Tests To Diagnose Hepatitis C
How is Hepatitis C diagnosed?
There are two main blood tests typically used to diagnose Hepatitis C. First, youll have a screening test that shows if youve ever had Hepatitis C at some point in your life. If this test is positive, youll have a second test to see if you have Hepatitis C now. These blood tests are described below:
Hepatitis C antibody test
This is the screening test used by doctors to show whether or not you have ever been exposed to Hepatitis C at some time in your life, by detecting antibodies in your blood. Antibodies are substances your body makes to fight off all kinds of infections. If you were ever infected with Hepatitis C, your body would have made antibodies to fight the virus.
If the test result is:
- Negative, it means you have not been exposed to Hepatitis C and further testing is usually not needed.
- Positive, you have had Hepatitis C at some point. However, it does not tell you whether you have it now. Youll need to see your doctor for another test the Hepatitis C RNA test to determine if the virus is still active and present in your blood.
Hepatitis C RNA Qualitative Test
This test will determine whether or not you are currently infected with Hepatitis C. It is often called the PCR test because of the process used . It looks for the genetic material of the Hepatitis C virus in your blood.
If the test result is:
Hepatitis C RNA Quantitative Test
Spread Of Hepatitis C
Hepatitis C is spread through blood-to-blood contact when blood from a person with hepatitis C enters another persons bloodstream.
The most common way people become infected with hepatitis C in Australia is by sharing injecting equipment such as needles, syringes, spoons and tourniquets. It is possible to be infected with hepatitis C after only one risk event.
Hepatitis C may also be spread through:
- tattooing and body piercing with equipment that has not been properly cleaned, disinfected or sterilised such as backyard tattoos’. Registered parlours with appropriate infection control procedures are not a risk
- needlestick injuries in a healthcare setting
- receiving blood transfusions in Australia prior to 1990 before hepatitis C virus testing of blood donations was introduced
- medical procedures, blood transfusions or blood products and mass immunisation programs provided in a country other than Australia
- pregnancy or childbirth there is a 5% chance of a mother with chronic hepatitis C infection passing on the virus to her baby during pregnancy or childbirth.
Breastfeeding is safe, however if nipples are cracked or bleeding cease breastfeeding until they have healed.
Less likely possible routes of transmission of hepatitis C include:
Hepatitis C cannot be transmitted by:
- kissing
- sharing food, cups or cutlery
- shaking hands or day-to-day physical contact.
Can You Prevent Hepatitis C Infection
Thereâs no vaccine to prevent hepatitis C. To avoid getting the virus:
- Use a latex condom every time you have sex.
- Don’t share personal items like razors.
- Don’t share needles, syringes, or other equipment when injecting drugs.
- Be careful if you get a tattoo, body piercing, or manicure. The equipment may have someone else’s blood on it.
Find out more on how to prevent hepatitis C.
Recommended Reading: Can You Catch Hepatitis C From Kissing
What Type Of Doctor Treats Hepatitis C
Hepatitis C is treated by either a gastroenterologist, a hepatologist , or an infectious disease specialist. The treatment team may include more than one specialist, depending on the extent of liver damage.Surgeons who specialize in surgery of the liver, including liver transplantation, are part of the medical team and should see patients with advanced disease early, before the patient needs a liver transplant. They may be able to identify issues that need to be addressed before surgery can be considered. Other persons who can be helpful in managing patients include dietitians to consult on nutritional issues and pharmacists to assist with management of drugs.
Who Is More Likely To Get Hepatitis C
People more likely to get hepatitis C are those who
- have injected drugs
- had a blood transfusion or organ transplant before July 1992
- have hemophilia and received clotting factor before 1987
- have been on kidney dialysis
- have been in contact with blood or infected needles at work
- have had tattoos or body piercings
- have worked or lived in a prison
- were born to a mother with hepatitis C
- are infected with HIV
- have had more than one sex partner in the last 6 months or have a history of sexually transmitted disease
- are men who have or had sex with men
In the United States, injecting drugs is the most common way that people get hepatitis C.13
You May Like: Interpretation Of Hepatitis A Serologic Test Results
Getting Tested Is The Only Way To Know If You Have Hepatitis C
A blood test called a hepatitis C antibody test can tell if you have been infected with the hepatitis C viruseither recently or in the past. If you have a positive antibody test, another blood test is needed to tell if you are still infected or if you were infected in the past and cleared the virus on your own.
- Are 18 years of age and older
- Are pregnant
- Currently inject drugs
- Have ever injected drugs, even if it was just once or many years ago
- Have HIV
- Have abnormal liver tests or liver disease
- Are on hemodialysis
What Are The Treatments For Hepatitis C
Treatment for hepatitis C is with antiviral medicines. They can cure the disease in most cases.
If you have acute hepatitis C, your health care provider may wait to see if your infection becomes chronic before starting treatment.
If your hepatitis C causes cirrhosis, you should see a doctor who specializes in liver diseases. Treatments for health problems related to cirrhosis include medicines, surgery, and other medical procedures. If your hepatitis C leads to liver failure or liver cancer, you may need a liver transplant.
You May Like: How To Get Checked For Hepatitis
How Can You Get Hepatitis C
Hepatitis C is a blood-borne disease. The main source of infection is from blood from an infected person.
- Most cases are caused by using contaminated needles or injecting equipment to inject drugs . Even a tiny amount of an infected person’s blood left on a needle is enough to cause spread to others.
- Some people who received blood transfusions or blood prior to 1991 were infected with hepatitis C from some donor blood. Since 1991 all blood and blood products donated in the UK are screened for HCV.
- There is also a risk of contracting hepatitis C from needlestick accidents, or other injuries involving blood spillage from infected people.
- There is a small risk of contracting the virus from sharing toothbrushes, razors and other such items which may be contaminated with infected blood.
- There is even a small risk from inhaling drugs like cocaine, as these can make the inside of your nose bleed. If that happens, tiny spots of blood can fall on to the note you are using and, if that is used by someone else, your blood can travel up their nose and into their bloodstream.
- There is also a small risk from re-used equipment used for tattooing, body piercing, acupuncture, etc.
- There is a small risk that an infected mother can pass on the infection to her baby.
- There is a small risk that an infected person can pass on the virus whilst having sex.
The virus is not passed on during normal social contact, such as holding hands, hugging, or sharing cups or crockery.
Hepatitis C: Diagnosis And Treatment
THAD WILKINS, MD JENNIFER K. MALCOLM, DO DIMPLE RAINA, MD and ROBERT R. SCHADE, MD, Medical College of Georgia, Augusta, Georgia.
Am Fam Physician. 2010 Jun 1 81:1351-1357.
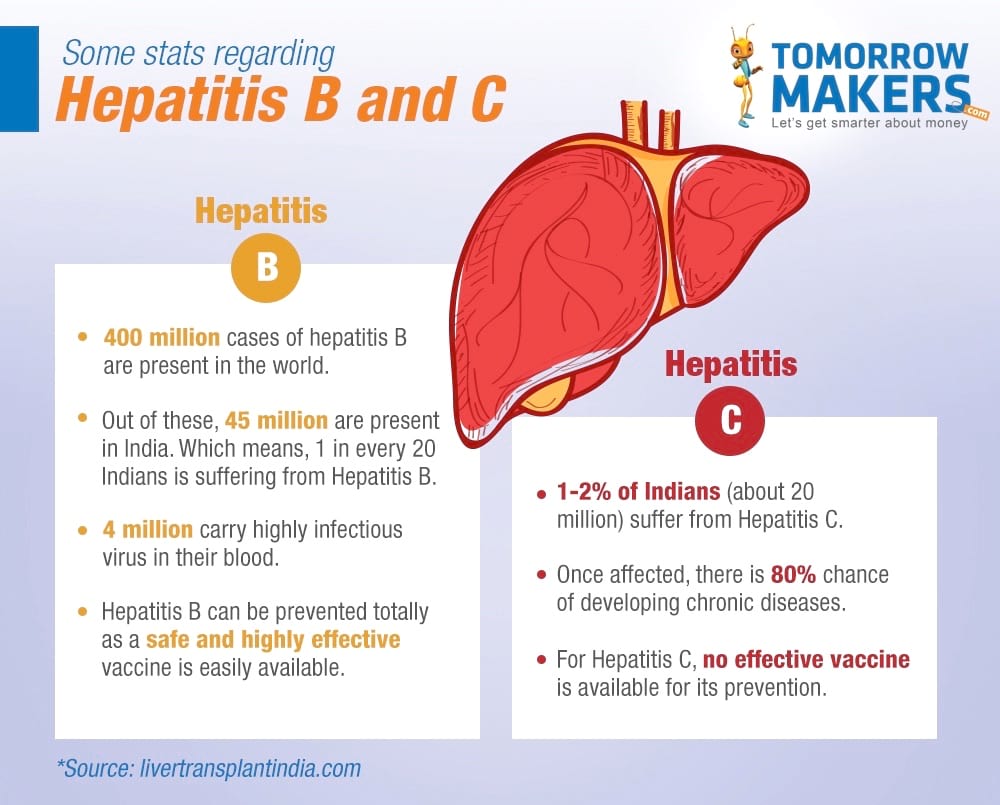
An estimated 170 million persons, or 3 percent of the worlds population, are chronically infected with the hepatitis C virus .1 In the United States, the prevalence of hepatitis C antibody is 2 percent in adults 20 years and older, but the prevalence is higher in groups at increased risk .2,3 HCV, a single-stranded RNA virus, is transmitted through percutaneous exposure to infected blood.4 HCV is categorized into nine genetically distinct genotypes.5 In the United States, 72 percent of patients with HCV infection have genotype 1 16 to 19 percent have genotype 2 8 to 10 percent have genotype 3 and 1 to 2 percent have other genotypes.6 This article focuses on chronic HCV infection in adults and excludes special groups, such as children, pregnant women, transplant recipients, and persons coinfected with hepatitis B virus or human immunodeficiency virus .
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Persons who are not at increased risk should not be screened for HCV infection.
HCV = hepatitis C virus.
*Recommendation for treatment is C because the outcome is a surrogate marker rather than mortality.
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Persons who are not at increased risk should not be screened for HCV infection.
HCV = hepatitis C virus.
Recommended Reading: How Can Get Hepatitis B
Who Should Get Tested
You should consider getting tested for hepatitis C if you’re worried you could have been infected or you fall into one of the groups at an increased risk of being infected.
- Hepatitis C often has no symptoms, so you may still be infected if you feel healthy.
- The following groups of people are at an increased risk of hepatitis C:
- ex-drug users and current drug users, particularly users of injected drugs
- people who received blood transfusions before September 1991
- recipients of organ or tissue transplants before 1992
- people who have lived or had medical treatment in an area where hepatitis C is common high risk areas include North Africa, the Middle East and Central and East Asia
- babies and children whose mothers have hepatitis C
- anyone accidentally exposed to the virus, such as health workers
- people who have received a tattoo or piercing where equipment may not have been properly sterilised
- sexual partners of people with hepatitis C
If you continue to engage in high-risk activities, such as injecting drugs frequently, regular testing may be recommended. Your doctor will be able to advise you about this.
What Is The Impact Of Hepatitis C
- 58 million people have hepatitis C
- 75% of people with hepatitis C live in low- and middle-income countries
- About 50% of all people with hepatitis C live in 4 countries: China, Pakistan, India, and Egypt
- 75% are unaware they are infected
- only 13% have had access to treatment
- 2.3 million people have both HIV and hepatitis C
- 1530% of those chronically infected develop cirrhosis of the liver within 20 years
- 800 people die every day
Hepatitis C is found throughout the world. There are six different major strains of hepatitis C, known as genotypes, distributed across different regions, with genotype 1 being most prevalent in high-income countries and genotype 3 most prevalent in low- and middle-income countries. Genotype 3 accounts for 30% of global hepatitis C infection.
Also Check: Is Hepatitis C An Std
How Should I Take Care Of Myself If I Have Hepatitis C
Good health habits are essential for those who have hepatitis C. You should especially avoid alcohol and medicines and drugs that can put stress on the liver. You should eat a healthy diet and start exercising regularly. Your family doctor can help you plan a diet that is healthy and practical.
Talk to your doctor about any medicines that you are taking, including over-the-counter medicine. Many medicines, including acetaminophen , are broken down by the liver. Because of this, they may increase the speed of liver damage. You should also limit alcohol use. It speeds the progression of liver diseases like hepatitis C. An occasional alcoholic drink may be okay, but check with your doctor first.
Complications Of Hepatitis C
If the infection is left untreated for many years, some people with hepatitis C will develop scarring of the liver .
Over time, this can cause the liver to stop working properly.
In severe cases, life-threatening problems, such as liver failure, where the liver loses most or all of its functions, or liver cancer, can eventually develop.
Treating hepatitis C as early as possible can help reduce the risk of these problems happening.
Also Check: What Are The Early Symptoms Of Hepatitis C
Read Also: How Does Hepatitis C Affect The Liver
Hepatitis C Symptoms : Diagnosis Treatment & Cure
Hepatitis C if not treated will cause irreversible damage to the liver.
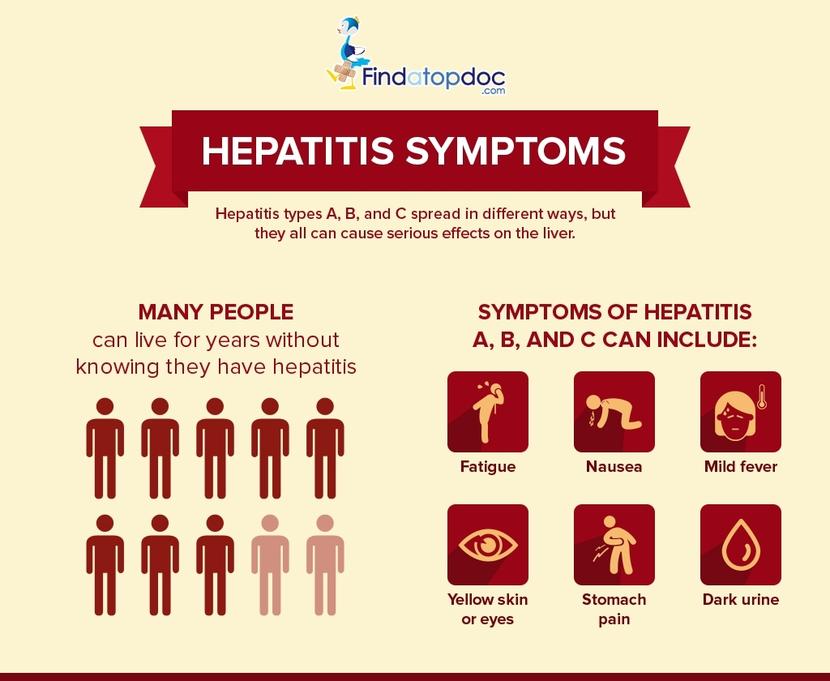
Most hepatitis C patients, about 70% to 80% do not show any signs or symptoms from a hepatitis C virus infection.
Lets go ahead and take a look at some of the hepatitis C symptoms and the diagnosis, treatment and cure options are.
Take time to learn about Hepatitis C Factshere.
However, they usually develop mild and flu like symptoms within 2 weeks to 6 months after being infected. It ranges from person to person. It can sometimes even vary by race, ethnicity and gender.
Contents
Additional Tests You Might Need
Once youve been diagnosed with Hepatitis C, your doctor will likely order a number of tests to find out about the health of your liver and decide on a treatment plan thats most appropriate for you.
Hepatitis C genotype
The Hepatitis C genotype refers to a specific strain or type of the Hepatitis C virus. There are six major types of Hepatitis C around the world: genotypes 1, 2, 3, 4, 5 and 6. In the United States, genotypes 1, 2, and 3 are common:
- Genotype 1: Most Americans with Hepatitis C have this type
- Genotype 2: About 10% of Americans with Hepatitis C have this type
- Genotype 3: About 6% of Americans with Hepatitis C have this type
The genotype of Hepatitis C does not change over time, so you only need to get tested once.
Genotype tests are done before a person starts treatment. Hepatitis C treatment works differently for different genotypes, so knowing your genotype helps your doctor choose the best treatment for you.
Testing for Hepatitis A and Hepatitis B
Your doctor may test to see if your body is immune to Hepatitis A and Hepatitis B. If these tests show no prior exposure or protection, he or she will recommend that you be vaccinated against these two viruses to eliminate the chance of becoming infected.
Liver function tests or liver enzymes
- ALT
- AST
Liver function tests also include ALP and total bilirubin, among other things.
Tests to measure liver scarring or fibrosis
- Liver Biopsy
- Elastography
- Serum markers
Imaging tests
Also Check: Hepatitis C Can You Get Rid Of It
What Is Hepatitis C Infection How Many People Are Infected
Hepatitis C virus infection is an infection of the liver caused by the hepatitis C virus . It is difficult for the human immune system to eliminate hepatitis C from the body, and infection with hepatitis C usually becomes chronic. Over decades, chronic infection with hepatitis C damages the liver and can cause liver failure. In the U.S., the CDC has estimated that approximately 41,200 new cases of hepatitis C occurred in 2016. When the virus first enters the body there usually are no symptoms, so this number is an estimate. About 75%-85% of newly infected people become chronically infected. In the U.S., more than 2 million people are estimated to be chronically infected with hepatitis C. Infection is most commonly detected among people who are 40 to 60 years of age, reflecting the high rates of infection in the 1970s and 1980s. There are 8,000 to 10,000 deaths each year in the U.S. related to hepatitis C infection. HCV infection is the leading cause of liver transplantation in the U.S. and is a risk factor for liver cancer. In 2016, 18,153 death certificates listed HCV as a contributing cause of death this is believed to be an underestimate.
Those who have cirrhosis from HCV also have a yearly risk of liver cancer of about 1%-5%.
Symptoms Of Hepatitis C
The problem with hep C is that most people will live with the virus without showing any signs. Not only does this place them at risk of not getting treatment, but during this time, they can also spread the virus without knowing. However, after someone gets infected with HCV, usually two weeks to 6 months after the virus enters the bloodstream, theyll experience some symptoms that last for 2 to 12 weeks. The most common symptoms include:
- Clay-colored poop
- Weight loss
- Fluid buildup in the abdominal cavity or legs
Many people eventually develop chronic liver disease, ranging from mild to severe, including cirrhosis and liver cancer. Chronic liver disease in people with hepatitis C usually happens slowly, without any signs or symptoms, over several decades. However, for alcohol abusers, this can happen sooner.
Also Check: What Is Hepatitis B Vaccine For
You May Like: What Kind Of Doctor Treats Hepatitis C
North America And Western Europe
The most common malignant tumors in the liver represent metastases from tumors which originate elsewhere in the body. Among cancers that originate from liver tissue, HCC is the most common primary liver cancer. In the United States, the US surveillance, epidemiology, and end results database program, shows that HCC accounts for 65% of all cases of liver cancers. As screening programs are in place for high-risk persons with chronic liver disease, HCC is often discovered much earlier in Western countries than in developing regions such as sub-Saharan Africa.
Acute and chronic hepatic porphyrias and tyrosinemia type I are risk factors for hepatocellular carcinoma. The diagnosis of an acute hepatic porphyria should be sought in patients with HCC without typical risk factors of hepatitis B or C, alcoholic liver cirrhosis, or hemochromatosis. Both active and latent genetic carriers of acute hepatic porphyriasare at risk for this cancer, although latent genetic carriers have developed the cancer at a later age than those with classic symptoms. Patients with acute hepatic porphyrias should be monitored for HCC.
The incidence of HCC is relatively lower in the Western Hemisphere than in Eastern Asia. However, despite the statistics being low, the diagnosis of HCC has increased since the 1980s and it is continuing to increase, making it one of the rising causes of death due to cancer. The common risk factor for HCC is hepatitis C, along with other health issues.