Should All Patients With Chronic Hepatitis B Be On Treatment
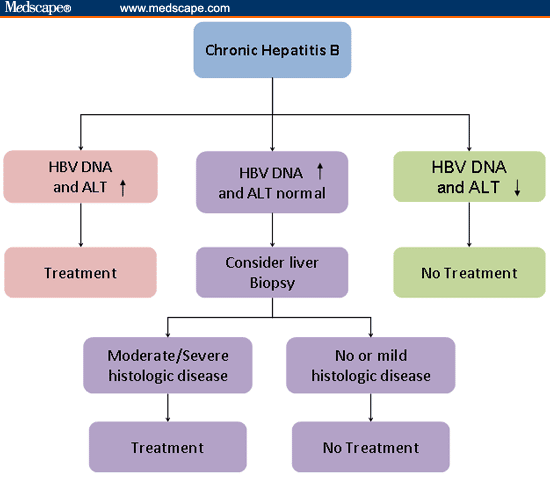
Not all patients with chronic hepatitis B need to be on treatment. The decision to treat HBV is based on several factors including blood tests results, the patient’s age, and the risk of developing cirrhosis or liver cancer. Sometimes a liver biopsy is needed to see if there is significant liver damage to make a decision.
Hepatitis B medications are recommended for patients with detected HBV virus on a blood test and evidence of liver damage. Liver damage can be detected with a liver enzyme known as ALT. People with cirrhosis should be considered for treatment even if the liver enzymes appear normal.
Chronic hepatitis B may change over time. Patients can go through different phases with low amounts of virus and normal level of ALT followed by high viral loads and ALT levels. These bursts of virus activity usually don’t cause any symptoms but may cause liver damage overtime. It is important that people with chronic hepatitis B have blood tests on a regular basis to see if treatment is needed.
There are some medications which can cause hepatitis B “reactivation” which can lead to life threatening liver failure. These medications are used to treat some cancers, inflammatory conditions and hepatitis C. Reactivation reactions can be prevented and it is important to let your provider know you have HBV before you start any new medications.
Hbv Primary Care Workgroup
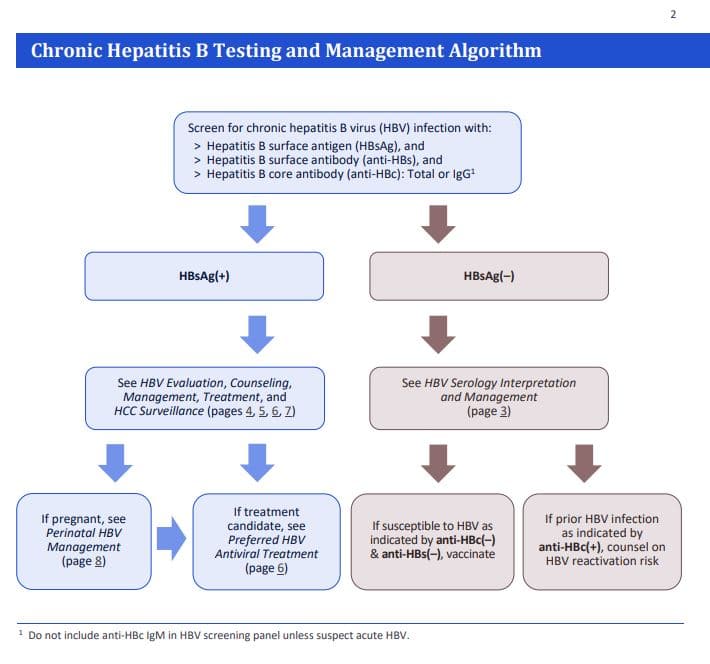
The HBV Primary Care Workgroup includes members in the United States from hepatology, infectious diseases, pharmacy, primary care, and public health. The 2020 HBV Primary Care Workgroup Guidance was first released in early 2020 and is accessible on this web site , with the aim to have regular updated versions posted online. The goal of this document is to provide simplified, up-to-date, and readily accessible HBV management guidance for primary care medical providers. Note, this guidance does not incorporate HBeAg status in the initial decision-making process, but persons positive for HBeAg are recommended to undergo monitoring of HBeAg for evidence of HBeAg seroconversion. The 2020 HBV Primary Care Workgroup Guidance recommends initiating HBV treatment in the following situations.
- : Treatment is recommended but persons should be promptly referred to a hepatologist.
- Cirrhosis: Treatment is recommended for all persons with cirrhosis, regardless of HBV DNA level, ALT level, or HBeAg status.
- Without Cirrhosis: For persons without cirrhosis, treatment is recommended if the HBV DNA level is greater than 2,000 IU/mL and the ALT level is elevated, regardless of HBeAg status. For this purpose, elevated ALT is defined as greater than 25 U/L in females and greater than 35 U/L in males that is persistent for at least 3 to 6 months.
Whats The Prognosis For Hepatitis B
Your doctor will know youâve recovered when you no longer have symptoms and blood tests show:
- Your liver is working normally.
- You have hepatitis B surface antibody.
But some people don’t get rid of the infection. If you have it for more than 6 months, youâre whatâs called a carrier, even if you donât have symptoms. This means you can give the disease to someone else through:
- Unprotected sex
- Contact with your blood or an open sore
- Sharing needles or syringes
Doctors donât know why, but the disease does go away in a small number of carriers. For others, it becomes whatâs known as chronic. That means you have an ongoing liver infection. It can lead to cirrhosis, or hardening of the organ. It scars over and stops working. Some people also get liver cancer.
If youâre a carrier or are infected with hepatitis B, donât donate blood, plasma, body organs, tissue, or sperm. Tell anyone you could infect — whether itâs a sex partner, your doctor, or your dentist — that you have it.
Show Sources
CDC: âHepatitis B Questions and Answers for Health Professionals,â âHepatitis B Questions and Answers for the Public.â
Mayo Clinic: âHepatitis B.â
UpToDate: âHepatitis B virus: Screening and diagnosis.â
CDC.
HealthyPeople.gov: âHepatitis B in Pregnant Women: Screening.â
Annals of Internal Medicine: âScreening for Hepatitis B Virus Infection in Nonpregnant Adolescents and Adults: U.S. Preventive Services Task Force Recommendation Statement.â
Recommended Reading: How Soon Can You Test For Hepatitis C
Is Antiviral Therapy Recommended For Acute Hepatitis B
No. Acute hepatitis B, defined as a positive test for hepatitis B surface antigen and the presence of hepatitis B core antibodyimmunoglobulin M , is a self-limited disease in 90% to 95% of adults and resolves without specific antiviral therapy within 3 to 6 months after the onset of clinical symptoms. For this reason, only supportive care is offered to patients with acute hepatitis B infection. Antiviral therapy is considered only for patients with chronic hepatitis B . For patients with severe acute hepatitis B with evidence of liver dysfunction such as coagulopathy or encephalopathy, antiviral therapy may be considered in this situation, expert consultation is advised.
Prodromos Hytiroglou MD, in, 2018
What Are The Risk Factors For Getting Hepatitis B
Due to the way that hepatitis B spreads, people most at risk for getting infected include:
- Children whose mothers have been infected with hepatitis B.
- Children who have been adopted from countries with high rates of hepatitis B infection.
- People who have unprotected sex and/or have been diagnosed with a sexually transmitted infection.
- People who live with or work in an institutional setting, such as prisons or group homes.
- Healthcare providers and first responders.
- People who share needles or syringes.
- People who live in close quarters with a person with chronic hepatitis B infection.
- People who are on dialysis.
Don’t Miss: Diagnostic Test For Hepatitis B
Medical Treatment Of Acute Hepatitis B Virus Infection
Background
Hepatitis B virus is a virus that affects the liver. It is usually transmitted by injectable drug abuse, transfusion of infected blood, unhygienic tattooing practices, coming into contact with blood infected with HBV, or by unprotected sex. Acute HBV infection is the period that covers the period immediately after HBV infection. Most people are asymptomatic. About 5% to 40% of people with acute HBV develop symptoms such as jaundice , tummy pain, tiredness, nausea, and vomiting. While most people clear the virus after acute HBV infection, the virus remains in others and causes major health problems . Occasionally, people with acute HBV may develop immediate liver failure . The best way to treat acute HBV is not clear. We sought to resolve this issue by performing this review. We included all randomised clinical trials published to August 2016. We included only trials in which participants with acute HBV infection had not undergone liver transplantation previously and did not have liver disease due to other viral infections. Apart from using standard Cochrane methods which allow comparison of only two treatments at a time , we planned to use an advanced method which allows comparison of the many different treatments individually which are compared in the trials . However, because of the nature of the information available, we could not determine whether the network meta-analysis results were reliable. So, we used standard Cochrane methodology.
Study characteristics
Prevention Of Acute Hepatitis B
High-risk behavior, such as sharing needles to inject drugs and having multiple sex partners, should be avoided.
All blood donors are tested for hepatitis B to prevent the spread of hepatitis B virus through transfusions. Also, even though the chance of getting hepatitis from transfusions is remote, doctors use transfusions only when there is no alternative. These measures have dramatically decreased the risk of getting hepatitis from a blood transfusion.
-
Any adult who wishes protection from hepatitis B
-
All unvaccinated adults whose risk of getting hepatitis B is increased, including pregnant women
-
People with chronic liver disease
If family members and close contacts of people with chronic hepatitis B have not been vaccinated, they should be vaccinated with the hepatitis B vaccine.
If the level of hepatitis B virus is high in pregnant women, they are often given antiviral drugs during the last trimester of pregnancy to prevent transmission of the virus from mother to child.
If people come in contact with the blood of someone who has hepatitis B, they are given hepatitis B immune globulin by injection. If they have not been vaccinated against hepatitis B, they are also vaccinated. If they have been vaccinated, blood tests are done to determine whether they are still protected. If they are not, they are vaccinated.
Don’t Miss: How Would You Know If You Have Hepatitis
Deterrence And Patient Education
Patient education remains one of the most important components in preventative measures regarding HBV infection.
Education should be provided to expecting parents about the importance of vaccination and to clarify erroneous beliefs about vaccinations.Patient education should also include counseling about the avoidance of risky behaviors that predispose an individual to be infected, including promiscuous sexual activity or intravenous drug abuse. They should also be advised not to share items such as shaving razors, toothbrushes, or hair combs due to possible transmission via mucosal contact or through microtrauma to protective barriers.
Chronic Hepatitis B Treatment
The aim of treatment in patients with hepatitis B is to prevent progression to liver cirrhosis, liver failure and liver cancer and to prevent transmission of the disease to others. People with chronic hepatitis B should maintain a healthy diet and avoid alcohol and unnecessary medications.
Regular blood tests to monitor the health of the liver will be recommended. Biopsies of the liver may also be recommended to monitor the seriousness of any liver damage over time.
The serious liver complications of chronic hepatitis B can be prevented if the disease is detected and treated in its early stages. Chronic hepatitis B is treated with antiviral medication that reduces the viral load on the body and allows the immune system to keep infection in check.
The main medications used in the treatment of chronic hepatitis B are:
Liver transplantation may be a treatment option for some patients with liver cancer or liver failure. Hepatitis B-specific immune globulin and antiviral medication is usually used before and after the transplant procedure to prevent recurrence of the hepatitis B virus.
Read Also: Hepatitis B Vaccine For Newborns
Acute Vs Chronic Hepatitis B
A hepatitis B infection can result in either an acute infection or a chronic infection. When a person is first infected with the hepatitis B virus, it is called an “acute infection” . Most healthy adults that are infected do not have any symptoms and are able to get rid of the virus without any problems. Some adults are unable to get rid of the virus after six months and they are diagnosed as having a “chronic infection.” A simple blood test can diagnose an acute or chronic hepatitis B infection.
The risk of developing a chronic hepatitis B infection is directly related to the age at which a person is first exposed to the hepatitis B virus. The younger a person is when they are first infected, the greater the risk of developing a chronic hepatitis B infection:
- More than 90% of infants that are infected will develop a chronic hepatitis B infection
- Up to 50% of young children between 1 and 5 years who are infected will develop a chronic hepatitis B infection
- 5-10% of healthy adults 19 years and older who are infected will develop a chronic hepatitis B infection
The recommendation for hepatitis B vaccination of babies and children is so important because they are at the greatest risk of developing a chronic infection if they are not protected against the hepatitis B virus as soon as possible.
Treatment Of Acute Liver Failure Due To Hepatitis B
No placebo-controlled trial has been published in the setting of established acute liver failure, but several cases series have suggested lower mortality in patients with fulminant hepatitis B compared to case series of patients who did not receive antiviral therapy. Most of these studies recruited patients before they had progressed to more advanced hepatic encephalopathy . In a study recruiting patients with more advanced liver failure, no benefit of nucleoside on survival was observed , but those authors still concluded that nucleoside analogues would be indicated in such patients to reduce viral load prior to potential liver transplantation. It is likely that early intervention is crucial. N-acetyl cysteine, which is highly effective in preventing death from liver failure from paracetamol/acetaminophen overdosing, has limited efficacy once hepatic encephalopathy is present. While early antiviral intervention is likely to be more effective when given early, we suggest that it should also be given at later time points, as it at least diminishes the risk of HBV reinfection should liver transplantation be required. In case of transplantation, it is unclear whether antiviral therapy can be stopped soon after or if long-term antiviral treatment is required. If transplantation can be avoided, antiviral treatment should be continued at least until HBsAg clearance.
Read Also: How Do You Test For Hepatitis C
Chronic Hepatitis B Infection
People who test positive for the hepatitis B virus for more than six months are diagnosed as having a chronic infection. This means their immune system was not able to get rid of the hepatitis B virus and it still remains in their blood and liver.
The risk of developing a chronic hepatitis B infection is also directly related to the age at which one first becomes exposed to the hepatitis B virus:
- 90% of infected newborns and babies will develop a chronic hepatitis B infection
- Up to 50% of infected children will develop a chronic hepatitis B infection
- 5-10% of infected adults will develop a chronic hepatitis B infection
Learning that you have a chronic hepatitis B infection can be very upsetting. Because most people do not have symptoms and can be diagnosed decades after their initial exposure to the hepatitis B virus, it can be a shock and a surprise to be diagnosed with a chronic hepatitis B infection. The good news is that most people with chronic hepatitis B should expect to live a long and healthy life.
There are effective drug therapies that can control and even stop the hepatitis B virus from further damaging a liver. There are also promising new drugs in the research pipeline that could provide a cure in the very near future. Although the risk of developing a serious liver disease or liver cancer is higher for those living with chronic hepatitis B than those who are not infected, there are still many simple things a person can do to help reduce their risks.
Can Hepatitis B Be Prevented
The hepatitis B vaccine is one of the best ways to control the disease. It is safe, effective and widely available. More than one billion doses of the vaccine have been administered globally since 1982. The World Health Organization says the vaccine is 98-100% effective in guarding against the virus. Newborns should be vaccinated.
The disease has also been more widely prevented thanks to:
- Widespread global adoption of safe blood-handling practices. WHO says 97% of the blood donated around the world is now screened for HBV and other diseases.
- Safer blood injection practices, using clean needles.
- Safe-sex practices.
You can help prevent hepatitis B infections by:
- Practicing safe sex .
- Never sharing personal care items like toothbrushes or razors.
- Getting tattoos or piercings only at shops that employ safe hygiene practices.
- Not sharing needles to use drugs.
- Asking your healthcare provider for blood tests to determine if you have HBV or if you are immune.
Read Also: Can A Child Get Hepatitis C
Treatment For Acute Hepatitis B
Acute HBV infection has in the past been associated with a number of extrahepatic manifestations. Most of these are believed to be related to immune complex formation with either HBeAg or HBsAg. Therefore, one might consider interferon-based therapies to be potentially more effective than purely antiviral therapies interferon also has been associated with stronger reduction of HBeAg and HBsAg than pure antivirals. Some recent papers, however, have also reported success with direct antiviral therapy, which remains the only option for interferon intolerant patients.
Interestingly, as acute HBV infections decrease, patients presenting with extrahepatic manifestations due to acute HBV infection are also seen less frequently . In our experience, we do not recall any patient with acute hepatitis and significant extrahepatic manifestations such are renal disease of polyarteritis nodosa. Still, it is important to be aware that HBV may be associated with extrahepatic diseases.
Interestingly, while HCV is associated with membranoproliferative glomerulonephritis, glomerulopathies associated with HBV were found to be dominantly membranous glomerulopathy .
Another manifestation reported with HBV is Gianotti-Crosti syndrome. This is a syndrome of skin eruption described as papular acrodermatitis. It is mostly limited to children and not limited to HBV, but reported with acute HBV infection .
Hepatitis B Treatment Guidance Recommendations
Several leading organizations have addressed guidance for treatment of chronic HBV, including when to initiate treatment. The following summary is intended to provide a succinct description of the indications for initiating HBV treatment in persons with chronic HBV, as outlined by the different organizational guidelines. The reader is encouraged to access these documents for additional details, descriptions, and discussion. The following summaries do not include guidance for the treatment of HBV in special situations or circumstances, such as reactivation of HBV, pre- or post-liver transplantation, treatment of HBV in persons who have coinfection , or treatment of HBV reactivation in persons undergoing immunosuppressive or cytotoxic therapy. These issues are addressed later in this topic review.
Read Also: How Does The Hepatitis B Vaccine Work
What Are The Complications Of Hepatitis B
The course of hepatitis B infection depends mostly on the age at which a person is infected.
People infected as infants are likely to develop long term infection and can get complications such as scarring of the liver or liver cancer. Infants have a 9 in 10 chance and children have a 3 in 10 chance of developing a chronic, lifelong infection.
People infected as teenagers or adults are likely to become unwell with symptoms , but have a smaller chance of developing a chronic infection. Others develop a silent infection, without any symptoms.
Most people infected as adults clear the virus from the body within 6 months. They develop immunity to future hepatitis B infections and do not develop long-term liver damage.
However, approximately 1 in 20 adults cannot clear the virus and develop chronic hepatitis B. They are at risk of developing complications such as cirrhosis and liver cancer in the longer term.