C183malignant Neoplasm Of Hepatic Flexure
Rare males and females disease from the section . Causes not a significant loss of workdays. Not mortally.
4 959 906 people were diagnosed with Malignant neoplasm of hepatic flexure
1 355 103 died with a diagnosis of Malignant neoplasm of hepatic flexure
0.27 % disease mortality Malignant neoplasm of hepatic flexure
Stage Iv And Recurrent Colon Cancer Treatment
Stage IV colon cancer denotes distant metastatic disease. Treatment of recurrent colon cancer depends on the sites of recurrent disease demonstrable by physical examination and/or radiographic studies. In addition to standard radiographic procedures, radioimmunoscintography may add clinical information that may affect management. Such approaches have not led to improvements in long-term outcome measures such as survival.
Treatment Options for Stage IV and Recurrent Colon Cancer
Treatment options for stage IV and recurrent colon cancer include the following:
Also Check: Can You Donate Blood If You Had Hepatitis A
Staging Of Colorectal Cancer And Survival
|
Cancer has metastasized to liver, bone or lung. |
Information from Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, Mulrow CD, et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology 1997 112:594642 , and Bresalier RS, Kim YS. Malignant neoplasms of the large intestine In: Feldman M, Sleisenger MH, Scharschmidt BF, eds. Sleisinger & Fordtranâs Gastrointestinal and liver disease pathophysiology, diagnosis, management. 6th ed. Philadelphia: Saunders, 1998.
On occasion, Roman numerals I through IV are used in colorectal cancer staging. These numerals correspond with Dukes classes A through D.
The TNM staging system is more detailed than the Dukes system. This system is most useful for surgical purposes, such as providing guidelines on the extent of resection. The Dukes system and corresponding TNM classifications are presented in Table 3.6
T = tumor N = node M = metastasis TIS = carcinoma in situ T1 = tumor invades submucosa T2 = tumor invades muscularis propria T3 = tumor invades through muscularis propria T4 = tumor invades serosa, nodes and adjacent organs N0 = negative lymph nodes at surgery N1 = one to three positive nodes N2 = more than three positive nodes N3 = positive nodes on vascular trunk M0 = no distant metastases M1 = distant metastases.
*On occasion, colorectal cancer is staged using roman numerals I through IV, which correspond with Dukes stages A through D.
Read Also: Hepatitis A Ab Total Reactive
Malignant Neoplasm Of Hepatic Flexure
- 2016201720182019202020212022Billable/Specific Code
- C18.3 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM C18.3 became effective on October 1, 2021.
- This is the American ICD-10-CM version of C18.3 other international versions of ICD-10 C18.3 may differ.
- Applicable To annotations, or
Availability Of Data And Materials

The data supporting the results of this study are available in the SEER 18 regions database , and can be obtained from the corresponding authors on reasonable request. We firstly logged in to the SEER*Stat software with a username of 13521-Nov2019, submitted a data retrieval request, and then we extracted the eligible data after the authorization of the SEER database.
Read Also: Just Food For Dogs Hepatic Support
What Do Colon Polyps Look Like
Most polyps are protrusions from the lining of the intestine:
- Polypoid polyps look like a mushroom, but flop around inside the intestine because they are attached to the lining of the colon by a thin stalk.
- Sessile polyps do not have a stalk, and are attached to the lining by a broad base.
- Flat polyps are the least common type of colon polyp, and are flat or even slightly depressed. These may be difficult to identify because they are not as prominent as polypoid or sessile polyps with the commonly available methods of diagnosing polyps.
Not all colon polyps are the same. There are different histologic types, that is, the cells that make up the polyp have different characteristics when viewed under the microscope. They also vary in size, number, and location. Most importantly, they vary in their tendency to become cancerous .
Adenomatous polyps
The most common type of polyp is the adenoma or adenomatous polyp. It is an important type of polyp not only because it is the most common, but because it is the most common cause of colon cancer.
Most adenomatous polyps are considered sporadic, that is, they do not stem from a recognized genetic mutation that is present at birth . Nevertheless, the risk of having colon polyps greater than one centimeter in size or developing colon cancer is two-fold greater if a first-degree relative has colon polyps greater than one centimeter in size. Therefore, there is likely to be a genetic factor working even in sporadic adenomatous polyps.
Prevention And Screening Methods
For at least two decades, preemptive removal of colon polyps has been the standard approach to cancer prevention. Aggressive screening and polypectomy can reduce the rate of colon cancer development by approximately 80 percent.6
Screening methods for colorectal cancer are discussed in the following sections and compared in Table 4.6
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
Don’t Miss: How Much Cost Hepatitis C Treatment
What Is A Tubular Adenoma
An adenoma is a type of polyp, or a small cluster of cells that forms on the lining of your colon.
When doctors look at an adenoma under a microscope, they can see small differences between it and your colons normal lining. Adenomas typically grow very slowly and look like a small mushroom with a stalk.
Tubular adenomas are the most common type. Theyre considered benign, or noncancerous. But sometimes cancer can develop in an adenoma if it isnt removed. If adenomas become cancerous, theyre referred to as adenocarcinomas.
Less than 10 percent of all adenomas will turn into cancer, but more than 95 percent of colon cancers develop from adenomas.
Read on to learn more about how doctors treat tubular adenomas.
There are two types of adenomas: tubular and villous. These are categorized by their growth patterns.
Sometimes doctors refer to polyps as being tubulovillous adenomas because they have features of both types.
Most small adenomas are tubular, while larger ones are typically villous. An adenoma is considered small when its less than 1/2 inch in size.
Villous adenomas are more likely to turn cancerous.
There are several other types of polyps, including:
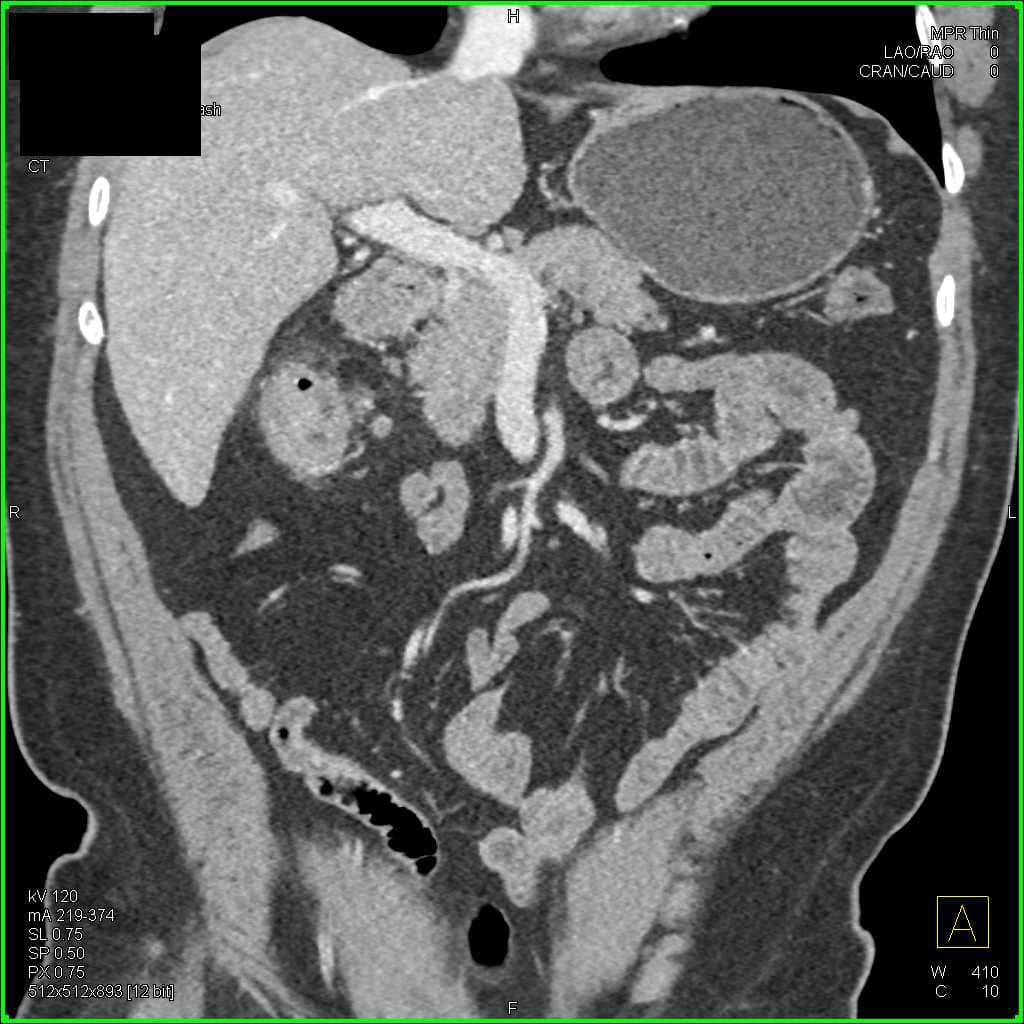
An Abnormality At The Hepatic Flexure
A 92 year old woman presented to the emergency department after collapsing at home. She recalled standing from her chair, feeling lightheaded, and then collapsing. She had felt generally weak for more than a year, with weight loss of 56 lb but no change in bowel habit, dysphagia, or gastrointestinal bleeding. Her medical history included hypertension, hypothyroidism, and anaemia . Among other drugs, she was taking lisinopril, bendroflumethiazide, and levothyroxine. Her son had died at 60 years of age from large bowel obstruction and perforation secondary to colon cancer.
On examination she appeared cachectic with evidence of conjunctival pallor. Her blood pressure was 117/54 mm Hg when lying and 52/31 mm Hg when standing. No masses were palpable on abdominal examination.
Fig 1 Axial computed tomogram of the abdomen
Recommended Reading: Hepatitis B And Ivf Treatment
Update On Colorectal Cancer
DAVID R. RUDY, M.D., M.P.H., and MICHAEL J. ZDON, M.D., Finch University of Health Sciences/Chicago Medical School, North Chicago, Illinois
Am Fam Physician. 2000 Mar 15 61:1759-1770.
See related patient information handout on screening for colorectal cancer, prepared by Courtenay Brooks, a Georgetown medical editing clerk.
An estimated 129,400 new cases of colorectal cancer occurred in the United States during 1999. The lifetime risk of developing this cancer is 2.5 to 5 percent in the general population but two to three times higher in persons who have a first-degree relative with colon cancer or an adenomatous polyp. Between 70 and 90 percent of colorectal cancers arise from adenomatous polyps, whereas only 10 to 30 percent arise from sessile adenomas. Tumors or polyps that develop proximal to the splenic flexure carry a poorer prognosis than those that arise more distally, in part because of delayed diagnosis secondary to later development of symptoms. The Dukes system is the classic staging method for colorectal cancer the TNM staging system is more detailed and therefore more useful for surgical purposes. Although screening guidelines vary, most agree that colorectal cancer screening should begin at 50 years of age in patients without a personal or family history of colorectal cancer.
Colorectal Polyps And Cancer
Studies estimate that colorectal polyps and cancer account for roughly 20% of lower GI bleeds, slightly more if postpolypectomy bleeds are included as well. Colorectal polyps or cancer usually do not cause severe hematochezia, but rather, occult GI bleeding or intermittent mild hematochezia. Patients with colorectal cancer may have other associated signs and symptoms, including weight loss, constipation, or change in bowel habits. Bleeding results from erosions and ulcerations that develop from the friable mucosa. Although polyps may be removed endoscopically, treatment of colorectal cancer usually requires surgery.
Postpolypectomy bleeding may occur up to one week after the procedure, and is treated endoscopically.
In , 2008
You May Like: How To Manage Hepatitis C
Diagnosis Of Sessile Polyps
A doctor can perform a colonoscopy to identify polyps in the colon. During this procedure, the doctor will observe the large intestine and part of the small intestine through a colonoscope.
The colonoscope, which is effectively a camera on a tube that provides images of the walls of the colon, allows the doctor to see whether there are polyps present. The flatter the sessile polyps are, the harder they are to identify.
The doctor may also carry out a biopsy, which involves taking tissue from the polyps to determine their type and whether they are likely to develop into cancer.
Sessile polyps may not always require treatment. If a doctor identifies them to be harmless, they may decide to leave the polyps but monitor them on a regular basis.
People with a history of polyps have a higher chance of developing more in the future, increasing their risk of developing cancerous polyps. Therefore, a doctor may schedule more frequent checkups with these individuals.
If polyps are cancerous or have the potential to become so, the doctor is likely to recommend removing them. If the polyps are in an accessible position, the doctor may be able to extract them at the time of the colonoscopy using a procedure called a polypectomy.
During a colon polypectomy, the doctor can use different surgical techniques to remove polyps. Some options include cold forceps polypectomy, hot forceps polypectomy, and snare polypectomy.
What Is Hepatic Flexure
The hepatic flexure, also known as the right colic flexure, is found in the digestive system of the human body and creates the bend in the colon that connects the ascending colon and the transverse colon. The name of this structure is influenced by its proximity to the liver the word hepatic comes from hpar, which means âliverâ in Greek. A flexure is a bend or a fold.
The ascending colon lies on one side of the hepatic flexure, near the right portion of the liver and the gallbladder. The ascending colon begins at the cecum, a pouch found on the colon, also known as the large intestine. From the cecum, it travels throughout the right side of the abdomen, eventually connecting to the part of the large intestine known as the transverse colon.
The transverse portion of the colon is the longest section of the large intestine. This is also the colon segment that is capable of the most movement. It crosses the abdomen, traveling to the left side and ending near the spleen. The transverse colon also attaches to the border of the pancreas.
Recommended Reading: How Is Hepatitis C Transmitted Cdc
Read Also: How Often Do You Need Hepatitis B Shots
What Is A Polyp In The Colon
A polyp is a projection of tissue from the inner lining of the colon into the lumen of the colon. Different types of polyps look different under the microscope. Polyps are benign growths, but cancer can start in some types of polyps. These polyps can be thought of as pre-cancers, which is why it is important to have them removed.
Cellular Classification Of Colon Cancer
Histologic types of colon cancer include the following:
- Adenocarcinoma .
References
You May Like: Hepatitis C What Is It
Recommended Reading: Can You Donate Blood If You Have Hepatitis C
What Are Juvenile Polyps
Juvenile polyps are cystic dilations of glandular structures within the lamina propria and occur in the colon and rectum of infants, children, and adolescents. The cause of these polyps is unclear. They may represent a response to inflammation. Juvenile polyps are the most common cause of GI bleeding in children or may serve as lead points for intussusception. They should be left alone unless they cause trouble, at which point endoscopic polypectomy is usually sufficient treatment.
Colon Polyp Growth Patterns
Doctors examine removed polyps under a microscope for a close-up look at their cells. The review is to determine levels of dysplasia, a term used to describe how cancerous polyps appear on a cellular level.
Polyps with signs of high-grade dysplasia have disorganized cells with a larger, darker center. These dysplastic cells often grow wildly, a sign that cancer may have been close to forming in the polyp.
Your healthcare provider may recommend a follow-up colonoscopy sooner than normal if they find polyps with high-grade dysplasia. Its a finding that warrants increased attention, notes Dr. Gunter.
Polyps with cells that look only mildly abnormal are labeled as having low-grade dysplasia and are of less concern.
Don’t Miss: How Long Can Hepatitis C Go Undetected
Polyps And Colorectal Cancer
Between 70 and 90 percent of colorectal cancers arise from adenomatous polyps, and 10 to 30 percent arise from sessile adenomas. The larger the polyp, the greater the potential for malignancy. Diminutive polyps have a negligible malignant potential. Polyps with a diameter of 5 to 10 mm are considered small, whereas polyps greater than 10 mm in diameter are considered large. Polyps larger than 2 cm in diameter have a 50 percent chance of becoming malignant over time.6
Polyps may be hyperplastic or adenomatous. From 15 to 30 percent of persons in the U.S. population ultimately develop polyps. About 15 percent of these polyps are hyperplastic and have no malignant potential. Hyperplastic polyps are usually diminutive or small and cannot be identified without biopsy and histologic examination.6
Among adenomatous polyps, those with a tubular histologic pattern are the least likely to become malignant .10 They are also the most common adenomatous polyps . Adenomatous polyps with this pattern have the highest potential for malignancy. Tubulovillous polyps constitute 12 percent of adenomatous polyps and have an intermediate malignant potential.6,10
*The overall weighted malignant potential for adenomatous polyps is 10.5 percent.
Sessile adenomas occur particularly in patients with hereditary nonpolyposis colon cancer. These adenomas account for 20 to 25 percent of the 2.5 to 5 percent lifetime risk of colorectal cancer.12
Read Also: How Much Cost Hepatitis C Treatment
What Happens At The Hepatic Flexure Of The Colon
4/5intestineintestinecoloncolonright colic flexurecolonflexureanswered comprehensively
The right colic flexure or hepatic flexure is the sharp bend between the ascending colon and the transverse colon. The hepatic flexure lies in the right upper quadrant of the human abdomen. It receives blood supply from the superior mesenteric artery.
what does the splenic flexure do? The right colic or hepatic flexure separates the ascending and transverse colon, and the left colic or splenic flexure separates the transverse and descending colon. In dogs and cats, the large intestine contributes 20% to 25% of the total intestinal length.
People also ask, what is the role of the ascending colon?
The role of the ascending colon is to absorb the remaining water and other key nutrients from the indigestible material, solidifying it to form stool. The descending colon stores feces that will eventually be emptied into the rectum.
Is the hepatic flexure part of the large intestine?
The large intestine includes the cecum, colon, and rectum. Upon entering the colon, the food residue first travels up the ascending colon on the right side of the abdomen. At the inferior surface of the liver, the colon bends to form the right colic flexure and becomes the transverse colon.
Also Check: What Are The First Symptoms Of Hepatitis C
Read Also: Hepatitis C Symptoms And Treatment
Familial Adenomatous Polyposis: Genetic Basis
FAP is a cancer predisposition syndrome characterized by numerous adenomatous colorectal polyps, with virtually universal progression to colorectal carcinoma at an early age. It accounts for less than 1% of all colorectal carcinoma cases in the United States and affects 1 in 800010,000 individuals. The majority of cases of FAP are caused by germline mutations in the APC gene on chromosome 5q, and in its inherited form, FAP is transmitted in an autosomal dominant fashion, although up to a third of cases may present as de novo germline mutations.