Sensitivity Analysis And Test Of Publication Bias
Sensitivity analysis was conducted to assess the consistency of the above results. We compared the use of the random- and fixed-effects models for analysis of the studies and found that there were no obvious differences between them .3). Then, impact analysis was carried out for both the OS and RFS studies, and the results suggested that no single study affected the pooled estimates .
Inherited Diseases And Hcc
Certain metabolic disorders such as hereditary hemochromatosis, 1-antitrypsin deficiency, Wilsons disease, and hepatic porphyria are associated with high risk for the development of HCC. These hereditary diseases are known to promote hepatocarcinogenesis as a result of increased inflammation and hepatocellular damage .
A Tabular Or Chart Listing Of Features And Signs And Symptoms
Symptoms that suggest the development of malignant liver tumors
There are three common presentations. Patients may present with malignant liver tumors found incidentally during investigation for unrelated symptoms or conditions. The most common focal mass in the liver is a hemangioma. This has a typical radiological appearance, so that if the radiologist diagnoses typical hemangioma, no further investigation is required. All other liver masses require aggressive investigation because the earlier a liver malignancy is treated, the better the prognosis. A delay in diagnosis may mean the difference between cure and palliation. A mass in the liver that has declared itself to be malignant by growing under observation without a firm diagnosis being made represents a failure of management.
Patients not known to have liver disease who develop a primary liver cancer may present with ascites, jaundice, or cancer symptoms, such as anorexia, weight loss, and weakness. Sometimes the first presentation is with an intrahepatic or intraperitoneal bleed due to a ruptured hepatocellular carcinoma . This would present as an acute abdomen with pain and hypotension being the major manifestations.
Also Check: Hepatitis B Vaccine Dose For Newborns
Ascites And Spontaneous Bacterial Peritonitis
Portal hypertension results in an increase in hydrostatic pressure within the splanchnic bed. Decreased oncotic pressure caused by decreased protein synthesis may contribute to the condition.
Ascites should be treated with salt restriction and diuretics.8,15 Diuretic regimens typically include a combination of spironolactone and a loop diuretic, unless the serum sodium level is less than 125 mEq per L .8,11 Patients with new-onset ascites should have diagnostic paracentesis performed, consisting of cell count, total protein test, albumin level, and bacterial culture and sensitivity.8,11 Serum-ascites albumin concentration is used to calculate the serum-ascites albumin gradient. If the serum-ascites albumin gradient is 1.1 g per dL or greater, the diagnosis of portal hypertension ascites or heart failureassociated ascites is confirmed. However, a serum-ascites albumin gradient less than 1.1 g per dL is suggestive of another cause of ascites, such as peritoneal carcinomatosis or nephrogenic ascites.
Characteristics Of Included Studies That Expressed Plt As Binary Variable
The baselines of our included studies are summarized in Table . In general, this meta-analysis involved 5545 patients with a mean or median follow-up of 5 to 46 months. The PLT cut-off values ranged from 75 to 150 , which were near the cut-off point for thrombopenia . The qualities of the studies were moderate to high . Four studies were performed in western regions, and the others were conducted in eastern countries. Twenty-one and 9 studies reported HR values for OS and RFS, respectively. Ten studies estimated the influence of PLTs on the prognosis of patients who underwent liver resection, and 5 studies involved patients with RFA.
Don’t Miss: How Do You Acquire Hepatitis C
Search Strategy And Selection Criteria
Two independent investigators performed a systematic search using the PubMed, EmBase, and ISI Web of Science databases with no language restrictions. Our core search consisted of the terms AND combined with the terms . In addition, we contacted authors if full text or crucial data were not available. We retrieved the reference lists from relevant literature reviews and included the articles manually. We used EndNote X7 software to search and manage citations.
Pooled Hr Value For All Studies
After calculating the total effect size using a random-effects model, we found that a low PLT level before treatment indicated a poor prognosis. The forest plot is shown in Figure , and the pooled estimator was stratified by survival . The 21 studies that analyzed OS had a pooled HR value of 1.41 , with a moderate degree of between-study heterogeneity . The pooled HR value for RFS was 1.44 , and this value also showed a moderate degree of heterogeneity .
Effects of platelet count on the survival of all HCC patients.
Don’t Miss: Best Food For Hepatitis C
How Can I Be Sure That The Patient Has Malignant Liver Tumors
What primary malignant liver tumor occurs?
The most common malignant liver tumors that occur in the liver is hepatocellular carcinoma , which accounts for about 85% of all primary hepatic cancers. The next most frequently occurring malignancy is cholangiocarcinoma. This disease accounts for about 10% to 12% of all hepatic malignancies. The remaining liver primaries are rare and include primary lymphoma of the liver, various sarcomas, and tumors of vascular or lymphatic endothelium.
What Is Hepatocellular Carcinoma
Hepatocellular carcinoma is a cancer that starts in your liver. It’s different from “secondary” liver cancers, which have spread to the liver from other organs.
If caught early, it can sometimes be cured with surgery or transplant. In more advanced cases it canât be cured, but treatment and support can help you live longer and better.
It’s important to remember that you still have control over the decisions you make about your treatment and your life. Make sure you have people you can talk to about your plans, your fears, and your feelings. Ask your doctor about support groups, where you can meet people who know what you’re going through.
Your doctor can help you understand your treatment options. Surgery, radiation, chemotherapy, immunotherapy, and target therapy may be some of your choices.
Recommended Reading: What Does Hepatitis B Come From
Risk Factors For Cirrhosis
- Alcoholic liver disease and hepatitis C are the most common causes in developed countries.
- Hepatitis B is the most common cause in parts of Asia and in sub-Saharan Africa.
- There may also be a genetic predisposition to cirrhosis which may explain the variable rates of its development in people with similar risk factors .
- Continued alcohol consumption increases the rate of progression of cirrhosis from any cause.
- Risk factors for the development of cirrhosis in those with chronic hepatitis C infection:
- Regular alcohol consumption.
What Are Other Treatments For Hepatocellular Carcinoma
Other treatments are:
- Ablation therapy. Your healthcare provider uses a special needle to burn your tumors.
- Embolization therapy or chemoembolization therapy. Healthcare providers inject chemotherapy drugs into your livers main artery, which carries the drugs to your tumor. Then they temporarily block your artery so the drugs stay in your tumor longer.
- Targeted therapy. This treatment blocks the growth of cancer cells and limits damage to healthy cells by targeting the cancer cells genes.
Recommended Reading: Hepatitis A Symptoms And Treatment
How Can I Confirm The Diagnosis
Radiological diagnosis
The diagnosis of malignant liver tumors is primarily radiological. Hepatocellular carcinoma is the most common hepatic neoplasm, and the diagnostic algorithm has been designed to diagnose HCC noninvasively if possible.
HCC has typical radiological features. These are hypervascularity in the arterial phase of a contrast-enhanced radiological study , followed by washout or hypovascularity compared to the rest of the liver in the portal venous and/or delayed phases.
If the typical features of HCC are present on either contrast-enhanced CT scan or dynamic MRI, a biopsy is not necessary for the diagnosis. If neither study shows typical features, a biopsy of the liver mass is required. However, if the lesion requires resection, whatever it is, there is no need for a biopsy prior to resection.
Histological diagnosis
Histological diagnosis of large liver lesions is not difficult. If radiology does not confirm the diagnosis, a core biopsy is recommended in most instances, although aspiration biopsies may be sufficient. However, for small lesions, aspiration biopsy is not adequate, and a core biopsy is necessary.
Comparison of a biopsy from the lesion and a biopsy from surrounding normal liver may also help make a diagnosis of HCC. There are intermediate forms between HCC and cholangiocarcinoma, such as cholangiocellular carcinoma, but not much is known about the clinical aspects of these variants.
Alcoholic Fatty Liver Disease
As the name suggests, AFLD is attributed to excessive alcohol consumption that causes hepatic injury by the build-up of fats, inflammation, and scarring leading to HCC, which could be fatal . Globally, the prevalence of AFLD is increasing and has become a significant contributor to the liver disease burden accounting for 30% of HCC related deaths . The safe levels of drinking as defined in the dietary guidelines in the United States is two drinks for men and one drink for women per day as one alcoholic drink accounts for about 14 g of alcohol . By contrast, excessive alcohol consumption is considered to cause AFLD . The threshold level of alcohol intake causing hepatotoxic effect varies and it depends on a variety of factors such as gender, ethnicity, and genetics .
You May Like: How Did I Get Hepatitis C
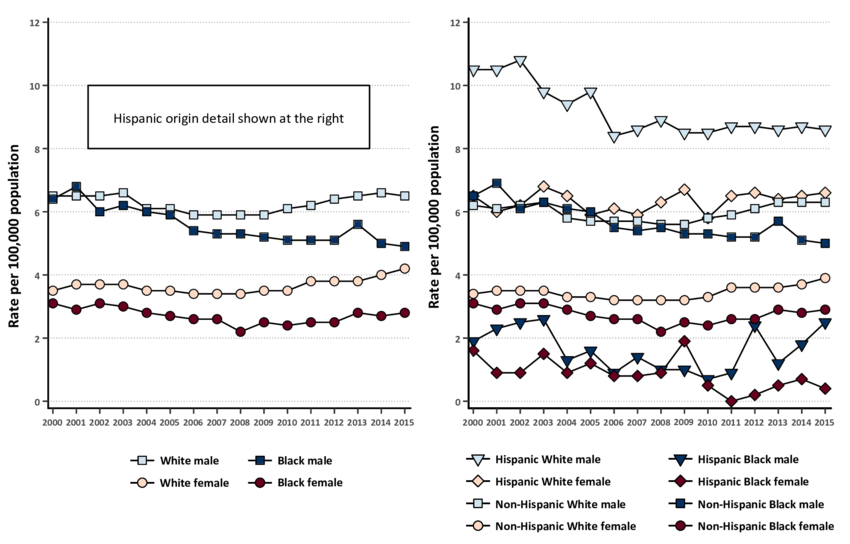
North America And Western Europe
The most common malignant tumors in the liver represent metastases from tumors which originate elsewhere in the body. Among cancers that originate from liver tissue, HCC is the most common primary liver cancer. In the United States, the US surveillance, epidemiology, and end results database program, shows that HCC accounts for 65% of all cases of liver cancers. As screening programs are in place for high-risk persons with chronic liver disease, HCC is often discovered much earlier in Western countries than in developing regions such as sub-Saharan Africa.
Acute and chronic hepatic porphyrias and tyrosinemia type I are risk factors for hepatocellular carcinoma. The diagnosis of an acute hepatic porphyria should be sought in patients with HCC without typical risk factors of hepatitis B or C, alcoholic liver cirrhosis, or hemochromatosis. Both active and latent genetic carriers of acute hepatic porphyriasare at risk for this cancer, although latent genetic carriers have developed the cancer at a later age than those with classic symptoms. Patients with acute hepatic porphyrias should be monitored for HCC.
The incidence of HCC is relatively lower in the Western Hemisphere than in Eastern Asia. However, despite the statistics being low, the diagnosis of HCC has increased since the 1980s and it is continuing to increase, making it one of the rising causes of death due to cancer. The common risk factor for HCC is hepatitis C, along with other health issues.
Management Of Liver Cirrhosis In Patients With Hepatocellular Carcinoma
Bahaa Eldeen Senousy Ismail1, Roniel Cabrera2
1Department of Medicine, 2Section of Hepatobiliary Diseases, University of Florida, Florida, USA
Corresponding to:
Abstract: Management of hepatocellular carcinoma is challenging compared to other common malignancies because of the nature of the associated background of chronic liver dysfunction. Most of the patients with HCC have underlying cirrhosis. While progression of the tumor is a major contributor to mortality, cirrhosis and its complications often accounts for a significant portion of the morbidity and mortality seen in this group of patients. Severity of underlying liver disease and degree of decompensation predicts prognosis and dictates the tumor treatment options and responses. A multidisciplinary approach is considered the standard of care and paramount to optimal patient outcomes. This review provides information on the general management of cirrhosis, cirrhosis-related complications and commonly associated symptoms, mainly focusing when available on high-level evidence and guidelines.
Keywords: Cirrhosis ascites encephalopathy varices peritonitis
Submitted Jul 25, 2013. Accepted for publication Jul 30, 2013.
doi: 10.3978/j.issn.2304-3865.2013.09.03
Also Check: How Is Hepatitis B And C Transmitted
Listing Of Usual Initial Therapeutic Options Including Guidelines For Use Along With Expected Result Of Therapy
Resection for HCC
Patients with Child A cirrhosis and insignificant portal hypertension tolerate resection well. Portal hypertension precluding resection includes a measured portal pressure gradient of more than 10 mmHg, esophageal varices, a platelet count of less than 100,000/mL, and a large spleen on imaging. Resection in these patients is associated with a poor prognosis, frequent post-resection ascites, jaundice, and slow deterioration to death.
The ideal malignant liver tumors for resection are a single lesion in the periphery of the left or right lobe. Unfortunately, few tumors are ideal. The tumor must be removed with at least a 1-cm tumor-free margin. This method usually involves a right or left partial hepatectomy. Occasionally, with poorly situated tumors, a trisegmentectomy can be performed. This method requires excellent liver function. Instead of this, sometimes it is possible to perform a mesohepatectomy: removal of the medial segments of both the right and left lobes. Smaller, well-situated tumors can be removed by a segmentectomy: removal of one or two segments. Laparoscopic hepatectomy is becoming more frequent, with the attendant decrease in post-operative complications.
In the best of hands, the post-operative mortality for hepatectomy even in cirrhosis is less than 1%, as long liver function is preserved and there is no portal hypertension. The long-term survival is about 50% at 5 years. The recurrence rate is 50% to 70% at 5 years.
Downstaging
Aki In Patients With Liver Cirrhosis
Patients with advanced liver cirrhosis are more susceptible to AKI compared to the normal population due to the reduced effective circulating blood volume and mean arterial pressure secondary to splanchnic vasodilation leading to kidney hypoperfusion . Common etiologies in cirrhotic patients are hypovolemia , hepatitis virus-associated glomerulonephritis and hepatorenal syndrome that is a diagnosis of exclusion observed in about 13-25% of patients .
The work-up is guided by the clinical setting, and generally includes ultrasound of the kidneys, urine electrolytes, urine analysis to assess for the presence of hematuria and proteinuria, and appropriate serological testing for antibodies against the glomerular basement membrane and for vasculitis. Occult sepsis should also be evaluated with ascitic fluid analysis for SBP. It should be noted that patients with chronic liver disease have a significantly lower baseline serum creatinine concentration than the general population and a slower rise in serum creatinine with a drop in GFR due to decreased production of creatinine and due to increased volume of distribution given the edema and ascites . Newer methods to assess renal function in cirrosis are being evaluated and includes urinary neutrophil gelatinase-associated lipocalin that was shown not only to accurately assess the degree of renal dysfunction, but also to identify the etiology .
Read Also: Hepatomegaly With Diffuse Hepatic Steatosis
What Other Diseases Conditions Or Complications Should I Look For In Patients With Malignant Liver Tumors
Cholangiocarcinoma
Intrahepatic and extrahepatic cholangiocarcinoma are different diseases, despite similarities in histological appearances. Extrahepatic cholangiocarcinoma is decreasing in incidence, whereas intrahepatic cholangiocarcinoma is increasing in incidence. This section will discuss only intrahepatic cholangiocarcinoma, including hilar carcinoma.
Clinical presentation
This is usually a silent cancer until presentation with either jaundice or cancer symptoms. With todaysâ frequent abdominal imaging for unrelated reasons it is not uncommon for this tumor to be detected incidentally. More often it presents with jaundice, either because of obstruction to the common hepatic ducts, or with an episode of cholangitis, also related to duct obstruction.
Risk factors for HCC are well known, but seldom present. These include infection with liver flukes, Opisthorchis viverini, or Chlornorchis sinensis, Caroliâs disease, or choledochal cyst. Cirrhosis also seems to be a risk factor, although the incidence of CCA in cirrhosis is much lower than for HCC. Most cases of CCA arise in patients with no known risk factors. Another predisposing condition is sclerosing cholangitis.
Serological diagnosis
CA19-9, CA 125, and carcinoembryonic antigen are frequently elevated in CCA but are nonspecific. In the presence of a liver mass, the specificity of CA19-9 is about 80%, but it is less specific in patients with sclerosing cholangitis.
Diagnosis of cholangiocarcinoma
What Is The Right Therapy For The Patient With Malignant Liver Tumors
Management of patients at risk for hepatocellular carcinoma
Patients at risk for HCC should undergo regular screening. The groups of patients at risk include all patients with cirrhosis and certain noncirrhotic patients with chronic hepatitis B. However, being at risk is not by itself sufficient to enter a patient into a screening program. It depends on the magnitude of risk.
Details of at-risk groups in whom the incidence of HCC is high enough to make screening worthwhile are listed in Table I. The recommended screening protocol is performing an ultrasound every 6 months. Alpha-fetoprotein is insufficiently sensitive or specific for routine use as a screening test. Des-gamma-carboxy prothrombin and the L3 fraction of AFP are also not recommended.
| Population group | |
|---|---|
| HBV carrier with family history of HCC | Incidence unknown but higher than without family history |
| Cirrhotic HBV carriers | |
| Incidence unknown but HCC occurs at a younger age | |
| Hepatitis C cirrhosis | |
| Stage 4 primary biliary cirrhosis | 3-8%/yr |
| Unknown, but probably > 1.5%/yr | |
| Alpha 1-antitrypsin deficiency and cirrhosis | Unknown, but probably > 1.5%/yr |
| Other cirrhosis | |
| Unknown, but probably 3-8%/yr |
You May Like: Hepatitis C Is It Curable
Nonalcoholic Fatty Liver Disease And Hepatocellular Carcinoma
Cláudia P. Oliveira
1São Paulo Clínicas Liver Cancer Group, Hospital das Clínicas, Instituto do Câncer do Estado de São Paulo, Department of Gastroenterology, University of São Paulo School of Medicine, Avenida Dr. Enéas de Carvalho Aguiar No. 255, Instituto Central No. 9159, 05403-000 Sao Paulo, SP, Brazil
Academic Editor:
Abstract
Hepatocellular carcinoma incidence is increasing worldwide in recent years. Most HCC cases develop in the presence of advanced chronic liver disease related to chronic hepatitis C virus infection, chronic hepatitis B infection, and alcohol abuse. Approximately 1550% of HCC cases are classified as idiopathic, suggesting that other risk factors are responsible for its rising incidence. Recent studies suggest that nonalcoholic fatty liver disease can be associated with these idiopathic cases. NAFLD progresses slowly and can develop into liver cirrhosis, liver failure, and HCC. In the last few years, NAFLD has received more attention because of its high prevalence worldwide.
1. Introduction
1.1. Retrospective Studies: Hepatocellular Carcinoma Was Associated with Cryptogenic Cirrhosis
1.2. Case Reports of HCC in Cirrhosis Related to NAFLD
| Case number | |
| TAE, resection | NR |
1.3. Prospective Studies of Nonalcoholic Steatohepatitis and HCC
1.4. Metabolic Risk Factors, Hepatocarcinogenesis, and Animal Models in NAFLD
2. Metabolic Syndrome and the Risk of HCC
2.1. Obesity and HCC
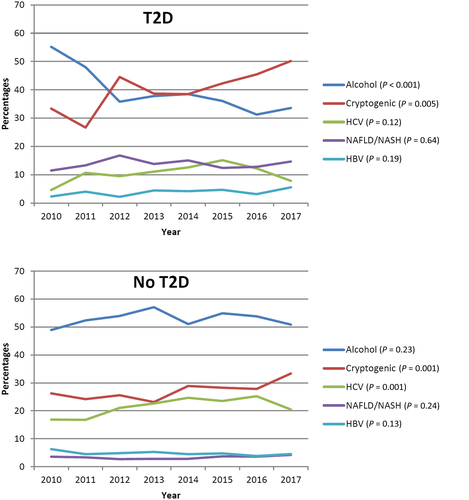
2.2. Diabetes and HCC
3. Hepatocarcinogenesis in NAFLD
Conflict of Interests