What Is The Treatment For Autoimmune Hepatitis
Treatment is almost always needed. Early treatment can improve symptoms, reduce the risk of complications, and also greatly improve your outlook . Treatment aims to reduce inflammation and suppress the immune system with immunosuppressant medicines:
- Steroid medication is the usual first treatment. Steroids are good at reducing inflammation. A high dose is usually needed at first. The dose is then gradually reduced over a few weeks. The aim is to find the lowest dose needed to control the inflammation. The dose needed varies from person to person. See the separate leaflet called Oral Steroids for more detail.
- Azathioprine is an immunosuppressant medicine that works in a different way to steroids. It is usually used in addition to the steroid. A steroid plus azathioprine tends to work better than either alone. Also, the dose of steroid needed is usually less if you also take azathioprine. This means that any side-effects from steroids may be less severe.
Treatment works well in most cases. Usually, the inflammation settles and symptoms improve within a few months of starting treatment. However, it may take a year or more to get the disease totally under control. Azathioprine is usually taken for at least two years.
For some people a liver transplant may be an option – for example:
- In the few people who do not respond to treatment with the medicines mentioned above or
- In people diagnosed in the late stage of the disease with severe ‘scarring’ of the liver or liver failure.
Autoimmune Liver Diseases Occur When The Bodys Immune System Attacks The Liver Causing Inflammation If Left Untreated The Liver Inflammation May Eventually Cause Cirrhosis Of The Liver Which May Lead To Liver Cancer And Liver Failure
Overview and Symptoms
Although a number of autoimmune conditions may involve the liver, the three most common autoimmune liver diseases are autoimmune hepatitis, primary biliary cholangitis and primary sclerosing cholangitis. These conditions may occur individually or as part of overlap syndromes.
How Is Autoimmune Hepatitis Treated
Treatment works best when autoimmune hepatitis is found early. The goal of treatment is to control the disease and to reduce or get rid of any symptoms .
To do this, medicines are used to help slow down or suppress your overactive immune system. They also stop your body from attacking your liver.
Once you have started treatment, it can take 6 months to a few years for the disease to go into remission. Some people can stop taking medicine, but often the disease comes back. You may need treatment now and then for the rest of your life. Some people need to remain on treatment if they have relapsed many times or if their disease is severe.
In some cases autoimmune hepatitis may go away without taking any medicines. But for most people, autoimmune hepatitis is a chronic disease.
It can lead to scarring of the liver . The liver can become so badly damaged that it no longer works. This is called liver failure.
If you have liver failure, a liver transplant may be needed.
Be sure to ask your healthcare provider about recommended vaccines. These include vaccines for viruses that can cause liver disease.
Don’t Miss: What Is Hepatic Metastatic Disease
When To See A Healthcare Provider
If you develop any of the symptoms of chronic hepatitis, liver damage, or liver cancer, see your healthcare provider. It takes only a blood test to detect the presence of a hepatitis virus in your body .
A blood test also can determine which hepatitis virus you’re infected with, which will determine what your treatment should be .
What Type Of Blood Tests Are Used To Diagnose Autoimmune Diseases
Several different blood tests may be used to diagnose an autoimmune disease. In addition to a regular complete blood count and metabolic panel, other tests that are likely to be included are anti-dsDNA, anti-RNP, anti-Sm, anti-Sjogren’s SSA and SSB, anti-scleroderma, anti-Jo-1, anti-CCP, antibody against cardiolipin, and an antinuclear antibody test. A rheumatoid factor test, which looks for rheumatoid arthritis, is also usually included during the diagnostic phase. The antinuclear antibody test looks for antibodies that could cause an autoimmune response.
Don’t Miss: What Does Non Reactive Hepatitis B Mean
What Is Autoimmune Hepatitis
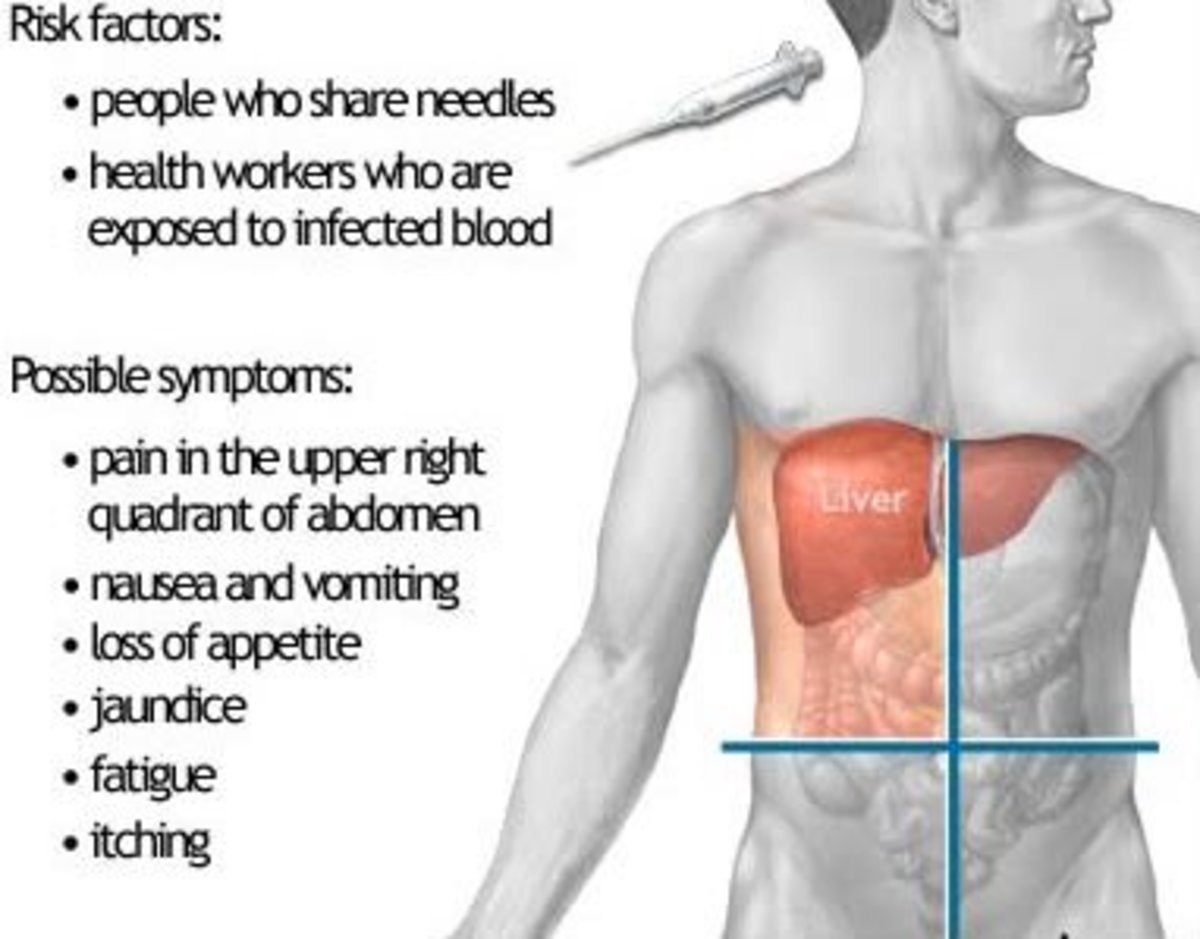
The liver is a large organ that sits up under your ribs on the right side of your belly . It helps filter waste from your body, makes bile to help digest food, and stores sugar that your body uses for energy. Autoimmune hepatitis occurs when your bodys infection-fighting system attacks your liver cells. This causes swelling, inflammation and liver damage.
It is a long-term or chronic inflammatory liver disease.
Autoimmune hepatitis:
- May occur at any age
- Affects women more than men
- Is often linked to other diseases where the body attacks itself
What To Expect From Your Doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may reserve time to go over any points you want to spend more time on. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous, or occasional?
- How severe are your symptoms?
- Does anything seem to improve or worsen your symptoms?
- Are you taking any medicines or treatments for your symptoms?
- Do you have a family history of liver disease?
© 1998-2019 Mayo Foundation for Medical Education and Research . All rights reserved.Terms of use.
Don’t Miss: What Is Hepatitis B Core Antibody
Drug Induced Liver Injury
Drug induced liver injury represents the most challenging differential diagnosis, not only because it can mimic the clinical, biochemical, serological and morphological phenotype of AIH , but also because drugs may trigger latent or induce a de novo AIH . The distinction between DILI and AIH by histology can be extremely difficult , due to the absence of histological features pathognomonic of either DILI or AIH. Severe portal plasma cell-rich inflammation, prominent intralobular plasmacells and eosinophils, rosette formation, absence of cholestasis and presence of fibrosis have been suggested as features that are in favor of the diagnosis of AIH . The absence of cirrhosis, or advanced fibrosis, at presentation mainly suggests AIH-like DILI. A detailed clinical information is crucial, and the patients history should focus on recent exposure to drugs that can induce AIH-DILI. Fortunately, AIH-DILI usually responds to high doses of steroids as severe AIH usually does, but differently from true AIH that always relapses, steroid treatment can be discontinued without a DILI relapse .
Do Patients Recover From Autoimmune Hepatitis Treatment
Autoimmune hepatitis is a chronic condition, and while it can be managed, it usually cannot be cured. It is possible to achieve remission from autoimmune hepatitis with the use of steroids. However, most individuals will require treatment for the rest of their lives. The 10-year survival rate for people being treated for autoimmune hepatitis is between 83.8%94%. Without treatment, the survival rate falls to 50%60%.
Recommended Reading: Chronic Hepatitis B Virus Infection
What Causes Autoimmune Hepatitis In Children
It is not known exactly why the immune system begins attacking liver cells in children with autoimmune hepatitis.
Experts are looking at a number of possible causes, including:
- Genetics. Physical traits passed down from parents
- Environment. Causes of disease from outside the body, such as toxic substances, certain medicines, or germs
- Problems with the immune system. For example, in patients with autoimmune hepatitis, it seems that some cells that regulate the immune system are fewer or weaker, while other cells that make the immune system attack are more frequent or more active.
Inside the Liver Center: Meet Dr. Weymann
Dr. Weymann leads a team of highly skilled specialists dedicated to caring for children suffering from a wide range of liver diseases. Named to the Best Doctors in America list, Dr. Weymann understands that liver problems can be life-threatening and life-changing. Quick evaluation, correct diagnosis and early treatment can impact long-term health.
What Do Researchers Know About What Causes Autoimmune Hepatitis
Autoimmune hepatitis is believed to be caused by a combination of genetic and environmental factors. The condition can be triggered by an environmental factor when you are already genetically predisposed to it. The genes HLA DRB1*03 and HLA DRB1*04 have both been linked to an increased risk of autoimmune hepatitis. Autoimmune hepatitis can also be triggered by certain medications or other diseases.
Recommended Reading: Hepatitis C Antigens And Antibodies
What Is The Right Therapy For A Patient With Autoimmune Hepatitis
AIH can be treated very effectively with immunosuppressive agents. The gold standard is the treatment with prednisone alone or in combination with azathioprine.
The indication for starting an immunosuppressive treatment has to be evaluated, and the treatment strategy must be adjusted to the patients individual risk for developing adverse events of either corticosteroids or azathioprine. For instance, in obese patients, patients with osteoporosis, or patients with brittle diabetes, the steroid dose should be as low as possible, whereas in patients with cytopenia, azathioprine should be avoided .
Patients with refractory disease and burned out cirrhosis may be candidates for liver transplantation. Alternative immunosuppressive agents are not well established in AIH, but the promising agents with the most empiric use are mycophenolate mofetil and cyclosporine.
Indications for treatment of AIH
Absolute indication for starting an immunosuppressive treatment in patients with AIH include the following:
-
An elevation of ALT > 10 fold ULN
-
A more than 5-fold ULN elevated ALT in conjunction with a more than twofold-elevated gamma globulin
-
Bridging necrosis or multiacinar necrosis in the histological picture
-
Cases of severe and intolerable symptoms
Patients with absolute indications for treatment have a poor prognosis without immunosuppressive therapy.
Relative indication for starting an immunosuppressive treatment include the following:
Instrtion
What Are The Risk Factors For Autoimmune Hepatitis

Several factors seem to increase the risk of developing autoimmune hepatitis. You may be at a slightly higher risk if you are a girl or young woman, if you have a relative with any autoimmune disorder, or if you already have an autoimmune disorder. Not all people with risk factors will get autoimmune hepatitis. Risk factors for autoimmune hepatitis can include:
-
Family history of an autoimmune disorder
-
Female sex
Your risk of autoimmune hepatitis is also increased if you have another autoimmune disease including:
-
Graves disease
-
Hashimotos thyroiditis
-
Sjogrens syndrome
-
Systemic lupus erythematosus
-
Type 1
Don’t Miss: Hepatitis E Causes And Treatment
What Is The Outlook
With treatment, most people with autoimmune hepatitis have a normal life expectancy and feel well most of the time. The treatment used for autoimmune hepatitis has improved the outlook tremendously. It is very important that you do not stop your treatment too early without your doctor’s knowledge, as your hepatitis may return. Although the condition usually returns at some point after stopping treatment, it can usually be treated again by quickly going back on medication.
There is a very small increased risk of developing liver cancer, especially if you also have ‘scarring’ of the liver due to your autoimmune hepatitis. Some doctors recommend a blood test and an ultrasound scan of your liver every so often to screen for this.
How Is Autoimmune Hepatitis In Children Diagnosed
Your childs health care provider will do several tests to look for autoimmune hepatitis and other related diseases. These tests may include:
- Blood tests
- Liver biopsy
- Special scans of the liver, such as ultrasound and magnetic resonance cholangiopancreatography
- Exam of the inside of the intestines , under anesthesia
You May Like: How Do You Get Hiv And Hepatitis
Willowbrook State School Experiments
A New York University researcher named Saul Krugman continued this research into the 1950s and 1960s, most infamously with his experiments on mentally disabled children at the Willowbrook State School in New York, a crowded urban facility where hepatitis infections were highly endemic to the student body. Krugman injected students with gamma globulin, a type of antibody. After observing the temporary protection against infection this antibody provided, he then tried injected live hepatitis virus into students. Krugman also controversially took feces from infected students, blended it into milkshakes, and fed it to newly admitted children.
Types Of Autoimmune Hepatitis
There are two types of AIH based on serum tests:
- Type I is more common, tends to affect young women, and is associated with other autoimmune diseases. This is the most common form of AIH in the United States.
- Type II primarily affects girls between the ages of 2 and 14.
While AIH generally occurs in adolescence or early adulthood, it can develop at any age.
Symptoms of AIH range from mild to severe. In the early stages, you may have no symptoms, but in later stages, symptoms can appear suddenly. They may also slowly develop over time.
AIH symptoms include:
Blood tests can also measure the amount of immunoglobulin G antibodies in your blood. IgG antibodies help the body fight infection and inflammation.
A liver biopsy may sometimes be necessary to diagnose AIH. It can reveal the type and severity of your liver damage and inflammation. The procedure involves removing a small piece of your liver tissue with a long needle and sending it to a laboratory for testing.
Treatment can slow down, stop, and sometimes reverse liver damage. Approximately 65 to 80 percent of people with AIH will go into remission. However, remission can take up to three years.
Recommended Reading: Why Are Baby Boomers Being Tested For Hepatitis C
How Is Autoimmune Hepatitis Treated In A Child
Autoimmune hepatitis is a serious, long-lasting disease. Right now, there is no cure for autoimmune hepatitis. Fortunately, most children with autoimmune hepatitis respond well to treatment.
The goal of autoimmune hepatitis treatment is remission. This means symptoms become less severe and liver damage slows or stops. Some children are able to stop taking medicine after two or three years. These children will still need to be watched for a return of autoimmune hepatitis symptoms and other health issues.
Two main types of medicine are used to help control autoimmune hepatitis in children:
- Corticosteroids . Prednisone helps stop the immune system from attacking the liver. It also reduces liver inflammation. Budesonide is another corticosteroid that is sometimes used it has less side effects, but it is mostly given later on when the disease is under control already.
- Immunosuppressants. Azathioprine or mercaptopurine are often added to the treatment they work together with prednisone to get the immune system under control. There are other medications to suppress the immune system that can be used if the standard treatment is not working well.
Treatments For Autoimmune Hepatitis
Treatment works best when AIH is diagnosed early. The goal in treating AIH is to slow or stop the bodys immune system from attacking the liver. The medications used are immunosuppressants, such as prednisone and Imuran® . Physicians usually prescribe a high initial dose of prednisone, and then taper it down progressively as symptoms and liver enzymes improve. Most people will need to take medication for the rest of their lives. Since prednisone can cause a wide range of side effects, Imuran® is often used in conjunction to allow for a lower dose of the prednisone.
Some people may go into remission, during which physicians can effectively discontinue treatment others will relapse after stopping treatment, and will then need to restart the medication and continue on long-term maintenance therapy. A few patients may eventually be tapered off the prednisone completely and stay solely on Imuran®. For those who do not respond to, or relapse from, the combination regimen, then stronger immunosuppressive agents such as mycophenolate mofetil, cyclosporine, or tacrolimus may be considered. When medications do not halt the progress of the disease, or complications from cirrhosis have developed, the remaining option is a liver transplant. Fortunately, the success rate of transplantation in people with AIH is excellent.
Also Check: Hepatitis C Can You Get Rid Of It
Symptoms Of Autoimmune Hepatitis
There are two forms of autoimmune hepatitis: type 1 and type 2. The majority of patients have type 1, which typically begins in adolescence or young adulthood. Almost half of individuals with type 1 disease also have other autoimmune disorders, including:
- Type 1 diabetes
- Ulcerative colitis
- Thyroiditis
Autoimmune hepatitis is a chronic disorder with symptoms that can worsen over time if not treated. Symptoms include:
- Fatigue
- Abdominal pain on the right side of the body where the liver is located
- Jaundice
- Dark urine
Enhancing Healthcare Team Outcomes
This article discusses hepatitis, which is a complex disease and requires an interprofessional approach from healthcare providers to tackle it. The article discusses strategies to prevent hepatitis through patient education and vaccination and the importance of closer monitoring for disease progression and complications. These strategies require significant interprofessional communication and care coordination by physicians, including primary care physicians and specialists, nurses, pharmacists, and other health professionals, to enhance patient-centered care. Nursing needs to work closely with the patient to ensure they understand their disease, are compliant with medications and vaccines, and note progress or lack thereof. Pharmacists are crucial to ensuring the proper medications at the correct dose are in the therapy regimen, and that there are no interactions. Any issues noted by any member of the interprofessional healthcare team need to be shared and charted, so everyone operates from the same data. These measures can help improve the outcomes and aid to patient safety and can also help enhance team performance.
Also Check: How Can Hepatitis C Be Transmitted Sexually
Potential Outcomes Of Immunosuppressant Therapy
The goal of treatment is disease remission. In remission, patients experience the improvement of symptoms, the normalization of abnormal liver chemistries and gamma globulin levels, and the reduction or elimination of inflammatory activity on liver biopsy.
Most patients who embark on a course of immunosuppressant therapy respond well initially. More than 90% of adults started on corticosteroid treatment experience improvements in liver chemistries and gamma globulin levels within 2 weeks.
Remission, if it is to be achieved, typically requires 18-24 months of immunosuppressant therapy. Remission can be achieved in about 65% of patients within 18 months and 80% of patients within 3 years. Once a drug-induced remission is achieved, an attempt should be made to withdraw immunosuppression. However, a sustained remission after total drug withdrawal is seen in 13% of patients at 5 years. Patients who relapse need to restart long-term immunosuppressant therapy in an effort to normalize their biochemical abnormalities and to delay the progression of liver disease. Many such patients are maintained on chronic maintenance therapy with azathioprine.
About 13% of patients experience an incomplete response to treatment, without worsening of their condition. Most incomplete responders need long-term immunosuppression in an attempt to stabilize levels of aspartate transaminase and alanine aminotransferase andby extensionprevent disease progression.
References