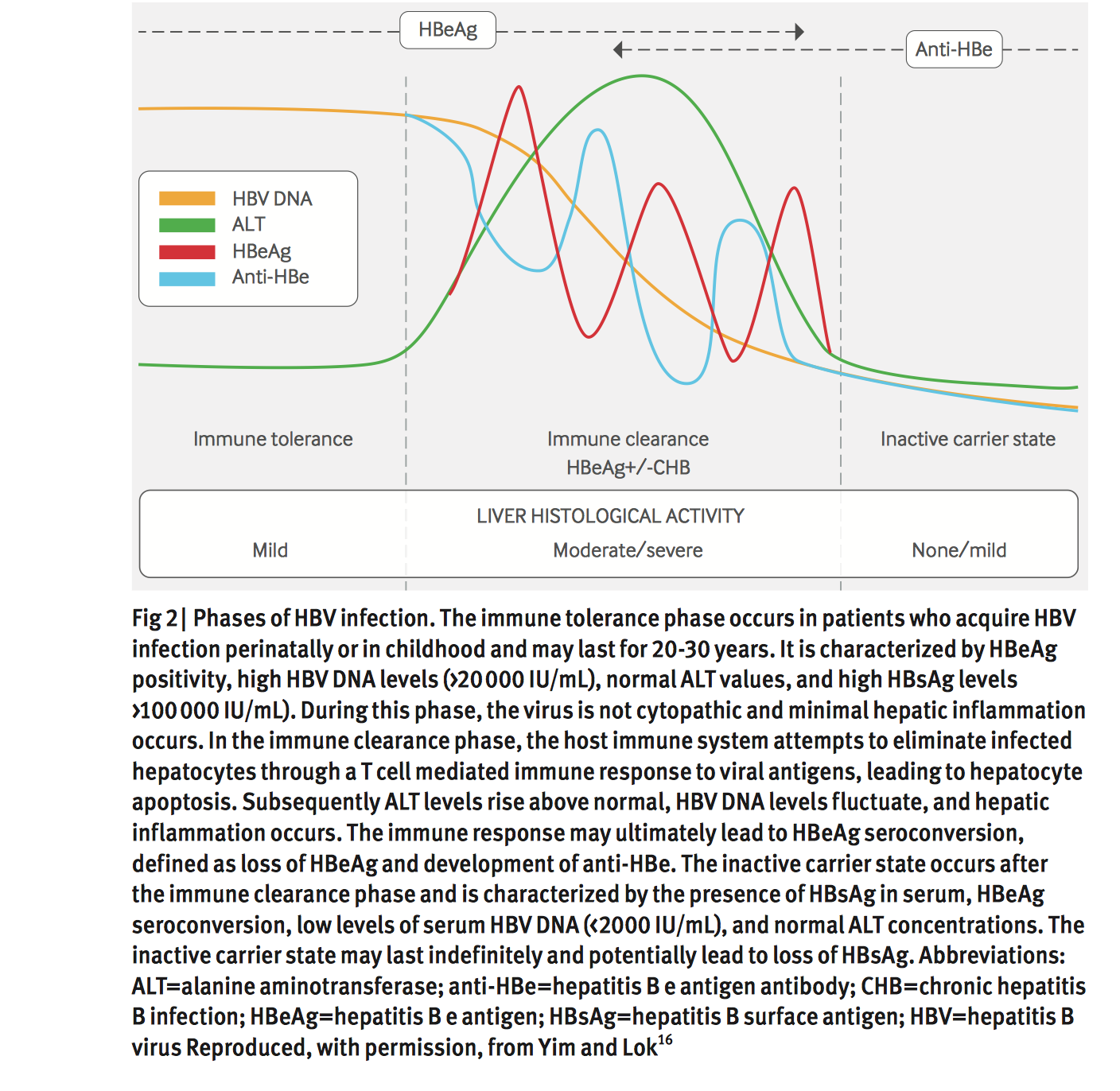
Sustained elevations in ALT, although an imperfect marker for hepatic damage, can help identify chronic HBV carriers at greatest risk of sequelae and those most likely to benefit from current treatments . Chronically infected patients with sustained ALT elevations greater than the upper limit of normal may be candidates for treatment and should undergo additional prognostic hepatitis marker testing as outlined below. Chronic carriers whose ALT is within the normal range should be tested for this marker periodically because ALT levels can fluctuate with this illness. Determination of ALT levels and HBV serological and nucleic acid markers, although valuable in following infection, is not adequate to assess the severity of infection and the resulting liver damage. Before appropriate treatment can be initiated, consultation with a specialist and assessment of the disease through histological examination of a liver biopsy is strongly recommended.
Also Check: Can You Catch Hepatitis C From Sex
Challenges Ahead And Conclusion
Targeting and elimination the HBV cccDNA which acts as a template for the transcription and persistence of HBV RNAs and seroconversion of HBsAg is considered a complete cure of HBV infection. It is well documented that cDNA acts as a reservoir of HBV and persists in the nucleus. The current treatment for CHBV patients is antivirals and traditional immune modulators. However, they have their own limitations such as drug resistance, flu-like symptoms, and other side effects. For the functional cure of HBV clearance, there is a need to introduce rationale-based newer immune modulators and cytokine adjuvants which induce protective host immune responses for seroconversion and target cccDNA and cellular host proteins for viral entry and replication. Research from the past 2 decades has provided clues of the role of humoral immune response in HBV infection.
Recommended Tests To Investigate Acute Hbv Infection And The Interpretation Of Results
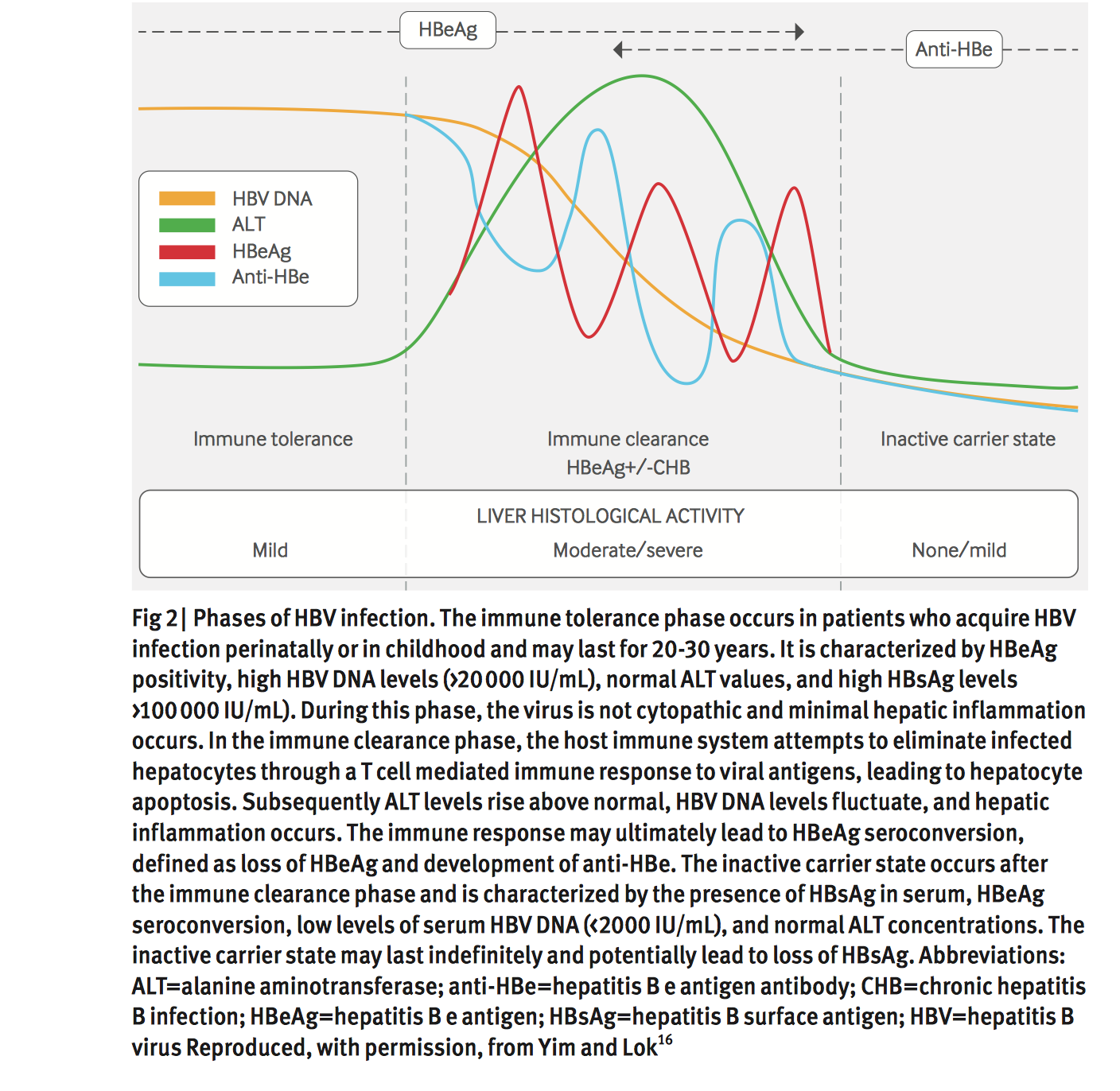
Acute HBV infection generally presents after an incubation period of six weeks to several months with an onset of nonspecific symptoms that may include fever, malaise, anorexia and nausea, followed by the onset of jaundice, dark urine and pale stools. Approximately 25% to 40% of infected adults will be symptomatic, and most will demonstrate elevations in ALT however, infants, toddlers and immunosuppressed individuals may not manifest signs or symptoms of infection. The management of acute infections is largely supportive unless fulminant hepatitis develops, in which case the patient should be referred to a liver specialist. Because the clinical features of acute hepatitis are very similar for HAV, HBV and HCV, testing for all three agents should be performed when working up an acute case. While the sexual transmission of HCV is rare, varying between zero to six cases per 1000 person-years , HAV that is typically spread by the fecal-oral route poses a clear risk to sexual partners. Figure and Table outline the appropriate serological tests to investigate acute hepatitis.
Don’t Miss: How Contagious Is Hepatitis B
Negative But Other Hepatitis Tests Are Positive
Your HBsAb test may be negative even when other hepatitis B tests are positive, showing active or chronic infection. Further testing is necessary, especially for the hepatitis B surface antigen , which shows that the virus itself is circulating in your bloodstream and that you have an active or chronic infection.
How Do Medical Professionals Diagnose Hepatitis B
Infection with hepatitis B is suspected when the medical history and the physical examination reveal risk factors for the infection or symptoms and signs that are suggestive of hepatitis B. Abnormalities in the liver tests also can raise suspicion however, abnormal liver tests can result from many conditions that affect the liver. The diagnosis of hepatitis B can be made only with specific hepatitis B virus blood tests. These tests are known as hepatitis “markers” or “serologies.”
HBsAg and anti-HBs
The presence of hepatitis B surface antigen in the blood indicates that the patient is currently infected with the virus. HBsAg appears an average of four weeks after initial exposure to the virus. Individuals who recover from acute hepatitis B infections clear the blood of HBsAg within approximately four months after the onset of symptoms. These individuals develop antibodies to HBsAg . Anti-HBs provides complete immunity to subsequent hepatitis B viral infection. Similarly, individuals who are successfully vaccinated against hepatitis B produce anti-HBs in the blood.
Patients who fail to clear the virus during an acute episode develop chronic hepatitis B. The diagnosis of chronic hepatitis B is made when the HBsAg is present in the blood for at least six months. In chronic hepatitis B, HBsAg can be detected for many years, and anti-HBs does not appear.
Anti-HBc
HBeAg, anti-HBe, and pre-core mutations
Hepatitis B virus DNA
How are the hepatitis B blood tests interpreted?
Also Check: Hepatitis C Treatment Side Effects
What Is New In The Treatment Of Hepatitis B
New agents are under development to treat hepatitis B. Many of these are nucleoside/nucleotide analogues that investigators hope will be more effective than older agents. Experts also are working on treatment guidelines and the use of multi-drug therapy. Vaccination remains the key to preventing hepatitis B and holds the most promise for reducing disease burden.
How Do People Get The Hbv Virus
Hepatitis B virus is found in the blood of people with HBV infection. It enters the body through blood-to-blood contact.
Reliable blood tests for HBV were developed many years ago. Since blood donors and blood products are tested for HBV, this is no longer the typical means of infection.
In many parts of the world, hepatitis B virus infects more than 8% of the population. HBV-infected women pass the infection to their babies during the birth process. People can also get hepatitis B by sharing needles for injection drug use, through sexual contact with an infected person, by an accidental needlestick with a contaminated needle, or from improperly sterilized medical, acupuncture, piercing, or tattooing equipment.
Read Also: Is There A Cure For Hepatitis C Virus
What Do I Do If Im A Hepatitis B Vaccine Non
Approximately 5-10% of people do not develop protective antibodies following the completion of the hepatitis B vaccine series. This is confirmed with a blood test called an anti-HBs titer test which is given 4 weeks following the completion of the series. If the test shows the titer is less then 10 mIU/mL the general recommendation is to complete the series again using a different brand of vaccine . A person is considered to be a non-responder if they have completed 2 full vaccination series without producing adequate protective antibodies.
Another vaccine option is the new two-dose hepatitis B vaccine, HEPLISAV-BTM. The new vaccine is expected to increase immunization rates for adults in the United States and is administered over a one-month period. The vaccine provides greater seroprotection, which can mean a greater antibody response especially in adults who may be older, obese or live with type 2 diabetes making it an effective vaccine option.
It is also possible that a person who does not respond to the vaccine may already be infected with hepatitis B. Therefore, testing for the presence of the hepatitis B virus is recommended before diagnosing a person as a vaccine non-responder.
CDC Recommendations for Hepatitis B Vaccine Non-Responders
Check out our previous post on the topic here.
References:
HEPLISAV-B. Retrieved from:
Therapeutic Strategies For Chb
Based on the knowledge about the immune pathogenesis of chronic HBV infection, a number of innovative strategies may be applied to enhance HBV-specific immune responses in patients . On one hand, oral, intranasal, or subcutaneous application of agonists of pathogen recognition receptors , including TLRs, retinoic acid-inducible gene 1 , and stimulator of interferon genes , activates host immune cells and hepatocytes/non-parenchymal liver cells, leading to the production of IFN/expression of interferon-stimulated genes and proinflammatory cytokines, which jointly mount an antiviral state . On the other hand, HBV-specific CTLs can be induced by therapeutic vaccines, boosted through checkpoint blockade, or renewed by adoptive transfer of in vitro activated T/NKT cells or genetically edited HBV-specific T cells such as chimeric antigen receptor T or T cell receptor -T cells . These strategies have been explored in the past years. Though their potential usefulness is partly proven, many obstacles hindering the clinical use of these approaches are still to be overcome in the future.
Don’t Miss: Hepatitis A And B Vaccine
What Treatments Are Available For Chronic Hepatitis B If Medications Dont Work
If you have advanced hepatitis B, you might also become a candidate for a liver transplant. This path does not always result in a cure because the virus continues in your bloodstream after a transplant. To prevent being infected again after your transplant, you may be prescribed hepatitis B immunoglobulin with an antiviral agent.
Evaluation Of Individuals Suspected Of Having An Hbv Infection
Given the perinatal and childhood vaccination programs already in place in North America, most HBV-infected individuals will likely present with chronic infection. Such individuals are likely to have risk factors that include immigration from high endemicity regions, injection drug use or sexual contact with an infected person 1) . Therefore, the present guideline will provide diagnostic recommendations first for individuals suspected of having chronic HBV infection and, subsequently, for those with acute infection. The diagnosis of HBV infection in any individual has important management implications, including appropriate counselling, monitoring and/or treating and vaccinating family or at-risk contacts.
Also Check: Hepatitis A Vaccine Cost Walmart
Diagnosis Of Acute And Chronic Hepatitis B
HBsAg is the first serologic marker to appear and may be detected within 1 to 2 weeks after exposure. It precedes the development of symptoms by an average of 4 weeks.106 The presence of HBsAg indicates ongoing infection. Qualitative but not quantitative methods are used by most clinical laboratories because the amount of antigen does not correlate with disease activity or with the presence of an acute or chronic infection.28 Some symptomatic patients may have self-limited, acute HBV infection without detectable HBsAg. These patients, up to 9% in some studies, have other detectable markers of infection.106 HBeAg appears virtually simultaneously, peaks, and then declines in parallel with HBsAg. It usually disappears before HBsAg does. Adult patients who remain persistently positive for HBeAg for more than 10 weeks are likely to become chronically infected. HBeAg indicates a high level of viral replication and infectivity. Most patients with nondetectable HBeAg have resolving, minimal, or no active liver disease.28 Precore mutants of HBV do not express HBeAg they may be responsible for a more severe course and, in some cases, fulminant disease. Serum aminotransferase levels become elevated but are nonspecific. They begin to increase just before the development of symptoms and then peak with the development of jaundice.
Howard C. Thomas, Jennifer A. Waters, in, 1998
Acquired Immunity Against Hbv
In acute hepatitis B, HBV-specific CD8+ T cells enter the liver and produce IFN- . Chimpanzee studies have shown that CD8+ T cells are critical to eliminating HBV when depleted during HBV amplification, infected animals lost the capacity to eradicate HBV. In contrast, CD4+ T cell depletion in acute hepatitis B has little effect on HBV eradication. However, CD4+ T cell depletion before HBV infection impairs HBV eradication by decreasing CD8+ T cell migration into the liver . These results indicate that the early priming of CD4+ T cell by HBV is of considerable importance to eradicating HBV.
Read Also: What Is The New Drug For Hepatitis C
Hbv Adaptive Immune Responses And Therapy
In adaptive immunity, CD8+ T cells are considered as one of the most important players in HBV infection, which act through cytolytic or noncytolytic mechanisms via the secretion of IFN- and TNF- . However, defective virus-specific responses by CD8 cells have been observed in CHBV patients . Even in the presence of profound DC activation and antigen presentation, HBV-specific CD8+ T-cell exhaustion under continuous exposure to HBV antigens is a major challenge to clear the virus. Regulatory T cells, which are known for downregulation of inflammatory immune responses and maintaining the immune homeostasis, have been shown to fail during chronic HBV infection . Regulatory T cells maintain immunosuppressive functions by secreting the inhibitory cytokines such as TGF-, IL-10, and IL-35 and suppress the activation of antigen-specific or nonspecific proliferation in most of the function of the immune cells . The current strategy for the restoration of the function of T cells, blocking or neutralizing the inhibitory receptors and cytokines may be effective therapeutic targets in HBV.
Currently available treatments of CHB include standard IFN-, Peg-IFN-2a, Peg-IFN-2b, and NA . A comparison of these antiviral therapies fails to show the superiority of one therapy over another with the aim of risk reduction in liver-related complications . The current, underexploration therapies and immune modulators have been discussed in Table 1.
Table 1.
Laboratory Findings And Diagnostic Tests
Serum HBsAg and anti-HBs are the most useful screening tests for chronic HBV infection or immunity to HBV. HBsAg is present in most chronically infected persons. Lack of anti-HBs in an unvaccinated HBsAg-negative person indicates susceptibility to HBV infection.3
Routine screening for HBV infection is recommended for the following people: all pregnant women all infants born to HBsAg-positive women after completing the vaccination series immigrants from regions of high or intermediate HBV endemicity US-born people, who were not vaccinated as infants, whose parents were born in regions with HBsAg prevalence â¥8% people with elevated serum ALT or aspartate transaminase levels of unknown etiology people with behavioral risks, including MSM and injection-drug users hemodialysis patients, HIV-positive persons persons needing immunosuppressive therapy donors of blood, plasma, organs, tissues, or semen household, needle-sharing, or sexual contacts of persons known to be HBsAg positive and persons who are the source of blood or body fluids for exposures that might require postexposure prophylaxis.65
Screening for HBsAg is recommended at the first prenatal visit for all pregnant women.3,109 Women in labor without HBsAg test information should have HBsAg serology on arrival. In addition, pretested women who have a history of certain risk factors should be retested at the time of admission to the hospital for delivery.3,110
Fabrizio Fabrizi MD, … Paul Martin MD, in, 2017
Read Also: What Is Hepatitis C Antibody Mean
Specimen Choice Collection And Transport
The specimen of choice for the diagnosis of HBV infection is blood. Serological tests for viral antigens and antibodies are typically used for diagnostic screening and can be performed on either serum or plasma. Both HBV antigens and antibody are stable at room temperature for days, at 4°C for months, and frozen at -20°C to -70°C for many years. Because modern testing involves automated enzyme immunoassays that depend on colourimetic or chemiluminescence signal measurement, care should be taken to avoid hemolysis of the sample because it may interfere with the ability of the assay to accurately detect these markers.
A number of nucleic acid-based tests, which have been the subject of recent reviews , are available to directly detect HBV-DNA in serum or plasma. Care must be taken to avoid the degradation of the viral nucleic acid in the specimen, which can result in falsely low or no measurable viral load. Serum should therefore be removed from clotted blood within 4 h of collection and stored at -20°C to -70°C , and can be subjected to up to eight short-term freeze-thaw cycles without significant loss of detectable HBV-DNA . Alternatively, the presence of EDTA in plasma is known to stabilize viral nucleic acids. EDTA blood can be stored for up to five days at 4°C without affecting the viral load . Polymerase chain reaction-based tests can use either serum or plasma, while hybridization-based assays recommend the use of serum.
Mechanisms Of Hbeag And Hbsag Seroconversion
B cells do not have critical roles in the elimination of viral particles directly . However, B- and TFh-cell responses have been shown to play an important role in preventing viral expansion within the host and also the main players in HBe or HBsAg seroconversion.
TFh cells reside in the secondary lymphoid organ and help in the B-cell differentiation through the secretion of IL-21 . TFh cells express distinctive markers, including the transcriptional repressor Bcl6, the chemokine, and the costimulatory molecules such as CXCR5, ICOS, and CD40L . Translocation of TFh cells toward the CXCL13-rich germinal center is mediated by the CXCR5 expression . TFh cells have been emerged as a crucial player in B-cell differentiation to form antibody-producing plasma cells that offer lifelong protection . It is observed that the absence of TFh cells at the onset of infection reduces the overall humoral response and prevents viral clearance .
Fig. 2.
Phenotypic marker and characterization of TFh cells: TFh cells can be distinguished on the basis of transcription factors , costimulatory marker , and by secretion of the key cytokine IL-21. TFh, T follicular helper.
High-affinity class-switched antibodies are essential in clearing and establishing long-lasting humoral immunity against HBV infection and effective vaccination. It is observed that in response to HBV vaccination, antibody secretion was influenced by genetic polymorphism of CXCR5 and CXCL13 .
Also Check: What Is The Prognosis For Hepatitis C