What Is Hepatitis B
Hepatitis B is an infection of your liver. Itâs caused by a virus. There is a vaccine that protects against it. For some people, hepatitis B is mild and lasts a short time. These âacuteâ cases donât always need treatment. But it can become chronic. If that happens, it can cause scarring of the organ, liver failure, and cancer, and it even can be life-threatening.
Itâs spread when people come in contact with the blood, open sores, or body fluids of someone who has the hepatitis B virus.
It’s serious, but if you get the disease as an adult, it shouldnât last a long time. Your body fights it off within a few months, and youâre immune for the rest of your life. That means you can’t get it again. But if you get it at birth, itâ unlikely to go away.
âHepatitisâ means inflammation of the liver. There are other types of hepatitis. Those caused by viruses also include hepatitis A and hepatitis C.
Complications Of Hepatitis B
A small proportion of people who become infected with the hepatitis B virus develop a long-term hepatitis B infection. They may have the virus in their bloodstream for most of their life without realising they are infected.
People with chronic hepatitis B infection may not notice any health problems until they develop liver problems such as liver disease or liver cancer later in life. Treatment for hepatitis B is essential because it is not possible to be a healthy carrier of the hepatitis B virus. Chronic hepatitis B infection occurs more commonly in some communities, including:
- Aboriginal and Torres Strait Islander communities.
- In people from parts of the world where hepatitis B is more common, such as:
- North-East Asia
- Sub-Saharan Africa.
What Are The Risk Factors For Getting Hepatitis B
Due to the way that hepatitis B spreads, people most at risk for getting infected include:
- Children whose mothers have been infected with hepatitis B.
- Children who have been adopted from countries with high rates of hepatitis B infection.
- People who have unprotected sex and/or have been diagnosed with a sexually transmitted infection.
- People who live with or work in an institutional setting, such as prisons or group homes.
- Healthcare providers and first responders.
- People who share needles or syringes.
- People who live in close quarters with a person with chronic hepatitis B infection.
- People who are on dialysis.
Don’t Miss: What Organ Does Hepatitis Affect
What Occupations Have Increased Risk Of Hepatitis B
In general, occupational groups with increased risk include:
- Health-care workers repeatedly exposed to blood or blood products or those who are at risk of needlestick injury.
- Pathologists, laboratory personnel, or embalmers.
- Dentists, dental assistants, and dental hygienists.
- Certain staff members of institutions for the developmentally handicapped.
- Staff of institutions where workers may be exposed to aggressive, biting residents.
Travellers to regions with intermediate or high rates of endemic HBV infection may also consider being vaccinated.
Exposure To A Source With Unknown Hbsag Status
Unvaccinated persons and persons with previous nonresponse to hepatitis B vaccination who have a discrete, identifiable exposure to blood or body fluids containing blood from a person with unknown HBsAg status should receive the hepatitis B vaccine series, with the first dose initiated as soon as possible after exposure and the series completed according to the age-appropriate dose and schedule. Exposed persons who are not fully vaccinated but started the series should complete the vaccine series. Exposed persons with written documentation of a complete hepatitis B vaccine series who did not receive postvaccination testing require no further treatment.
Recommended Reading: What Is Genotype 3 Hepatitis C
Cases And Clusters Of Potential Public Health Importance
Jurisdictions should review and analyze hepatitis B data regularly to identify cases and clusters of hepatitis B that merit further investigation. When resources are limited, these should be prioritized for investigation based on the degree of public health importance. The following are examples of high priority cases and clusters:
- People of childbearing age who are or have the potential to become pregnant, indicating the potential for perinatal transmission
- Children 24 months of age to detect perinatal transmission
- People in age and demographic groups for whom infection may be acute due to recent transmission, including those
- 70 years of age
Also Check: Can Hepatitis C Cause Diarrhea
Acute Vs Chronic Hepatitis B
A hepatitis B infection can result in either an acute infection or a chronic infection. When a person is first infected with the hepatitis B virus, it is called an “acute infection” . Most healthy adults that are infected do not have any symptoms and are able to get rid of the virus without any problems. Some adults are unable to get rid of the virus after six months and they are diagnosed as having a “chronic infection.” A simple blood test can diagnose an acute or chronic hepatitis B infection.
The risk of developing a chronic hepatitis B infection is directly related to the age at which a person is first exposed to the hepatitis B virus. The younger a person is when they are first infected, the greater the risk of developing a chronic hepatitis B infection:
- More than 90% of infants that are infected will develop a chronic hepatitis B infection
- Up to 50% of young children between 1 and 5 years who are infected will develop a chronic hepatitis B infection
- 5-10% of healthy adults 19 years and older who are infected will develop a chronic hepatitis B infection
The recommendation for hepatitis B vaccination of babies and children is so important because they are at the greatest risk of developing a chronic infection if they are not protected against the hepatitis B virus as soon as possible.
You May Like: How Do You Know If You Get Hepatitis C
Where Is The Hepatitis B Virus Found And How Is It Transmitted
Blood is the major source of the hepatitis B virus in the workplace. It can also be found in other tissues and body fluids, but in much lower concentrations. The risk of transmission varies according to the specific source. The virus can survive outside the body for at least 7 days and still be able to cause infection.
Diagnosis Of Hepatitis B
Blood tests are available to determine if you are or have been infected with hepatitis B. It may take 6 months from the time of infection before a blood test can detect antibodies to hepatitis B, so follow-up testing may be required. During this 6-month period, until you know whether you are infected or not, take action to prevent potential infection of other people.
There are also tests that can assess liver damage from hepatitis B. The interpretation of these tests can be complicated and specialist advice is needed, so talk to your doctor.
All pregnant women are tested for hepatitis B. If you are found to have chronic hepatitis B, your doctor can help reduce the risk of transferring the infection to your newborn child.
Also Check: How Do You Get Rid Of Hepatitis B
Informed Consent And Ethical Evaluations
All procedures used were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964, as revised in 2008. Informed consent for the observational process was obtained from all patients before inclusion in the study. The observational protocol was approved by the institutional review board or ethics committee before study initiation.
How You Can Get Hepatitis B
You can get hepatitis B from:
- injecting drugs using shared needles
- being injured by a used needle
- having a tattoo or piercing with unsterilised equipment
- having a blood transfusion in a country that does not check blood for hepatitis B. Blood transfusions in the UK are checked for hepatitis B.
If youâre pregnant and have hepatitis B, you can also pass it onto your baby during pregnancy or birth.
Recommended Reading: Patient Has Immunity To Hepatitis B Virus
Recommended Reading: How Can You Catch Hepatitis B
Symptoms Of Hepatitis B
Some people who are infected with the hepatitis B virus have mild, flu-like symptoms and some do not become sick at all. Children who are infected are less likely to have an illness or get sick after getting hepatitis B than adults.
In more severe cases, hepatitis B can cause:
- Loss of appetite.
- Pain in the joints.
Normally, these health problems disappear in a few weeks, but even when the person feels much better, they may still be infectious.
Most adults who become infected with the hepatitis B virus recover completely and do not become infected again. A few people become very ill in the time just after infection and need to go to hospital some may even die.
Administration Eyes National Hepatitis C Treatment Plan
- SANDHYA RAMANCQ-Roll Call
WASHINGTON The Biden administration is preparing a comprehensive initiative to fight hepatitis C that would streamline testing and treatment and secure an agreement with drugmakers to bring down the cost of treatment of the disease, which has spiked during the pandemic.
Francis Collins, special project adviser to President Joe Biden and former longtime director of the National Institutes of Health, said this week that the administration hopes to secure some funding this year for the yet to be formally unveiled initiative.
He said he briefed Biden on the plan, and the Office of Management and Budget is enthusiastic about figuring out how to fit this into the budgetary requests.
The plan, he said, would include agencies including the Centers for Disease Control and Prevention, Substance Abuse and Mental Health Services Administration, the Indian Health Service, Food and Drug Administration and the Federal Bureau of Prisons.
Recommended Reading: Glomerulonephritis Due To Infectious Hepatitis
Prognosis Improvement After Hbsag Clearance
These related studies provide clear recommendations that patients who achieve HBsAg clearance have favourable clinical outcomes compared to patients who achieve only HBV DNA suppression and HBeAg seroconversion. HBsAg clearance leads to biochemical, virological and liver histological improvements, and it significantly reduces the risk of HCC. However, HCC may occur after HBsAg seroclearance despite it being the ultimate treatment endpoint recommended by current guidelines. The risk factors associated with HCC include the presence of cirrhosis, male sex, and age50 years at the time of HBsAg clearance . Closer attention should be given to patients with one or more of these risk factors.
These high-risk patients should be re-examined in a timely manner even if HBsAg clearance is obtained. These results also suggest that achieving a functional cure early in the absence of cirrhosis results in a better prognosis .
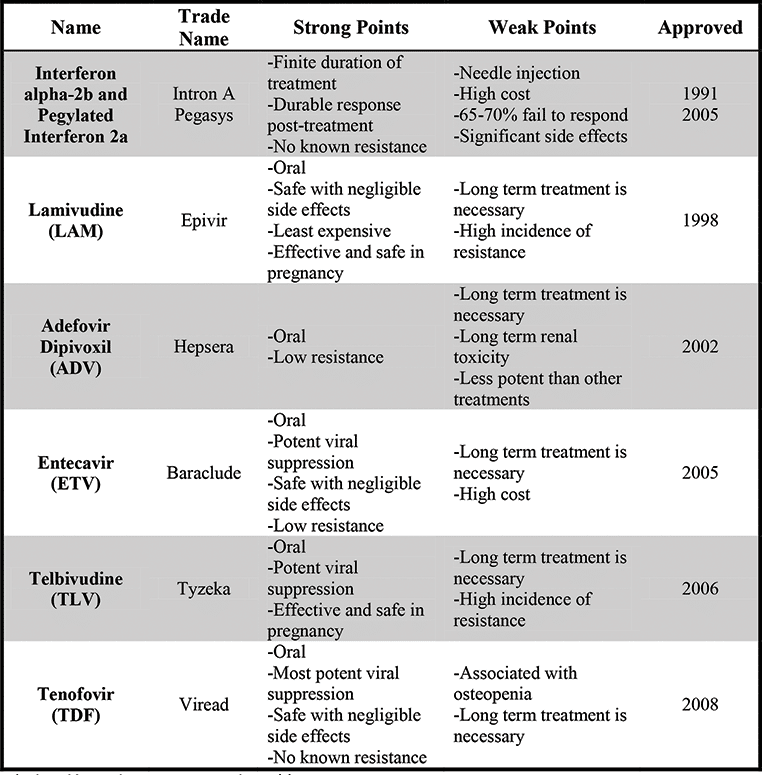
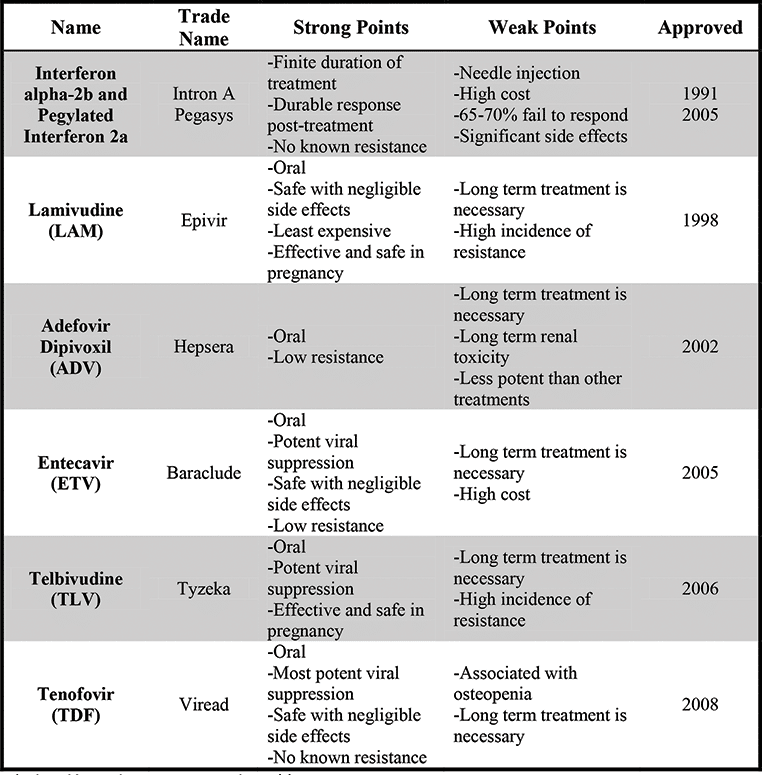
Indications For Antiviral Therapy
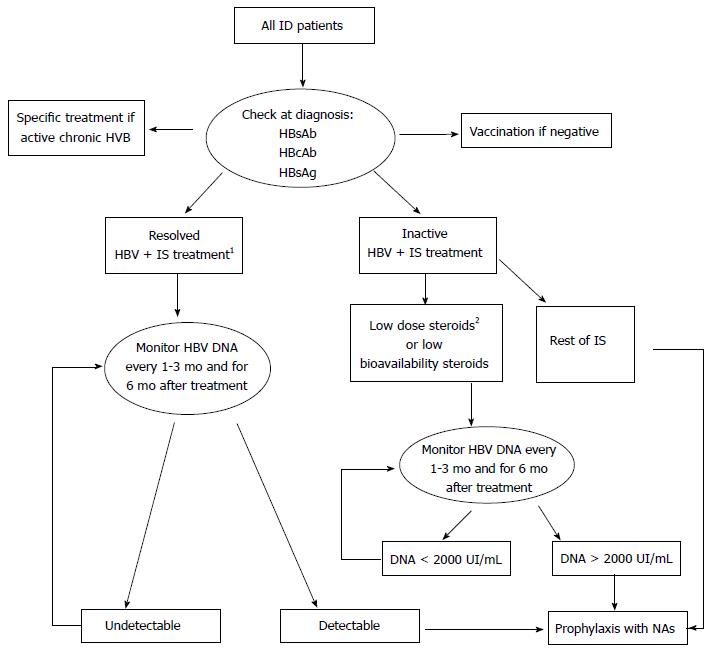
Patients should be assessed for the risk of disease progression to determine whether to start antiviral therapy based on a comprehensive analysis of serum HBV DNA levels, ALT levels, the severity of liver disease, as well as their age, family history, and concomitant diseases.6,112,113 Dynamic assessment is more meaningful than a single test .
Flow chart of antiviral therapy for patients with chronic HBV infection.
Follow-up tests: virological test, liver biochemical test, AFP test, PIVKA-II test, abdominal ultrasound, and liver stiffness measurement. HBV-related extrahepatic manifestations: glomerulonephritis and vasculitis. Follow-up criteria for patients with HBV-related decompensated cirrhosis during NA treatment: perform a routine blood test, liver biochemical test, renal function test, virological test, and test for blood ammonia, AFP, and PIVKA-II, and abdominal ultrasound every 3 months. If necessary, perform enhanced CT or MRI. Other causes of ALT elevation: infection by other pathogens, history of drug or poison use, history of alcohol use, lipid metabolism disorders, autoimmune disorders, liver congestion or vascular diseases, inherited metabolic liver disease, systemic diseases. NAs-ETV, TDF, TAF. HbsAg, hepatitis B surface antigen HBV, hepatitis B virus ALT, alanine aminotransferase HCC, hepatocellular carcinoma NAs, nucleoside analogs peg-IFN-, pegylated interferon-.
Also Check: Is Hepatitis C And Herpes The Same Thing
How Do You Know If You Have Hepatitis B
Signs and symptoms can vary, in particular by the age of the individual. Many individuals may not show symptoms . When symptoms develop, they include fever, joint pain, abdominal pain, fatigue, lack of appetite, nausea, vomiting, dark urine, clay-coloured bowel movements, or jaundice.
Most infections are asymptomatic or mild. Occasionally, people with serious cases of hepatitis B require hospitalization. A very small proportion of these patients develop a critical form of the disease called “fulminant” hepatitis B. This condition results from a sudden breakdown of liver function.
Questions For A Doctor Or Healthcare Professional
A doctor or healthcare professional can give you guidelines on how to best manage your chronic hep B. Together, you can develop a plan that minimizes your chances of complications.
Some questions you may want to ask a doctor include:
- Do I have acute or chronic hep B?
- What do the results of my blood test mean?
- Should I be taking medication?
- What should I do to monitor my disease?
- Are there any clinical trials that Im eligible for?
Recommended Reading: Is Hepatitis B More Infectious Than Hiv
How Is Hepatitis B Diagnosed
There are three main ways to diagnose HBV infection. They include:
- Blood tests: Tests of the blood serum shows how your bodys immune system is responding to the virus. A blood test can also tell you if you are immune to HBV.
- Abdominal ultrasound: An ultrasound uses sound waves to show the size and shape of your liver and how well the blood flows through it.
- Liver biopsy: A small sample of your liver tissue is removed though a tiny incision and sent to a lab for analysis.
The blood test that is used to diagnose hepatitis B is not a test that you get routinely during a medical visit. Often, people whove become infected first learn they have hepatitis B when they go to donate blood. Blood donations are routinely scanned for the infection.
The virus can be detected within 30 to 60 days of infection. About 70% of adults with hepatitis B develop symptoms, which tend to appear an average of 90 days after initial exposure to the virus.
What Causes Hepatitis B
- being born to a mother with hepatitis B
- having unprotected sex with an infected person
- sharing drug needles or other drug materials with an infected person
- getting an accidental stick with a needle that was used on an infected person
- being tattooed or pierced with tools that were used on an infected person and werent properly sterilized, or cleaned in a way that destroys all viruses and other microbes
- having contact with the blood or open sores of an infected person
- using an infected persons razor, toothbrush, or nail clippers
You cant get hepatitis B from
- being coughed on or sneezed on by an infected person
- drinking unclean water or untreated water that has not been boiled
- eating food that is unclean or has not been properly cooked
- hugging an infected person
- shaking hands or holding hands with an infected person
- sharing spoons, forks, and other eating utensils
- sitting next to an infected person
Mothers who have hepatitis B can safely breastfeed their babies. If a baby receives hepatitis B immune globulin and starts receiving the hepatitis B vaccine to prevent hepatitis B infection shortly after birth, hepatitis B is unlikely to spread from mother to child through breastfeeding.15
Read Also: Hepatitis A Vaccine At Cvs
Chronic Hepatitis B Infection
People who test positive for the hepatitis B virus for more than six months are diagnosed as having a chronic infection. This means their immune system was not able to get rid of the hepatitis B virus and it still remains in their blood and liver.
The risk of developing a chronic hepatitis B infection is also directly related to the age at which one first becomes exposed to the hepatitis B virus:
- 90% of infected newborns and babies will develop a chronic hepatitis B infection
- Up to 50% of infected children will develop a chronic hepatitis B infection
- 5-10% of infected adults will develop a chronic hepatitis B infection
Learning that you have a chronic hepatitis B infection can be very upsetting. Because most people do not have symptoms and can be diagnosed decades after their initial exposure to the hepatitis B virus, it can be a shock and a surprise to be diagnosed with a chronic hepatitis B infection. The good news is that most people with chronic hepatitis B should expect to live a long and healthy life.
There are effective drug therapies that can control and even stop the hepatitis B virus from further damaging a liver. There are also promising new drugs in the research pipeline that could provide a cure in the very near future. Although the risk of developing a serious liver disease or liver cancer is higher for those living with chronic hepatitis B than those who are not infected, there are still many simple things a person can do to help reduce their risks.
Hbsag Clearance After Na Treatment
There are few large or conclusive studies on the clearance of HBsAg after NA treatment, and some of these studies are single-centre retrospective studies. Kim et al. reported a clearance rate of 1% or less in 110 CHB patients who were treated with ETV/LAM for approximately 1 year. A retrospective study by Yip et al. reported an HBsAg clearance rate of 2.1% after an average follow-up of 4.8 years in 20,263 CHB patients treated with ETV/TDF for longer than 6 months. Wong et al. retrospectively evaluated 1072 CHB patients on antiviral therapy for approximately 6 years and found an HBsAg clearance rate of 4.58%. This study found no significant difference in the clearance rate between HBeAg-positive and HBeAg-negative patients, but the rate in patients with cirrhosis was significantly lower than patients without cirrhosis . These results suggested that the clearance rate of non-cirrhosis patients was higher after NA treatment, which is not consistent with the results of patients who experienced spontaneous clearance. Compared to patients with normal baseline ALT, patients with higher ALT levels had significantly higher rates of achieving HBsAg clearance. In general, the clearance rate may increase with the extension of treatment in CHB patients, but the overall rate with currently available NA treatment is low. The HBsAg clearance rates were 1.45.1% after an average follow-up of 27 years after NA treatment .
You May Like: Hepatitis C Symptoms In Child