How Should Potential Liver Disease Be Investigated
As outlined, assessment of standard liver function tests at baseline or steady state can be difficult, unless very normal or very abnormal. Minor abnormalities may reflect hemolysis more than intrinsic liver injury. More significant derangements are encountered in the acute liver syndromes, as described in the following paragraphs. In the setting of chronic liver disease, a progressive increase in the conjugated fraction of total bilirubin and reduction in serum albumin are ominous signs. All patients should have a screen to identify liver disease that has resulted from transfusion of blood or is coexistent this includes hepatitis viral serology, a liver autoantibody screen , ferritin, and copper studies. Ferritin is limited as a marker of iron burden in SCD because it can be affected by both liver disease and inflammation. Instead, magnetic resonance imaging is recommended to detect liver iron load such as R2-MRI or T2* measurements.
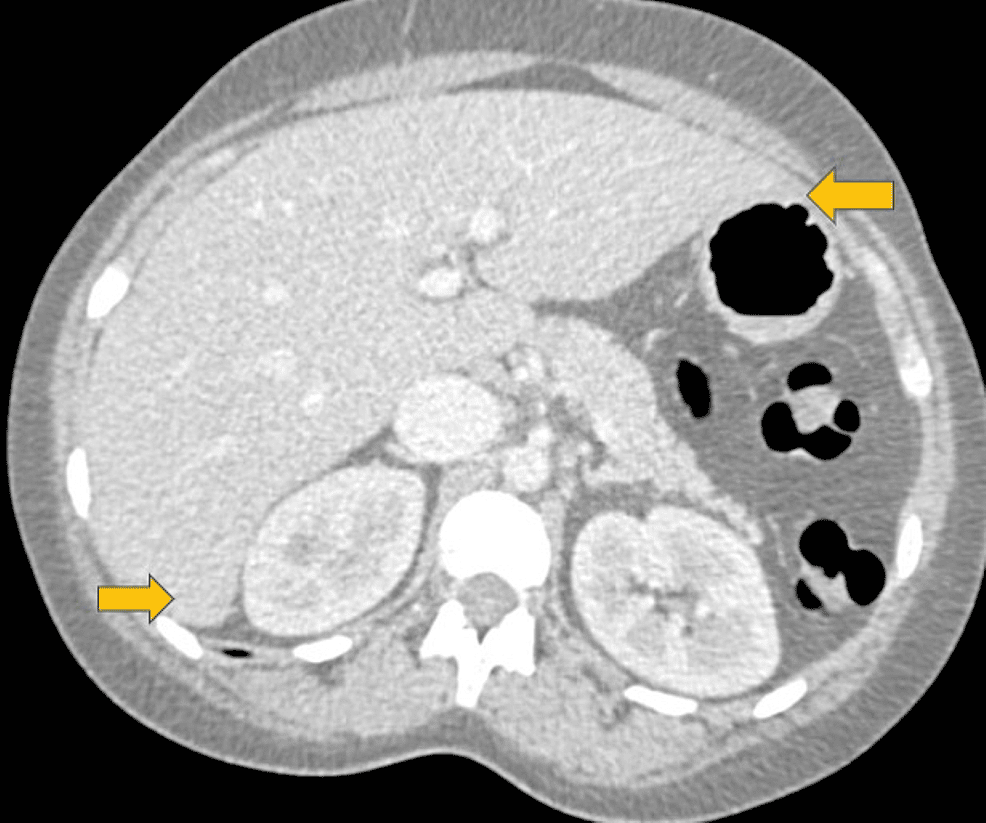
Appropriate imaging studies include abdominal ultrasound, cross-sectional imaging with CT or MRI scan, and indirect cholangiography. The liver is usually enlarged and splenic infarction characteristic. Irregularity of the liver outline is suggestive of established fibrotic disease. Magnetic resonance cholangiography will identify cholelithiasis and choledocholithiasis as well as cholangiopathic change.
How Do We Define Sickle Hepatopathy
In developed countries, SCD has evolved into a debilitating chronic disorder with significant morbidity because of end-organ damage. The liver is one of the affected organs, resulting in sickle hepatopathy. In SCD, some end-organ damage has a well-recognized natural history with identified treatments: proteinuria and renal impairment, right-sided heart pressures and pulmonary hypertension, and high velocities on transcranial Dopplers and ischemic stroke risk . However, the nature of liver dysfunction in SCD has not been characterized, nor has the natural history and pathogenesis of the liver disease been fully defined. This lack of knowledge prevents specific monitoring and deciding when, how, and in whom to intervene.
Hepatobiliary Manifestations Of Scd
SCD can involve multiple organ systems including the gastrointestinal tract. These gastrointestinal manifestations usually occur due to small vascular infarcts and microvascular occlusion and ischemia presenting as abdominal crisis with severe pain, acute pancreatitis, peptic ulcer disease and rarely ischemic bowel. The hepatobiliary system is one of the most common intra-abdominal organs involved in SCD and hepatic involvement is observed in 10%-40% cases of sickle cell crisis.
Clinically, the diagnosis and appropriate management of hepatobiliary manifestations of SCD is challenging as they may present in myriad ways along a spectrum from relatively benign such as gallbladder sludge to as lethal as acute liver failure. The objective of this review is to describe the hepatobiliary manifestations of sickle cell disease with emphasis on their pathophysiology and clinical manifestations. We also organize and discuss existing clinical terminologies used to describe these hepatobiliary manifestations.
Recommended Reading: Hepatitis C Screening Guidelines 2020
What Is Appropriate Management Of Sickle Hepatopathy
The management of sickle hepatopathy relies on accurate identification and treatment of any coexisting cause. The diverse etiologies contribute to the extensive variation in natural history and severity of liver disease. Joint management involving a hepatologist with an interest in SCD is useful.
Investigation.
It is important to exclude other causes of liver dysfunction in SCD including alcohol, medication , and BMI evaluation .
In any liver disease, the first imaging investigation is an abdominal ultrasound the technique is accurate in assessment of the presence of cirrhosis, ascites, portal vein anatomy, biliary calculi, and biliary dilatation. Ultrasound is also the most sensitive imaging technique for assessment of acute calculous cholecystitis with a positive predictive value of 95% when gallbladder wall thickening is more than 3.5 mm and gallstones are present. Abdominal CT is useful in diagnosing complications of biliary disease, perforation, emphysematous cholecystitis, cholangitis, and liver abscess. MRCP is the imaging technique of choice in the diagnosis of cholangiopathy it is noninvasive, accurate, and predicts the need for ERCP to allow intervention regarding common bile duct calculi and dominant stricture. The accuracy of MRCP for detecting biliary calculi is 98%. MRCP is comparable with ERCP for the diagnosis of primary sclerosing cholangitis but less effective in diagnosis of dominant strictures.
Treatment options for specific complications.
Presentation Of Acute Scic
Acute SCIC presentations vary, but manifestations are characterized by progressive liver failure. Patients characteristically have elevated total bilirubin, variable changes in liver function tests, and upper abdominal pain. Many patients without underlying hepatic disease have significant improvement with RBCEx therapy, though mortality has been described despite intervention . We present a case report of a patient we saw in our clinic.
Read Also: What Are The First Signs Of Hepatitis C
Results Of Laboratory Information System Query
No liver biopsy specimens with acute SCIC were identified. A single autopsy case was signed out as acute SCIC however, upon review of the materials and medical records, this more likely represented another etiology of hepatic failure in an SCD patient, as there was no pronounced hyperbilirubinemia reported or significant sickling or cholestasis in the submitted liver sections
Presentation Of Chronic Scic With Acute Exacerbation
Chronic SCIC is less well characterized, but patients routinely have variable baseline liver dysfunction with intermittent exacerbation. Few cases have been previously described. Patients present with chronically elevated bilirubin, as is characteristic of SCD, likely due to baseline hemolysis as well as liver dysfunction . We herein present a case report of a patient we saw in routine practice and followed thereafter.
Also Check: How Many Hepatitis C Genotypes Are There
Types Of Sickle Cell Crisis
There are several conditions that are defined as sickle cell crisis, and they can cause sudden, severe, and sometimes dangerous effects.
The major common types of sickle cell crisis are:
- Vaso occlusive pain: This type is considered the most common. It occurs when the red blood cells form a sickle shape and block small blood vessels. This can cause extreme pain in the affected areas of the body.
- Acute chest syndrome: This type can occur when the small blood vessels of the lungs become blocked by sickle-shaped red blood cells. It can cause shortness of breath, low oxygen levels, and it can be fatal.
- Aplastic crisis: This condition occurs when the bone marrow slows or stops making red blood cells, leading to severe anemia .
- Splenic sequestration: This occurs when the red blood cells accumulate in the spleen. It causes enlargement of the spleen and severe anemia.
- End organ damage: The sickled cells can accumulate in the blood vessels of any organ, causing pain and organ damage. Examples include priapism , intestinal ischemia , and stroke .
Sickle cell disease has other health effects that are not considered sickle cell crisis, including anemia, a predisposition to infection, a risk of serious complications such as kidney and liver damage, and avascular necrosis .
Can You Prevent Sickle Cell Crisis
Sickle cell crisis can cause substantial distress, and it takes at least a few days to resolve. Sometimes a sickle cell crisis can be dangerous. Preventive therapies can help reduce the severity and frequency of sickle cell crises for people who have sickle cell disease.
Prevention includes medical interventions and lifestyle approaches. Medical interventions that treat sickle cell anemia may reduce the frequency of crises and include hydroxyurea, L-glutamine, chronic blood transfusion, and stem cell transplant .
Oxbryta , a drug that prevents the red cells from sickling, has received accelerated approval by the Food and Drug Administration for clinical use in people ages 4 and up.
Other potential treatments are being investigated in research trials, including anti-inflammatory treatments, Dacogen and tetrahydrouridine , and gene therapy .
Lifestyle approaches for preventing sickle cell crisis include:
- Stay hydrated, especially after exercise, during an infection, or during any medical illness.
- Reduce the risk of infections with methods such as frequent handwashing, avoiding close contact with people who you know have an infection, and staying up to date on recommended vaccinations.
- Maintain stable temperatures by wearing gloves, hats, and other temperature appropriate clothes as needed.
- Exercise in moderation.
- Avoid high altitudes, where there is low oxygen.
Recommended Reading: How Much Is Hepatitis A Vaccine
Acute And Chronic Hepatobiliary Manifestations Of Sickle Cell Disease: A Review
Correspondence to: Saurabh Chawla, MD, Assistant Professor of Medicine, Division of Digestive Diseases, Department of Internal Medicine, Emory University School of Medicine, Faculty Office Building, 49 Jesse Hill Jr. Drive, Suite 431, Atlanta, GA 30322, United States.
Telephone: +1-140-47781684 Fax: +1-140-47781681
Endari Approved To Treat Sickle Cell In Adults Children In Qatar
Raising access to SCD treatment in ‘large and underserved’ areas of world
The Qatar Ministry of Public Health has approved Endari to treat adults and children, starting at age 5, with sickle cell disease , the therapys developer, Emmaus Life Sciences, announced.
We are grateful that Qatari officials made access to Endari easier for the sickle cell patients in the country, Yutaka Niihara, MD, chairman and CEO of Emmaus, said in a press release.
Don’t Miss: How Is Hepatitis B Diagnosed
What Is The Role Of Lt
Worldwide experience of LT as a therapeutic modality for end-stage liver disease as a consequence of sickle hepatopathy is slowly developing, with 22 cases reported in the literature.,,, However, several questions remain unanswered. The poor results reported in early case series have improved, to some degree, in later studies. This is likely a consequence of better patient selection and improved perioperative management of SCD.
Currently, end-stage liver disease as a consequence of sickle hepatopathy is not an accepted indication for LT in the United Kingdom. A pilot study is underway to define the role of this treatment modality in this group of patients. We would recommend that patients approaching end-stage liver disease be referred to centers where joint hematologic and hepatological assessment can be performed and patients offered the full range of treatment options.
Our experience in the United Kingdom represents a well-resourced setting with well-established infrastructure within hematology and hepatology. LT is a difficult option for those in poorly resourced settings. Transplantation planning must not only take into account the workup and surgery itself, but also consider postoperative multidisciplinary care involving hematology and EBT, and the logistics and side effects of immunosuppression.
The Definition Of Hepatic Crisis Is Not Always Precise And The True Incidence May Be Lower Than
Mozygous sickle cell disease, with gallstones being present in up to 58% of patients aged 10 to 65 years versus 17% in patients with hb sc disease and hb s bthalassemia.25 chole. Sickle cell disease is a group of inherited red blood cell disorders affecting about 1 in 500 african american children and 1 in 36,000 hispanic american children. scd. Sickle cell disease can cause progressive injury to the liver with significant fibrosis, often cirrhosis, and decreased liver function by adulthood.
You May Like: Hepatitis C Viral Rna Genotype Lipa
Pulmonary Crises And Multiorgan Failure Syndrome
Causes and mechanisms of acute chest syndrome . Vaso-occlusive crises precede ACS in 80% of cases and are characterized by red blood cell sickling, cellular hyperadhesion, hemolysis, and vaso-occlusion. These processes are responsible for acute pain and bone marrow necrosis. ACS typically occurs 2.5 days after hospitalization for a vaso-occlusive episode, and radiographically presents as new infiltrates on a chest radiograph. Common causes include fat embolization from necrotic marrow , pulmonary infection , pulmonary infarction , and hypoventilation. In situ pulmonary thrombosis has been identified in 17% of patients with ACS and may also be responsible for infarction. Animal models have shown that by-products of hemolysis, such as heme, cause experimental ACS. As a result of lung injury, ventilation-perfusion mismatches and shunting ensue, with subsequent hemoglobin desaturation and hypoxemia. Tissue hypoxia in turn triggers further sickling in a vicious cycle. The chest radiographs are those of a patient with SCD who received chronic exchange transfusions on hospital day 1 and day 3 . By day 3 extensive infiltrates had developed in the patient, who required endotracheal intubation for respiratory failure. PLT = platelet.
Complications Of Sickle Cell Disease
People with sickle cell disease start to have signs of the disease during the first year of life, usually around 5 months of age. Symptoms and complications of SCD are different for each person and can range from mild to severe. People with SCD can experience different complications, but some of the common ones are listed below.
Don’t Miss: Hepatitis B Surface Antigen Antibody
How Can It Be Diagnosed
The diagnosis is defined according to the following criteria:
AST, ALT and lactic dehydrogenase levels are markedly elevated. The ALT/LDH ratio is generally less than 1.5 which helps distinguish ischemic hepatitis from other forms of hepatitis.
ALT, AST and LDH generally peak 13 days after the precipitating event and return to normal values in 710 days after the blood supply to the liver is restored.
An increase in the level of bilirubin in the blood may be seen a few days after transaminases reach their peak .
What Are The Treatments For Sickle Cell Crisis
In general, sickle cell crisis is managed symptomatically. Most of the time, pain medication is prescribed.
If you are able to experience pain relief with over-the-counter medication, your healthcare provider will let you know how much you can safely take. Some powerful prescription medications that are commonly used to treat a sickle cell crisis, such as morphine, can have severe side effects, including profound constipation.
Pain control is important, and your healthcare providers will give you prescription-strength oral or intravenous medication to reduce your pain if OTC pain medications are not sufficient.
Other treatments that you might need include:
- Intravenous fluids
- Supplemental oxygen
- Blood transfusion
If you need to be admitted to the hospital for your treatment, your condition would be monitored closely, and your treatment would be adjusted as needed.
Also Check: Hepatitis B Surface Antibody Qualitative
Evaluation Of Sickle Cell Liver Disease
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : September 25, 2013Last Update Posted : May 16, 2022 |
Background:
– Sickle cell disease changes the shape of red cells. This makes them more likely to break down as they get stuck in small blood vessels. This leads to low red cell count and also damage to small blood vessels that supply many organs. One of the affected organs is the liver. Sickle cell disease and its treatment through blood transfusion can lead to significant liver damage. This disease also can cause the liver to regrow abnormally after damage. This can cause high blood pressure in the liver. Researchers want to know if curing sickle cell disease with a stem cell transplant improves liver damage.
Objectives:
– To explore specific factors that improve or worsen sickle cell liver disease after a stem cell transplant.
Eligibility:
– Adults ages 18 and older with sickle cell liver disease.
Design:
| Sickle Cell Disease |
Sickle cell disease causes multi-organ dysfunction and early death in affected individuals. Many succumb to complications of chronic organ dysfunction and eventual organ failure one of which is the liver.
| Non-Probability Sample |
Deterrence And Patient Education
Patient education is important for SCD and even more critical for SCH, as there is not much easily accessible information for patients on SCH. Patients should be taught to know signs of acute sickle cell crisis, one component of which can be acute hepatic crisis, requiring hospitalization. Further, patients should be encouraged to have regular follow-ups with their hematologists or primary care physicians. They should have regular laboratory investigations that include liver function tests, so that hepatic function can be monitored, with any abnormalities necessitating further workup.
Patients should also be educated on gallstones, which is a common occurrence. They should be aware of the signs, such as right upper quadrant pain that is worse with eating greasy foods. They should avoid fatty and spicy foods, and if it is a recurrent problem, they should be educated on possible surgery. Patients with SCH should also be educated on the need for vaccines such as Hepatitis A and B. Patients who show milder forms of SCH should be educated on the signs and symptoms of cirrhosis. They should continue close follow-up with their healthcare providers so that this is not missed.
Recommended Reading: How Long Can Someone Live With Hepatitis C
Which Is The Prognosis Of Hepatic Ischemia
If the disease causing the liver ischemia can be reversed quickly the prognosis is usually good with a complete recovery.
However, the overall prognosis is poor with mortality rates of at least 25% because hepatic ischemia is usually seen along with serious disorders such as sepsis, acute renal failure or coagulopathies. Hepatic ischemia can sometimes lead to liver failure.
Medically reviewed by our Medical staff on 22-11-2022
What Causes Liver Disease In Patients With Sickle Cell Disease
Sickle hepatopathy is an umbrella term, encompassing the range of liver disease encountered in patients with sickle cell anemia. As such, it includes diverse hepatic pathology arising from a variety of insults to the liver that can occur in these patients. It occurs predominantly in patients with homozygous HbSS disease, and to a lesser extent in patients with hemoglobin SC disease or HbS -thalassemia. Liver disease can result from:
the effects of sickling of erythrocytes within the vasculature of the liver, with consequent hypoxic liver injury, particularly affecting the centrilobular region and biliary system
complications related to the multiple blood transfusions some patients require, including viral hepatitis and iron overload
gallstones, causing gallbladder pathology and biliary obstruction or
coincidental liver pathology .
Recommended Reading: How Serious Is Hepatitis B
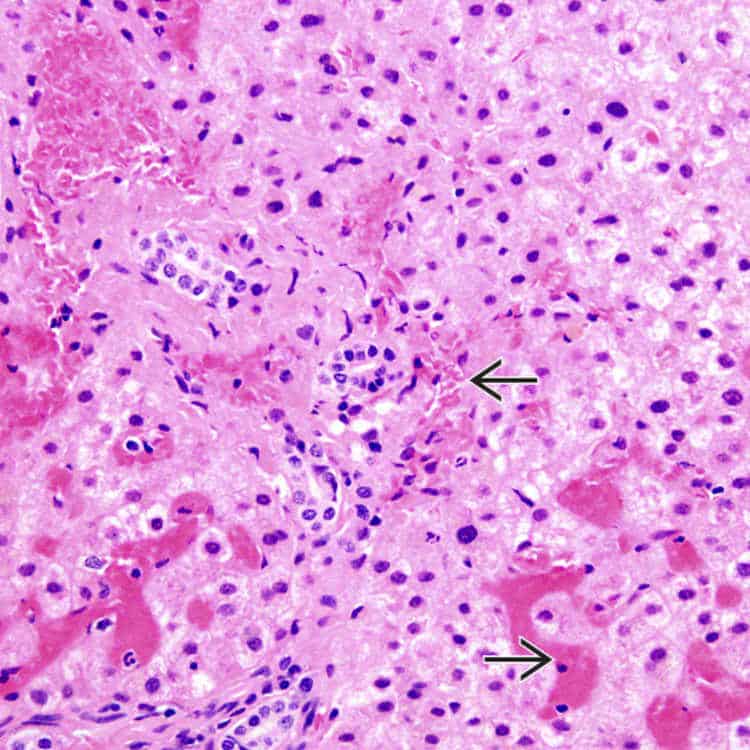
The Role Of Liver Biopsy
This is an important clinical question. The histologic changes occurring in acute and chronic liver disease in patients with SCD have been characterized: sinusoidal obstruction due to sickling with variable centrilobular and hepatocyte damage in the acute syndromes, and cholangiopathy, biliary type cirrhosis, and iron overload in the chronic setting. However, percutaneous liver biopsy can be associated with increased risk of complications in SCD, principally hemorrhage. In a series from our center, 36% of patients undergoing liver biopsy developed severe bleeding complications and 28% died. The majority of patients who developed complications were in acute sickle crisis at the time of the biopsy. Importantly, the authors did not feel that histology significantly changed the management of these patients.