Healthy Tips For Living With Hepatitis C
The Mayo Clinic has identified some lifestyle changes you can make to help improve your health during your treatment for hepatitis C. They suggest that you:
- Be careful with your medications. Some drugs, even those prescribed by your doctor, may have the side effect of causing liver damage. This is a bigger risk for people with hepatitis C. Talk to your doctor about whether you should avoid certain prescription or over-the-counter drugs.
- Avoid alcohol. Drinking alcoholic beverages can make liver disease progress more quickly. Therefore, its best to avoid alcohol if you have hepatitis C.
Medical Treatment For Hepatitis A B & C
Treatment for hepatitis A, B, or C is based on which type of hepatitis is present in the bloodstream and the severity of the resulting liver damage. Depending on the results of diagnostic tests, our specialists at NYU Langone may recommend antiviral medication to stop the virus from replicating and protect your liver from further damage.
Who Is Most At Risk Of Contracting Hepatitis C
You have a high risk of contracting hepatitis C if you:
- use or have used injection drugs even if it was just once or many years ago
- have received blood or blood products or an organ transplant before July 1990 in Canada
- have been in jail or
- have been injected or scratched during vaccination, surgery, blood transfusion or a religious/ceremonial ritual in regions where hepatitis C is common.
You have a high moderate risk of contracting hepatitis C if you:
- have tattoos or body piercing
- have multiple sexual partners
- have a sexually transmitted infection , including HIV or lymphogranuloma venereum
- have experienced traumatic sex or rough sex or have used sex toys or fisting that can tear body tissue
- have vaginal sex during menstruation
- have received a kidney treatment
- have received an accidental injury from a needle or syringe
- have another infectious disease
- were born to a hepatitis C infected mother or
- have a sexual partner infected with hepatitis C.
Hepatitis C is NOT passed from person to person by:
- coughing, sneezing
- breastfeeding unless your nipples are cracked and bleeding or
- oral sex, unless blood is present.
Don’t Miss: How Can Someone Get Hepatitis
What Are The Side Effects Of Treatment
Some people stop therapy because of side effects. Since hepatitis C can lead to liver damage, cirrhosis, and liver cancer if not treated, its vital to stick with a treatment plan.
Newer drugs have fewer severe side effects than pegylated interferon and ribavirin. Nevertheless, you may feel some effects while taking hepatitis C medication. Side effects can include:
- nausea, vomiting, or diarrhea
- appetite loss or weight loss
Serious side effects can occur with pegylated interferon and ribavirin treatment. If youre taking these medications, you should be monitored for these serious side effects:
- anemia
- thrombocytopenia
- light sensitivity in the eyes
- trouble breathing because of lung tissue inflammation
- suicidal thoughts, depression, or irritability
- thyroid disease
- elevated liver enzymes
- autoimmune disease flares
Some medications arent recommended if theres evidence of liver damage, like cirrhosis . A co-infection with HIV also affects medication options.
C Data Abstraction And Data Management
The following data will be extracted from included trials: study design, setting, population characteristics , eligibility and exclusion criteria, hepatitis C treatments and comparisons, the method of outcome ascertainment if available and results for each outcome. An investigator will extract study data and a second investigator will review extractions. Intention-to-treat results will be recorded if available.
Also Check: Hepatitis C Treatment Guidelines 2017
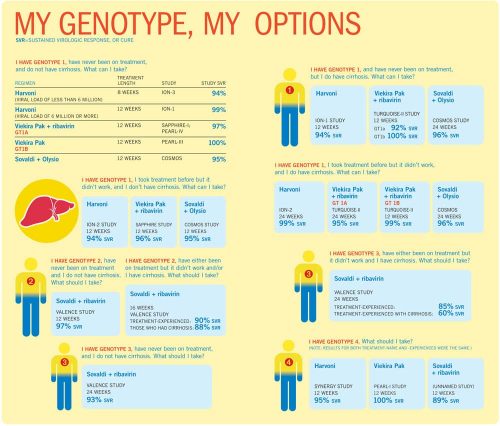
Initial Treatment Of Adults With Hcv Infection
Initial treatment of HCV infection includes patients with chronic hepatitis C who have not been previously treated with interferon, peginterferon, ribavirin, or any HCV direct-acting antiviral agent, whether investigational, or US Food and Drug Administration approved.
Simplification of the treatment regimen may expand the number of healthcare professionals who prescribe antiviral therapy and increase the number of persons treated. This would align with the National Academies of Science, Engineering, and Medicine strategy to reduce cases of chronic HCV infection by 90% by 2030 .
Recommended and alternative regimens are listed in order of level of evidence. When several regimens are at the same recommendation level, they are listed in alphabetical order. Regimen choice should be determined based on patient-specific data, including drug-drug interactions. Patients receiving antiviral therapy require careful pretreatment assessment for comorbidities that may influence treatment response or regimen selection. All patients should have access to an HCV care provider during treatment, although preset clinic visits and/or blood tests depend on the treatment regimen and may not be required for all regimens/patients. Patients receiving ribavirin require additional monitoring for anemia during treatment .
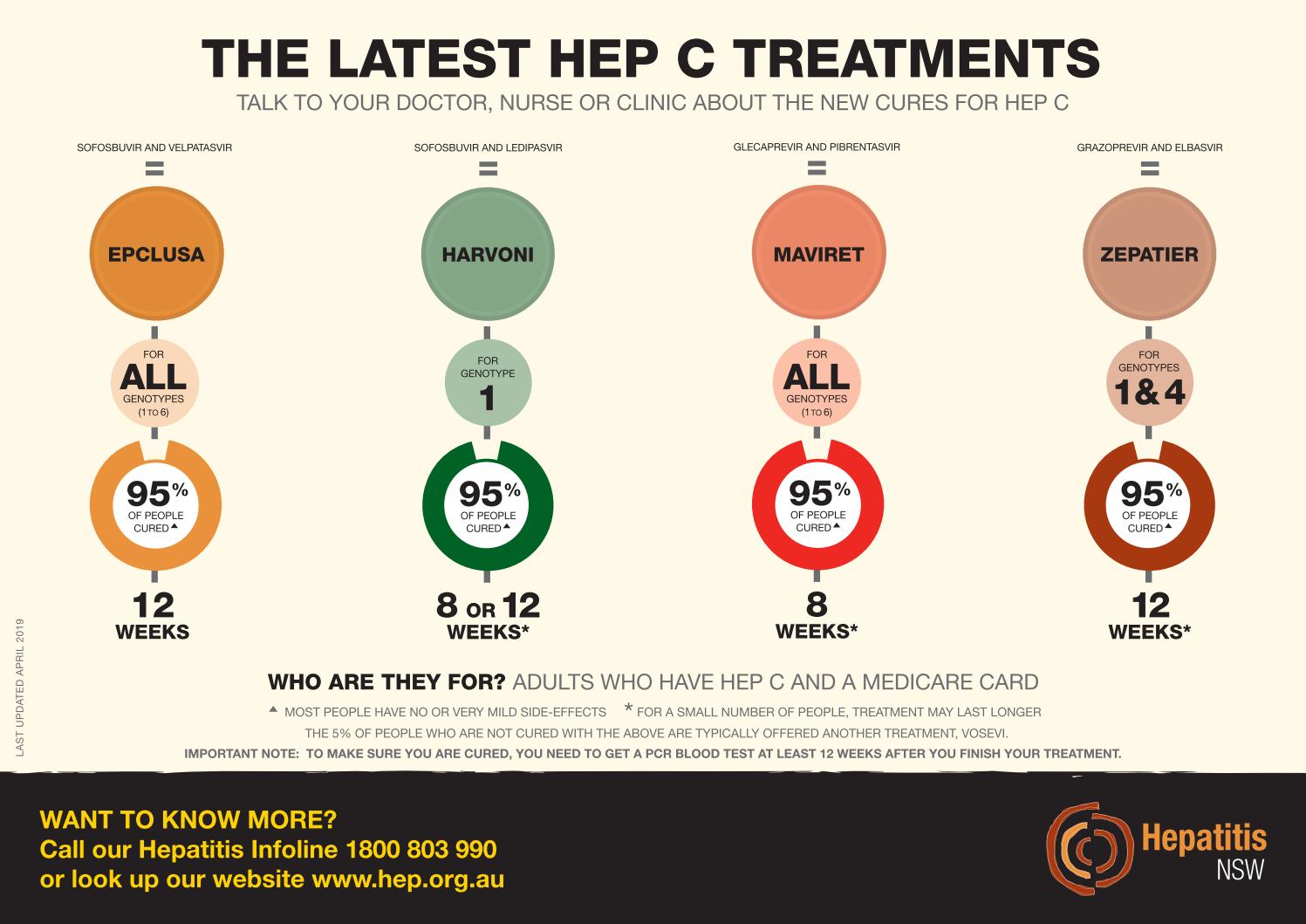
What Is Hepatitis C
Hepatitis C is a contagious, blood-borne virus that causes liver inflammation and kills liver cells, permanently damaging the liver. Hepatitis C infections are more common than you think and can have devastating impacts for individuals in their later years of life. The current treatment options have demonstrated a 95% cure rate.
You May Like: Hepatitis B And C Can Be Spread By
When To Get Help For Hepatitis C
It is very common to become infected with hepatitis C but not have symptoms. If you do have symptoms, they will appear within 6 to 12 weeks after you are exposed to the virus. Symptoms may include the following:
- Abdominal pain
- Jaundice
- Loss of appetite
- Nausea or vomiting
The longer hepatitis C goes untreated, the more damage it causes to your liver. Eventually, it may lead to liver cancer or liver failure. Speak with your primary care doctor about being tested if you believe you have been exposed to hepatitis C or if you are in one of these high-risk groups:
- Your mother had hepatitis C at the time you were born
- You’ve had contact with blood or needles at work
- You’ve had more than one sex partner in the last 6 months
- You are a man who has had sex with another man
- You have a history of sexually transmitted disease
- You are on kidney dialysis
- You are HIV positive
- You have injected illegal drugs or have shared needles
- You have tattoos or body piercings
- You work or live in a prison
- You had a blood transfusion or organ transplant before July 1992
- You have hemophilia and received clotting factor before 1987
- You are an adult age 45 to 65
Nonstructural 5a Complex Inhibitors
The NS5A complex plays a role in HCV RNA replication regulation as well as viral assembly and packaging, and directly interacts with the RNA-dependent RNA polymerase . The exact antiviral action of NS5A inhibitors is unknown they are theorized to inhibit hyperphosphorylation of the NS5A protein and alter the proteins location from the endoplasmic reticulum, likely causing faulty HCV assembly. Ledipasvir, ombitasvir, daclatasvir , elbasvir, velpatasvir, odalasvir, samatasvir, ravidasvir, ruzasvir, and pibrentasvir currently make up the class of NS5A inhibitors . Ledipasvir is one of the most potent inhibitors of the NS5A complex, but may have lower activity in HCV genotypes 2 and 3 infections.,, Ombitasvir is approved in combination with paritaprevir, ritonavir, and dasabuvir as part of the 3D regimen for the treatment of HCV genotypes 1 and 4 infections, but also has a higher pill burden, which could affect compliance. Velpatasvir has antiviral activity against HCV replicons in genotypes 1 through 6. NS5A complex inhibitors have high potency, multigenotypic coverage, and generally a low barrier to resistance. Newer agents in this class have the promise to increase the resistance threshold.
Don’t Miss: How Long Does It Take To Cure Hepatitis C
Are There Ways To Cure Hepatitis C Other Than With Medications
Patients sometimes ask whether there are ways to treat hepatitis C other than taking medicines. Currently, there are no vaccines to prevent hepatitis C. Once a person is infected, the only way to treat it is with prescribed antiviral medications.
Some patients worry that having hepatitis C means they will need a liver transplant. Only a very small fraction of people with hepatitis C require a liver transplant. By far, most people with hepatitis C never need a liver transplant. A transplant is performedonlywhen damage to the liver is extremely advanced and the liver is unable to perform its basic functions. A transplant provides a new working liver, but a transplant does not get rid of the hepatitis C virus in the patient. Patients with a liver transplant still need antiviral medication to cure their virus.
Sustained Viral Response: A Patient
The molecular demonstration of the absence of HCV-RNA twelve weeks after the end of a course of antiviral treatment confirms the sustained eradication of the virus. The likelihood of a late recurrence is well under 1% , and most such events are actually not recurrences but reinfections . The eradication of HCV does not generate protective immunity .
A meta-analysis of 129 studies involving a total of 34 563 patients who had undergone interferon-based treatment revealed that a sustained virological response was associated with a 62% to 84% reduction of mortality, a 68% to 79% reduction of the risk of hepatocellular carcinoma , and a 90% reduction of the risk of needing liver transplantation . As interferon-based treatment was contraindicated in patients with decompensated cirrhosis, these data are uninformative with respect to any potential clinical benefit, for these patients, of sustained viral eradication with direct antiviral agents . Initial studies have yielded clinical and laboratory evidence of improvement mainly for patients with a MELD score below 1618 points . In large-scale cohort studies, sustained viral eradication was associated both with lower liver-associated mortality and with substantially lower extrahepatic mortality . Sustained viral eradication eliminates the risk of individual transmission and is associated with a better quality of life .
HCV genotypes
Don’t Miss: How Do Contract Hepatitis C
Ifn Monotherapy In Acute Hepatitis C
Although the short courses of standard IFN monotherapy introduced in the 1980s by Hoofnagle et al, Davis et al, and Di Bisceglie et al led to sustained improvement in liver disease and loss of virus in less than 10% of patients, these therapies were the first to cure chronic viral hepatitis.
Jaeckel et al reported that treatment with IFN alfa-2b prevented chronic infection in 98% of a group of 44 German patients with acute hepatitis C. In this study, patients received 5 million U/day of IFN alfa-2b subcutaneously for 4 weeks and then three times per week for another 20 weeks the IFN alfa-2b was well tolerated in all patients but one.
Because it has the poorest safety profile of all the HCV antiviral agents, with few exceptions PEG-IFN is no longer recommended in combination regimens. Spontaneous resolution of acute HCV infection may occur in 15% to 50% of patients. Monitoring for spontaneous clearance for a minimum of 6 months before initiating any treatment is therefore recommended.
References
World Health Organization. Hepatitis C: fact sheet. Available at . Updated: October 2017 Accessed: January 23, 2018.
Frank C, Mohamed MK, Strickland GT, et al. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet. 2000 Mar 11. 355:887-91. .
Kim A. Hepatitis C virus. Ann Intern Med. 2016 Sep 6. 165 :ITC33-ITC48. .
What About Patients With Hepatitis C Who Also Have Hepatitis B
Hepatitis B virus can flare in patients who are co-infected with hepatitis B and hepatitis C and are taking medication for hepatitis C. This has been reported as a potential risk for patients who are taking hepatitis C treatment and have underlying hepatitis B as well. The flare usually occurs within a few weeks after the patient starts taking medication for hepatitis C. Therefore, patients who have both hepatitis B and hepatitis C should be seen by a hepatitis expertbeforestarting treatment of the hepatitis C they may need to start taking hepatitis B treatment to avoid a hepatitis B flare.
Read Also: Liver Disease Caused By Hepatitis C
Treatment For Acute And Chronic Hepatitis C Infection
Some people are diagnosed with hepatitis C when the infection is in the acute phase . About one in four people will clear the hepatitis C virus from their body on their own within six months. When a person is diagnosed with hepatitis C in the acute phase, a healthcare provider might recommend waiting to see if their body clears the virus on its own.
Current treatment guidelines in Canada focus on treatment for chronic hepatitis C infection . The treatment guidelines recommend that treatment of acute hepatitis C infection be assessed on an individualized basis. In many cases, a person has to progress to chronic hepatitis C infection before they can receive public or private drug coverage for hepatitis C treatments.
You May Like: Royal Canin Feline Hepatic Diet
What Are The Symptoms Of Hepatitis C
During the acute phase most persons have no symptoms or might experience a mild illness. Symptoms of acute HCV infection, when present, may include:
- Jaundice
- Dark-colored urine, light-colored stools
- Diarrhea
- Fever
During the chronic phase hepatitis C usually progresses silently, with no symptoms at all during the first 10-20 years. Signs of severe liver scarring may include:
- Ascites
- Star-shaped vein pattern developing on the swollen belly
- Jaundice
- Itching
- Easy bruising and bleeding
Because symptoms of hepatitis C are usually absent, persons with risk for HCV infection should be tested. The blood test for hepatitis C infection is called the hepatitis C antibody test. People who have hepatitis C infection will show positive antibodies on this test. In many cases, it is necessary to confirm a positive hepatitis C antibody test with a more specific test, such as a test for HCV virus RNA.
If you think you have hepatitis C or have risk for hepatitis C, you should contact your doctor. The Communicable Disease Control Unit may be able to help answer your questions.
You May Like: Drinking Alcohol With Hepatitis C
Antiviral Treatment In Pregnancy
The risk of vertical transmission in mothers with an HCV monoinfection is 5% and is not diminished by cesarean section . Mothers are not advised against breastfeeding either. Vertically acquired hepatitis C takes a mild course in childhood, with very slow progression of hepatic fibrosis . Antiviral treatment during pregnancy cannot be recommended, as there are insufficient data on the potential teratogenicity of DAAs.
Pregnancy And Hepatitis C
The new hepatitis C medicines have not been tested in pregnancy.
You should not become pregnant while taking treatment as it could be harmful to unborn babies.
If you’re pregnant, you must delay treatment until after your baby is born.
Speak to your doctor before starting hepatitis C treatment if you’re planning to become pregnant in the near future.
You’ll need to wait several weeks after treatment has ended before trying to get pregnant.
Women taking ribavirin should use contraception during treatment and for another 4 months after the end of treatment.
Men taking ribavirin should use a condom during treatment and for another 7 months after the end of treatment. This is because semen can contain ribavirin.
If you become pregnant during treatment, speak to your doctor as soon as possible to discuss your treatment options.
Also Check: What Are The Symptoms To Hepatitis C
Limitations Of Drug Treatments
Though the latest generation of hepatitis C drugs can effectively cure the disease, patients whose hepatitis C infection has progressed to the point of causing advanced cirrhosis or liver failure may require a liver transplant to fully recover.
Its important to let your doctor know what other medications and supplements youre taking so you can avoid harmful interactions. If youre nursing or pregnant, youll also want to let your healthcare provider know, as this can affect your treatment options.
How Do You Treat Hepatitis C
Treatment for hep C has come a long way. Patients used to require weekly interferon injections that required a course of six months to a year. Now, meds are in the form of a tablet thats taken over just a few weeks. Better yet, 80% of patients taking hep C meds report no side effects. Those who do experience them say theyre extremely mild and can be managed with OTC medications.
The beauty of todays treatments is that they can cure even chronic hep C cases that have been around for decades. Though these meds can eliminate the virus from a patients system, they cant cure damage already done to the liver or reverse liver cancerthose more serious complications will often require a separate course of treatment.
Recommended Reading: Hepatitis A Vaccine Cost Cvs
Hepatitis C Virus Epidemiology
The World Health Organization estimates that there are 130 to 150 million cases of HCV infection worldwide, totaling 3% of the worlds population, with an average of 3 to 4 million new infections occurring each year. HCV infection causes substantial morbidity, ranging from cirrhosis to hepatocellular carcinoma , liver failure, and death. HCV infection and HCC were the leading indications for liver transplantation in the United States in 2014 however, the spectrum for transplantation is expected to shift as more patients with HCV infection are identified and successfully treated. According to estimates in 2013, 3.2 million Americans have chronic HCV infection, yet only 50% of patients infected with HCV know of their viral status of those, 7% to 11% are treated, and 5% to 6% have successful clearance of the virus. Furthermore, it is predicted that the burden of cirrhosis due to HCV infection could reach 37.2% by 2020 in infected patients.
In order to identify patients infected with HCV, recommendations have been made for routine testing in people born between 1945 and 1965 in people who have injected illegal drugs, received blood transfusion or organ transplantation prior to July 1992, or received clotting factor concentrates before 1987 in patients on long-term dialysis in children born to HCV-positive mothers in health care workers who have been exposed to HCV infection and in patients with evidence of chronic liver disease.