Cdc Recommendations For Hepatitis C Screening Among Adults In The United States
- Universal hepatitis C screening:
- Hepatitis C screening at least once in a lifetime for all adults aged 18 years and older, except in settings where the prevalence of HCV infection is less than 0.1%*
- Hepatitis C screening for all pregnant women during each pregnancy, except in settings where the prevalence of HCV infection is less than 0.1%*
- Any person who requests hepatitis C testing should receive it, regardless of disclosure of risk, because many persons may be reluctant to disclose stigmatizing risks
Hepatitis C Virus Infection In Adolescents And Adults: Screening
Recommendations made by the USPSTF are independent of the U.S. government. They should not be construed as an official position of the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.
| Adults aged 18 to 79 years | The USPSTF recommends screening for hepatitis C virus infection in adults aged 18 to 79 years. | B |
- View the Clinician Summary in PDF
Management Of Sex Partners
Because incident HCV has not been demonstrated to occur among heterosexual couples followed over time , condom use might not be necessary in such circumstances. Persons with HCV infection with one long-term, steady sex partner do not need to change their sexual practices. However, they should discuss the risk for transmission with their partner and discuss the need for testing . Heterosexual persons and MSM with HCV infection and more than one partner, especially those with concurrent HIV infection, should protect their partners against HCV and HIV acquisition by using external latex condoms and HIV PrEP. Partners of persons with HCV and HIV should be tested for both infections.
Recommended Reading: Can Hepatitis B Virus Be Cured
Hepatitis C Testing Strategy
The goal of hepatitis C screening is to identify persons who are currently infected with HCV. Hepatitis C testing should be initiated with a U.S. Food and Drug Administration -approved anti-HCV test. Persons who test anti-HCV positive are either currently infected or had past infection that has resolved naturally or with treatment. Immunocompetent persons without hepatitis C risks who test anti-HCV negative are not infected and require no further testing. Persons testing anti-HCV positive should have follow-up testing with an FDA-approved nucleic acid test for detection of HCV RNA. NAT for HCV RNA detection determines viremia and current HCV infection. Persons who test anti-HCV positive but HCV RNA negative do not have current HCV infection. CDC encourages use of reflex HCV RNA testing, in which specimens testing anti-HCV positive undergo HCV RNA testing immediately and automatically in the laboratory, using the same sample from which the anti-HCV test was conducted. Hepatitis C testing should be provided on-site when feasible.
Evaluation Of Individuals With Positive Screening Test
Patients with a positive screening test for anti-HCV antibody should be tested for serum HCV RNA. Serum HCV RNA quantifies the amount of viral RNA in serum and indicates ongoing infection. If HCV RNA is detectable, tests should be performed to determine the extent of hepatic fibrosis. These tests typically include liver biopsy or noninvasive measures, such as biochemical markers of fibrosis or transient elastography., An ultrasound of the abdomen should also be performed to identify the possible presence of cirrhosis and focal lesions in the liver suspicious for hepatic malignancy.
Patients who have a positive anti-HCV on a screening test but have no detectable HCV RNA should have a confirmatory HCV RNA test a few months later. If HCV RNA remains undetectable, these individuals should be reassured that they do not have hepatitis C infection and that the anti-HCV may remain persistently positive. Such individuals have either cleared the virus or the true specificity of the test is lower than the reported 100%, and the test result was a false positive.
You May Like: Hepatitis B Surf Ab Quant 3.1 Low
You May Like: What Age Do You Get Hepatitis B Vaccine
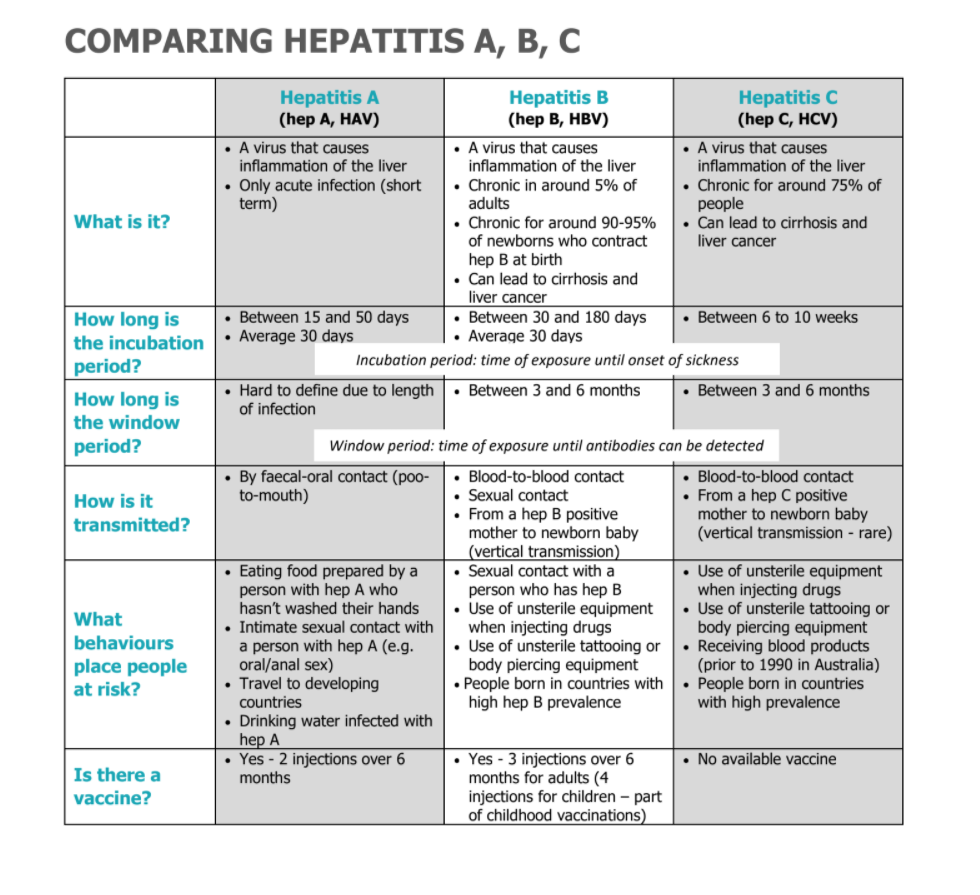
What Is Hepatitis C
Hepatitis C is a liver disease caused by the hepatitis C virus. Hepatitis C can cause a mild illness of a few weeks or develop into a serious, lifelong, chronic illness. It is a major cause of cancer and cirrhosis of the liver, and if not treated, it can be fatal.
Hepatitis C is transmitted through exposure to small quantities of blood. People who inject drugs are at particular risk. About 30% of people infected clear the virus within 6 months without treatment. The remaining 70% develop chronic hepatitis C and for these, the risk of liver cirrhosis ranges between 15% and 30% within 20 years. 75% of those reported as living with chronic hepatitis C live in low- and middle-income countries.
Recommended Reportable Laboratory Markers
The following laboratory markers are recommended for reporting to public health to aid in case ascertainment, case classification, and monitoring cure continua for hepatitis C:
- HCV RNA , including quantitative, qualitative, and genotype testing
- HCV antigen when and if a test is approved by FDA and
- If any of the above positive results are reported, also report the following:
- Pregnancy status,
- Concurrent ALT and total bilirubin results,
- Other hepatitis serological results .
Jurisdictions are strongly encouraged to incorporate the reporting of negative/undetectable HCV RNA test results into their surveillance regulations and systems to support improved understanding of their local epidemic. Such reporting may increase awareness regarding
- acute infections and cleared infections,
- completeness of testing, and
- availability of reflex testing.
Jurisdictions might also wish to receive negative anti-HCV results to assist in identifying cases of test conversion and examine trends in screening however, they must be mindful of their ability to process and store high volumes of data. Further, caution must be taken in the collection and use of these results, as people with non-reactive anti-HCV tests do not have a reportable condition. Jurisdictions must have legal authorization for receipt of these data.
Recommended Reading: How Serious Is Hepatitis C
Recent Increases In Hepatitis C Infections
Between 2013 and 2020, the reported number of acute HCV infections more than doubled. High rates of new infections were predominantly among young adults aged 20-29 years and aged 30-39 years. The number of cases continues to increase, in 2020 an estimated 66,700 new HCV infections occurred in the United States. For the most recent surveillance data visit CDC Viral Hepatitis Surveillance.
Benefits Of Early Detection Or Treatment
The USPSTF found no direct evidence on the benefits of HCV screening vs no screening on health outcomes or the effects of prenatal HCV screening on the risk of vertical transmission.1 Treatment studies focused on populations without cirrhosis who are more likely to be asymptomatic and identified by screening. Of the trials of DAA regimens , 14 were multinational 11 were conducted in the US or Canada and the remainder were conducted in New Zealand, Egypt, France, or Asia. In 29 trials, 60% to 100% of patients were white.1 The trials evaluated a variety of DAA regimens recommended in current guidelines. Treatment duration was 12 weeks in all but 2 trials, which allocated patients to either 8 or 12 weeks of treatment. Eleven trials were of good quality and 22 were of fair quality. Forty-nine trials found DAA regimens to be associated with pooled SVR rates ranging from 95.5% to 98.9% across genotypes. Evidence was greatest for genotype 1 infection , the most frequent genotype in the US.1 Sustained virologic response rates were similar in trials that stratified patients according to age, sex, race/ethnicity, or treatment experience with non-DAA regimens.1
Recommended Reading: Natural Treatment For Hepatitis C
Also Check: Hepatitis B Dosage For Adults
Summary Of The Literature
For the all-adult review, the initial literature search yielded 4,867 studies. Twenty-nine duplicates were identified. Of 4,838 unique studies, 4,170 were deemed irrelevant by title/abstract screening, resulting in 668 full texts for review. Among these, 368 studies had data available to extract.
For the pregnancy review, the initial literature search yielded 1,500 studies. Two duplicates were identified. Of 1,498 unique studies, 1,412 were deemed irrelevant by title/abstract screening, resulting in 86 full texts for review.
The supplementary review yielded an additional 1,038 and 195 studies among all adults and pregnant women, respectively. Of these, 912 and 168 , respectively, were deemed irrelevant by title/abstract screening, resulting in 126 and 27 , respectively, full texts for review. One study was added to the pregnant women review outside of the formal literature search .
Considering all 104 applicable studies, the median anti-HCV positivity prevalence among all adults was 6.6% . Median anti-HCV positivity prevalence was 1.7% for the general population , 7.5% for ED patients , 3.3% for birth cohort members , 9.3% for others/multiple risk factors , 54.2% for persons who use drugs , 5.2% for persons with HIV or sexual risk , and 4.7% for immigrants . Considering 26 applicable studies among pregnant women, median anti-HCV positivity prevalence was 1.2% .
Recommended Reading: How Do You Get Hepatitis A
Benefits Of Screening For Hepatitis C
If individuals with chronic hepatitis C are identified before they develop advanced fibrosis, cirrhosis, or hepatocellular carcinoma, 90%-100% can now be expected to respond to treatment, whereas previously only 66%-75% of individuals responded to treatment.-,- Thus, detecting individuals with hepatitis C before they develop signs or symptoms of the disease can have an important impact on their subsequent clinical course. Sustained virologic clearance for more than 6 months after treatment of hepatitis C is also associated with a reduction in all-cause mortality.
Recommended Reading: What Causes Hepatitis C Infection
Interpretation Of Laboratory Test Results
The two tests used primarily for hepatitis C screening and diagnosis are an antibody test and an RNA test , respectively . A description of hepatitis C laboratory markers can be found in Appendix B. Figure 4-1 describes the typical serologic course of HCV infection .
Figure 4-1. Typical serologic course of hepatitis C virus infection
In 2013, CDC provided updated guidance on the recommended testing sequence for identifying current hepatitis C . Hepatitis C testing should be initiated with an anti-HCV screening test, and if positive, an HCV RNA test should be performed. In settings serving high-risk populations , rapid anti-HCV testing can be used in lieu of laboratory-based anti-HCV testing to deliver results to the patient at the time of visit. For people who tested anti-HCV positive through rapid screening, an on-the-spot blood draw to be sent for HCV RNA testing should be performed or a referral and/or evaluation for HCV RNA testing should be provided. For blood draws collected for anti-HCV testing, all positive specimens should reflex to HCV RNA testing to reduce the number of patients lost to follow-up.
Table 4-1. Interpretation of hepatitis C laboratory results
| Test Outcome* |
|---|
Limitations Of Screening For Hepatitis C
Barriers to screening for hepatitis C include limited access to healthcare, inadequate health insurance coverage, individuals decreasing recall of past risky behaviors, lack of knowledge of hepatitis C prevalence, natural history, and available tests and treatments for hepatitis C at the provider level.- Moreover, nearly 42% of primary care physicians reported being unfamiliar with the CDC guidelines in a survey of community-based physicians.
Don’t Miss: Hepatitis C False Positive Antibody
Postexposure Prophylaxis Is Not Recommended
Recent data have shown that the risk for HCV infection from percutaneous exposure is 0.2% and from mucocutaneous exposure is 0%. On the basis of this information, the CDC guidelines do not recommend routine postexposure prophylaxis for HCPs with occupational exposure to HCV. Rather, curative antiviral regimens should be reserved for instances of documented HCV transmission.
The authors have disclosed no relevant financial relationships.
MMWR. Published online July 23, 2020. Full text
Uses Of Surveillance Data
Acute and chronic hepatitis C surveillance data can be used to inform and improve public health interventions in the following ways:
You May Like: What Is Hepatitis B Shot
What Are Current Treatments For Hepatitis C
Pegylated-interferon with ribavirin
- 40-80% cure rate
- long treatment duration
- complex management of the treatment
- administered by injection
- difficult to access in some settings.
Direct acting antivirals
- highly effective
- safer and better tolerated than existing therapies
- shorter treatment duration
- oral formulation
- simpler monitoring and laboratory requirements
- access is quite limited, mostly because of high cost
Cases And Clusters Of Potential Public Health Importance
Jurisdictions should review and analyze hepatitis C data regularly to identify cases and clusters of hepatitis C that merit further investigation. When resources are limited, these should be prioritized for investigation according to degree of public health importance. The following are examples of high priority cases and clusters:
- People of childbearing age who are or have the potential to become pregnant, indicating the potential risk for perinatal transmission.
- Children 36 months of age, indicating possible perinatal transmission.
- People in age and demographic groups among whom infection might be acute due to recent transmission. This includes people
- < 40 years of age and
- > 70 years of age .
Recommended Reading: Natural Cure For Hepatitis A
How Is Hepatitis C Diagnosed
Hepatitis C infection is diagnosed in two steps:
- A serological test is used to test for hepatitis C antibodies, produced by the body to fight the infection.
- A nucleic acid test is used to test for hepatitis C ribonucleic acid to confirm chronic infection. This test is needed because about 30% of people infected with hepatitis C whose infection clears up by itself will still test positive for hepatitis C antibodies long after they are no longer infected.
Existing diagnostic tests remain too complex and/or too expensive for countries with limited budgets, weak health systems, or both. Simple, more affordable tests are needed.
We are working with FIND and the Ministry of Health in Malaysia to simplify hepatitis C screening and make it more widely available.
Case Reporting And National Notification
Cases of acute, chronic, and perinatal hepatitis C and hepatitis C during pregnancy should be reported to HDs as specified by state, territorial, or local regulations. Acute, chronic, and perinatal hepatitis C are nationally notifiable conditions . Hepatitis C cases are identified using an event code corresponding to the hepatitis C condition . Data are sent weekly or more frequently, depending on the infrastructure of the jurisdiction sending the data. Cases might be re-classified or removed as needed after the initial transmission to CDC, as long as the changes occur before surveillance data are finalized each year.
Also Check: Hepatitis B Vaccine Cost Cvs
How Do You Get Hepatitis C
Hepatitis C is a blood-borne virus. The most common ways to get infected are:
- unsafe injection practices
- inadequate sterilization of medical equipment
- blood transfusions of un-screened blood or blood products
Hepatitis C can also be transmitted sexually and be passed from mother to child, but these types of transmission are less common.
Considerations For Hepatitis C Cases Who Were Transplant Recipients
With the availability of curative treatment for HCV infection, an increasing number of transplant recipients are receiving organs from anti-HCV and HCV-RNA positive donors . This can result in transmission of hepatitis C to the recipient, which is then treated with DAA agents . In some jurisdictions, these expected donor-derived HCV transmissions might represent a significant proportion of new acute HCV infections therefore, jurisdictions are encouraged to reach out to transplant facilities and discuss public health reporting of expected donor-derived HCV infections.
A listing of transplant facilities in the United States, including facility location and phone number, can be found on the OPTN websiteexternal icon . As these patients are already linked to testing and treatment, the infections should be notified to CDC as new acute cases. However, the jurisdiction need not investigate beyond indicating that the infection was donor-derived.
Typically, there are two outstanding questions that only the public health jurisdiction can answer: 1) Did the recipient have any behavioral or other risks for hepatitis C and 2) Does the jurisdiction have any ongoing investigations of health care-associated hepatitis C that might be related to this investigation?
Table 4-3. Considerations for hepatitis C cases who were organ transplant recipients*
| Organ Recipient Pre-transplant |
|---|
You May Like: Is Hepatitis B The Same As Hiv