Pathogenesis Of Hepatitis C Infection
Once inside the host, the HCV is transported in the blood to the liver, where it infects liver cells, although other types of cell, including blood cells, may also be infected. The incubation period for acute HCV infection is usually around 70 days, but can range from 2 to 26 weeks. The acute phase of HCV infection is often without symptoms, or mild. Diagnosis of infection is by detection of antibodies or virus RNA and/or antigen in serum. If the infection proceeds to a chronic phase, progression of liver damage is usually slow, and the most common complaint is fatigue. Liver enzyme abnormalities may fluctuate or persist, and the degree of liver damage is variable. The Department of Health estimates that between 60 to 80% of patients with acute HCV infection go on to develop chronic infection with a variable degree of hepatitis, with the risk of cirrhosis and, in a smaller number, primary liver cancer several decades later.
What Are The Chances Of Getting Hep C Sexually
Hepatitis C can be transmitted through sexual activity, but it is uncommon. It is estimated that among heterosexual couples, the risk of getting hepatitis C through sexual activity is approximately 1 in 380,000 individuals. However, you are at a greater risk of getting hepatitis C if you have a sexually transmitted infection or have sex with multiple partners.
Heterosexual Transmission Of Hcv
Heterosexual transmission of HCV is widely considered to be inefficient . Prospective studies of heterosexual monogamous couples reported incident transmission rates of up to 0.6% per year . A literature review found no increased risk of sexual transmission of HCV among heterosexual couples in monogamous relationships
Also Check: Cure For Hepatitis A And B
Premature Rupture Of The Membranes
Premature rupture of the membranes is considered a risk factor for HCV vertical transmission by exposing the fetus to maternal HCV in the birth canal. The duration of rupture has been found to be significantly longer in infected children. These parameters are potentially related to contamination of the fetus with infected maternal blood in the birth canal.
Diagnosis Of Hcv Infection
2.7.1. Recombinant immunoblot assay
This test can detect viral antigens and is performed for confirmation of specific serological test.
2.7.2. Polymerase chain reaction
Different molecular techniques such as real-time PCR, reverse transcriptase PCR, transcription mediated amplification , and branched DNA can detect HCV RNA among serum or plasma of patients. This diagnostic method was more useful in cases in which virus counts are low. Determine of HCV genotype is performed with 5â² noncoding sequence and Trugene 5/NC and it is useful to predict the patientâs outcome .
2.7.3. Liver biopsy and fibroscan
Read Also: What Lab Test For Hepatitis C
Sexual Transmission And Hepatitis B
Hepatitis B can be transmitted through sexual activity. Unvaccinated adults who have multiple sex partners, along with sex partners of people with chronic hepatitis B infection, are at increased risk for transmission. Injection-drug use and sexual contact are other common modes of hepatitis B transmission in the United States.
Among adults seeking treatment in STD clinics, as many as 10%40% have evidence of past or current hepatitis B virus infection. Many of these infections could have been prevented through universal vaccination during delivery of STD prevention or treatment services. Offering vaccination to all adults as part of routine prevention services in STD treatment facilities has been demonstrated to increase vaccination coverage among adults at risk for hepatitis B infection, as the behavioral risk factors for STDs and hepatitis B are similar.
Transmission Of Hepatitis C
Routine screening of blood donors has been introduced to prevent transmission via transfusion and the use of blood products. The greatest risk of acquiring HCV in the UK is now through sharing of blood-contaminated needles and injecting equipment among drug users.
Routine screening of blood donors has been introduced to prevent transmission via transfusion and the use of blood products. The greatest risk of acquiring hepatitis C in the UK is now through sharing of blood-contaminated needles and injecting equipment among drug users. Workplace exposure in the healthcare setting usually occurs as a result of a needle-stick or injury with other contaminated sharp instruments, and rates of occupational exposure and transmission are presented in HPA’s Eye of the Needle report. Exposure to other contaminated sharp injuries, for instance, via tattooing and skin piercing, may also result in infection. Mother-to-baby transmission occurs at a rate of about 3-5% .
You May Like: How Does Someone Contract Hepatitis
Blood Transfusion/receipt Of Blood Products
Early case-control studies of patients with newly acquired, symptomatic non-A, non-B hepatitis found a significant association between disease acquisition and a history six months prior to illness of blood transfusions, injection drug use, health care employment with frequent exposure to blood, personal contact with others who had hepatitis, multiple sexual partners or low socioeconomic status. Today, HCV is rarely transmitted by blood transfusion or transplantation of organs due to thorough screening of the blood supply for the presence of the virus and inactivation procedures that destroy bloodborne viruses. In the last several years, blood banks have instituted techniques that utilize nucleic acid amplification of the hepatitis C virus, which will detect the presence of virus even in newly-infected patients who are still hepatitis C antibody-negative. These techniques are estimated to have prevented 56 transfusion-associated HCV infections per year in the U.S. since 1999, and have lowered the current risk of acquiring HCV via transfused blood products to 1 in 2 million.
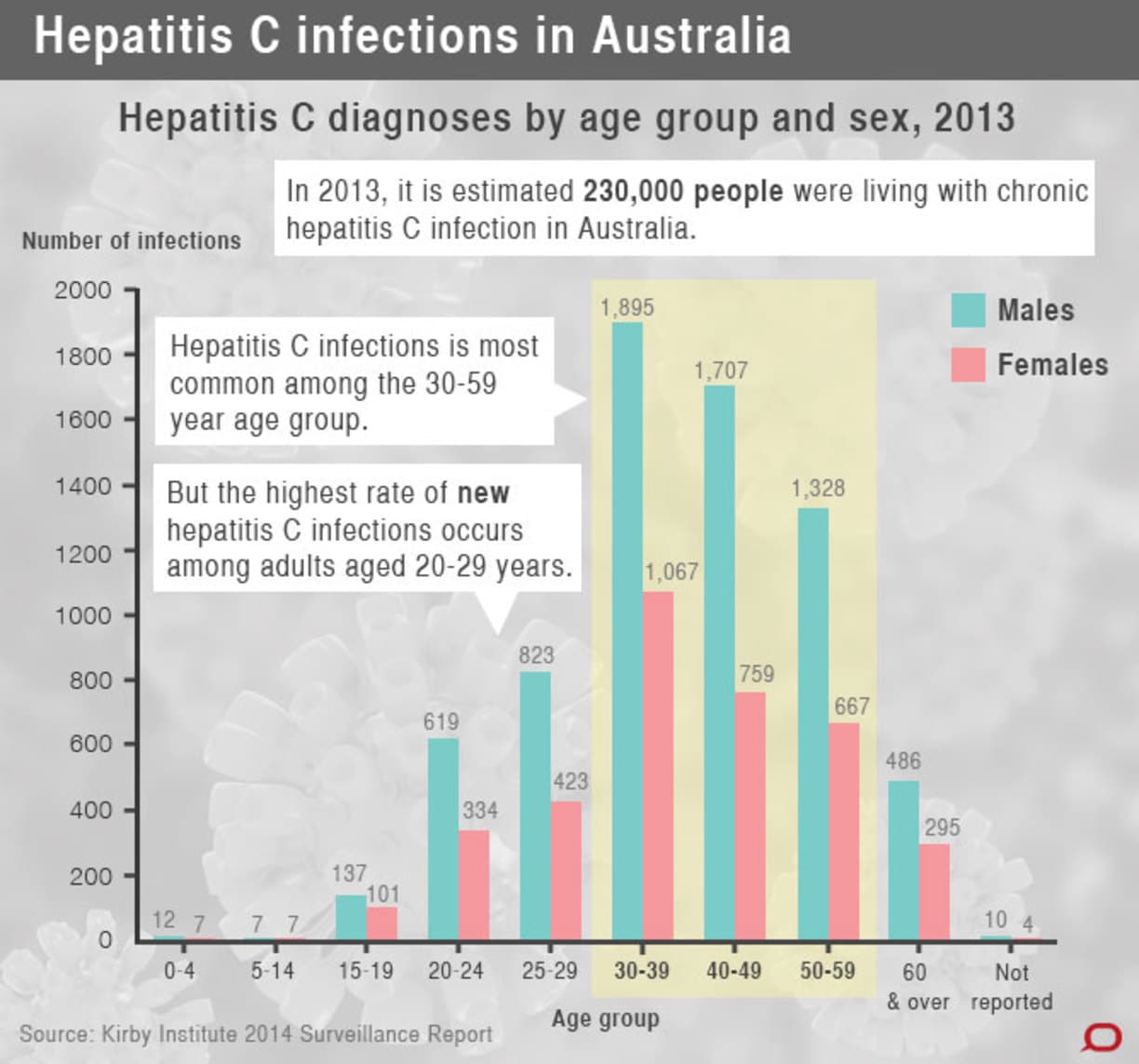
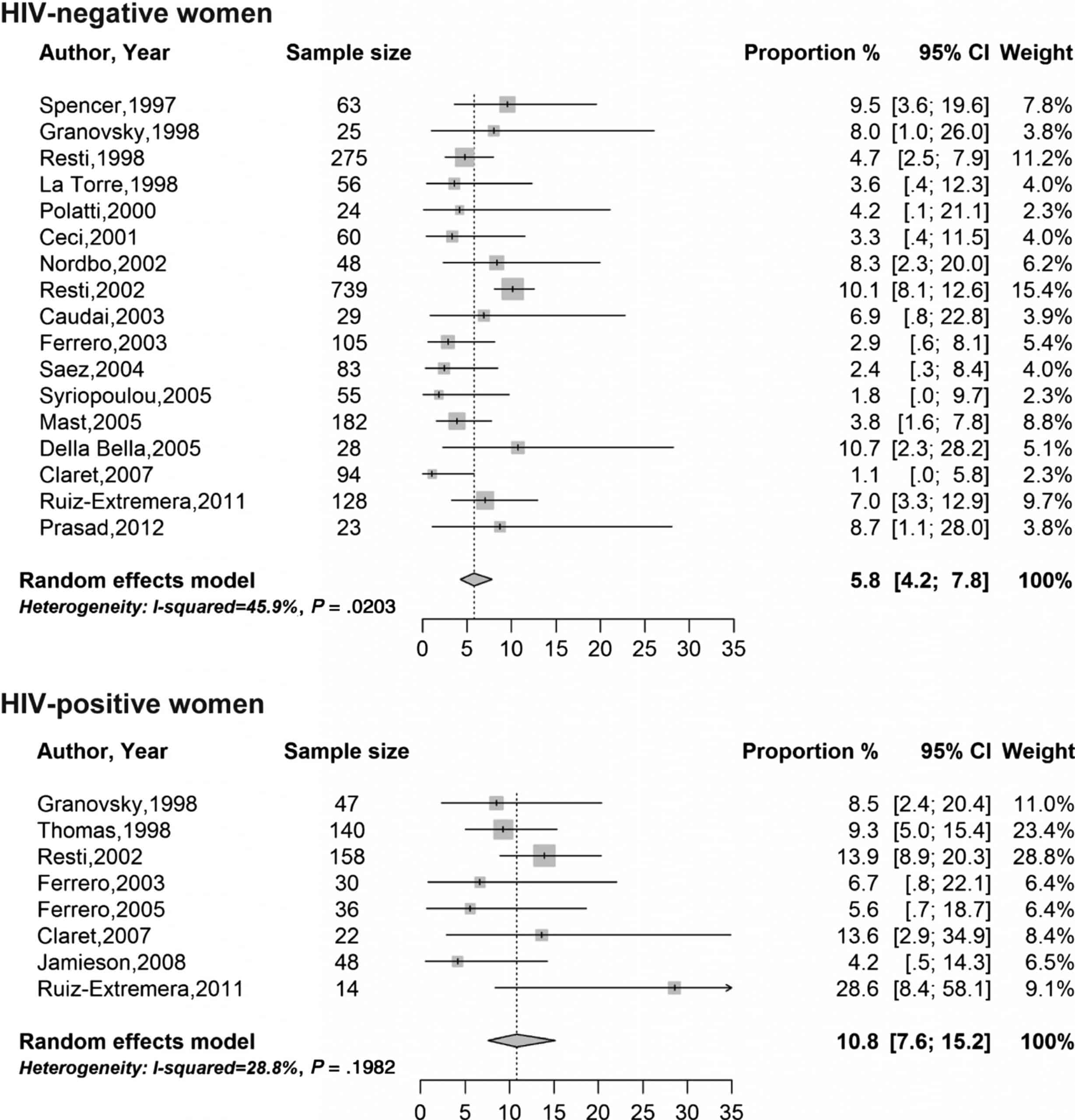
Risk Of Perinatal Hcv Transmission
Perinatal transmission of hepatitis C occurs in approximately 5 to 6% of pregnant women with HCV who have viremia, a rate significantly lower than with perinatal transmission of hepatitis B or HIV. The timing of perinatal HCV transmission is poorly understood, but intrauterine, intrapartum, and postnatal transmission are possible, with the majority of infants likely becoming infected in utero or around the time of delivery. In a systematic review of 77 studies published between 1990 and 2000, investigators calculated a 4.3% rate of mother-to-infant transmission among women with HCV viremia. A more recent systematic review and meta-analysis of 109 articles reported a 5.8% risk of perinatal HCV transmission among women who are HCV antibody positive and HCV RNA positive.
Also Check: Sign And Symptoms Of Hepatitis B
Also Check: Getting Paid For Hepatitis B Plasma
Hcv Prevalence Among Pregnant Women In African Countries
Africa is geographically divided into 5 regions with heterogeneity in religion, culture and practices, and with a high human immune-deficiency virus burden in sub-Saharan areas. Arab countries lie at the northern region. Most of the countries in the other four regions suffer from political conflicts, military confrontations, droughts and famines, leading to large numbers of internally and externally displaced people which might increase the prevalence of sexually transmitted diseases .
A systematic review and meta-analysis study published in 2015, conducted in 21 sub-Saharan African countries, found that the overall HCV prevalence among pregnant women in antenatal clinics was 3% and was 2% in the Central African region .
Sexual Transmission And Hepatitis A
Transmission of hepatitis A virus can occur from any sexual activity with an infected person and is not limited to fecal-oral contact. People who are sexually active are considered at risk for hepatitis A if they are MSM, live with or are having sex with an infected person, or inject drugs. Vaccination is the most effective means of preventing hepatitis A transmission among people at risk for infection. CDC has published recommendations for prevention of hepatitis A that identify all groups recommended for vaccination, including hepatitis A vaccination for MSM.
You May Like: Who Should Get Tested For Hepatitis C
Gay Men Chemsex And Hep C
Group sex and chemsex parties provide the perfect storm for hepatitis C transmission.
The iBase guide Safer HCV sex for gay men is a useful reminder of what to avoid and what steps to take to protect yourself.
The Hepatitis C Trust has some useful information about transmission. They also provide an advocacy service for men who have sex with men who have been re-infected with hepatitis C after previously being successfully treated.
Donât Miss: Hepatitis C Without Hepatic Coma
Hcv Transmission By Blood
HCV transmission has considerably changed, reflecting both the evolution of medicine, in particular the cloning of the HCV, and health and social changes. The main modes of HCV transmission are parenteral exposure, unapparent parenteral transmission and occupational exposure. Blood transfusion was the main risk factor for HCV infection before donor screening for surrogate marker testing for non-A and non-B hepatitis which began in the mid-1980s, followed by screening for antibodies to HCV in 1990 . After 1985, the incidence of post-transfusion HCV infection has been halved by excluding HIV-positive people in developed countries . Moreover, since 1993, the availability of more sensitive tests has further reduced this prevalence. However, given that anti-HCV antibodies are not detectable for several weeks or months in recently infected donors blood, in some countries, all donations are tested by nucleic acid amplification tests for the presence of HCV RNA. The WHO reports that 39 countries do not routinely screen blood transfusions for blood-borne viruses . The generalised epidemic of HCV infection in Egypt is an example of health careassociated transmission originating from unsafe injection practices, where, in 2015, HCV RNA prevalence was 7.7% in some regions .
In Italy, in 2013, the prevalence was 80.8/100,000 in first time donors and the incidence rate was 2.5/100,000 in first time donors .
You May Like: Long Term Effects Of Hepatitis C
Reducing The Burden Of Hcv
In 2010, the World Health Assembly adopted a resolution calling for a comprehensive approach for the prevention, control and management of viral hepatitis. In passing this resolution, member states recognized the tremendous burden of viral hepatitis. In line with this resolution, the WHO established a Global Hepatitis Programme and released a framework in 2012 for global action on viral hepatitis, outlining four axes for action with suggested approaches for member states to adopt or adapt as they see fit. As these axes are from a global point of view, each country should adapt actions depending on the local burden of disease and routes of transmission.
What Should You Know About Pregnancy And Hepatitis B
A pregnant woman who has hepatitis B can pass the infection to her baby at delivery. This is true for both vaginal and cesarean deliveries.
You should ask your healthcare provider to test you for hepatitis B when you find out you are pregnant. However, while it is important for you and your healthcare provider to know if you do have hepatitis B, the condition should not affect the way that your pregnancy progresses.
If you do test positive, your provider may suggest that you contact another healthcare provider, a liver doctor, who is skilled in managing people with hepatitis B infections. You may have a high viral load and may need treatment during the last 3 months of your pregnancy. A viral load is the term for how much of the infection you have inside of you.
You can prevent your infant from getting hepatitis B infection by making sure that your baby gets the hepatitis B vaccine in the hours after they are born along with the hepatitis B immunoglobulin. These two shots are given in two different locations on the baby. They are the first shots needed.
Depending on the type of vaccine used, two or three more doses must be given, usually when the baby is 1 month old and then 6 months old, with the last by the time the baby is 1 year old. It is critical that all newborns get the hepatitis B vaccination, but even more important if you have hepatitis B yourself.
Don’t Miss: Hepatitis B And C Vaccine
Brief Communicationtransmission Of Hepatitis C Virus By Occupational Percutaneous Injuries In South Korea
Korea is an endemic area of hepatitis. Hepatitis C virus infections caused by occupational percutaneous injuries are a serious problem for healthcare workers and there has been a gradual increase in the number of HCV infections. We therefore determined the transmission rate of HCV after occupational percutaneous injury. This was a retrospective cohort study reviewing all occupational blood exposure reports made between January 1, 2004, and December 31, 2008, at a university-affiliated acute care hospital. Over the 5-year study period, there were 1,516 accidents of occupational exposure to blood of these, 327 were to the blood of HCV-infected patients and 3 healthcare workers became infected with HCV . In Korea, although the bloodborne accidents leading to exposure to HCV occurred frequently , the transmission rate was very low .
How Are Hepatitis B And Hepatitis C Spread From Person To Person
Like HIV, the hepatitis B and hepatitis C viruses spread:
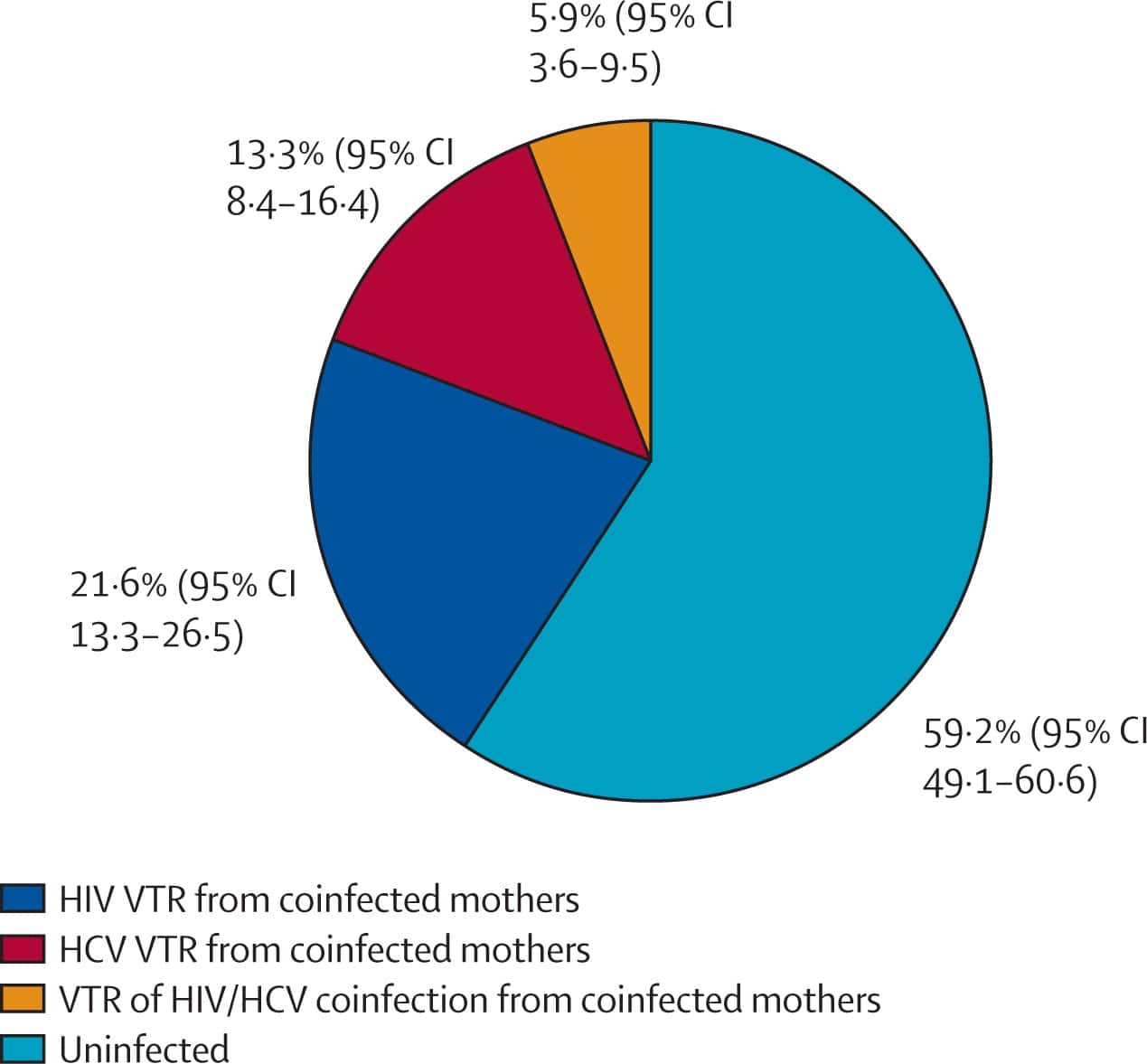
- Perinatally: Pregnant people can pass these infections to their infants. HIV-HCV coinfection increases the risk of passing on hepatitis C to the baby.
- Sexually: Both viruses can also be transmitted sexually, but HBV is much more likely than HCV to be transmitted sexually. Sexual transmission of HCV is most likely to happen among gay and bisexual men who have HIV.
Read Also: Hepatitis C Reactive Test Results
Risk Factors Of Vertical Transmission
Multiple risk factors were studied to increase the risk of HCV vertical transmission, including coinfections with HIV, intravenous drug use, high maternal HCV viral load, mode of delivery, preterm labor, prolonged rupture of membranes and amniocentesis, while breastfeeding and HCV genotypes have little impact on vertical transmission. However, most of the reports are still controversial.
No Identifiable Source Of Infection
According to the Centers for Disease Control and Prevention, injection drug use accounts for approximately 60% of all HCV infections in the United States, while other known exposures account for 20-30%. Approximately 10% of patients in most epidemiological studies, however, have no identifiable source of infection. HCV exposure in these patients may be from a number of uncommon modes of transmission, including vertical transmission, and parenteral transmission from medical or dental procedures prior to the availability of HCV testing. There are no conclusive data to show that persons with a history of exposures such as intranasal cocaine use, tattooing or body piercing are at an increased risk for HCV infection based on these exposures solely. It is believed, however, that these are potential modes of HCV acquisition in the absence of adequate sterilization techniques.
Recommended Reading: Why Is My Doctor Testing Me For Hepatitis C
Hcv Prevalence For Males Aged 1649 Years
Table 3
Observed hepatitis C virus antibody prevalence rates for male 1649 year olds in five year age bands undergoing, or eligible to undergo, surgery
Figure 1 summarises the results of pooled HCV antibody testing and confirmatory testing of samples reactive on individual testing. The overall prevalence of HCV antibodies was 3.8% . Observed prevalence rates among males aged 1649 years varied from 1.6% among cardiothoracic/cardiology patients at Stobhill General Hospital to 6.3% among general surgery/ENT patients at Glasgow Royal Infirmary . No statistically significant difference in overall prevalence was observed between the hospitals however, there was a significant difference in the prevalence observed among specialty groupings .
Figure 1
Summary of testing 2702 hospital inpatient and outpatient sera for antibodies to hepatitis C virus by Ortho ELISA-3 in pools of five.
Table 3 summarises the prevalence of HCV antibodies according to age band of those tested. A significant difference was observed in anti-HCV prevalence among different age groups the highest prevalences were observed in the 2529 year and 3034 year age bands . There were no significant differences in the prevalence of anti-HCV among specialties in any of the age bands.
Diagnosis Of Perinatal Transmission
A practical and widely acceptable recommendation by most studies is to consider children born to anti-HCV positive mothers infected with HCV when: HCV RNA is detected in at least two serum samples and at least three months apart during the first year of life and HCV antibody is positive after 18 mo of age. There is agreement on delaying PCR testing until 3 mo of age and to repeat it, if positive, at 6 mo of age. Testing of HCV antibody is of limited value before 18 mo of age due to passive transfer of maternal antibodies.
Read Also: How To Get Hepatitis B Vaccine
Prevalence Of The Hepatitis C Virus In The Uk
HCV infection is a major worldwide public health problem, although the UK is thought to be a low prevalence area. Based on seroprevalent studies performed on residual specimens, the prevalence of HCV in England is predicted to be around 0.5-1%. As with HIV infection, the prevalence of HCV is often higher in major cities or other highly populated regions, compared to other parts of the UK, and is mostly associated with high-risk groups. This is demonstrated by the high incidence of hepatitis C among injecting drug users in Glasgow, London and the North West of England, ). Recent mathematical modelling data cited by the Health Protection Agency indicates that, within England and Wales, 191 000 individuals had antibodies to hepatitis C virus. HPA also report 12 000 chronically infected individuals in Wales. In Scotland, , around 50 000 people were estimated to be infected with hepatitis C 38,000 with chronic infection. Estimates from Northern Ireland suggest that around 4000 individuals are likely to be chronically infected.
Most infections are due to injecting drug use. Since the discovery of HIV , there has been raised awareness of the transmission of blood-borne viruses through shared injecting equipment. However, a significant number of chronic infections may have been acquired in the 1970s and 1980s through contaminated blood products, before routine screening was introduced.
Natural History Of Hcv Infection In Infected Pregnant Women
Pregnancy is considered a state of relative immunodeficiency , especially T-cell mediated immunity , with a shift in the Th1/Th2 balance toward the Th2 response, and expansion of regulatory T-cells , to safeguard against rejection of the newly developing embryo by the maternal immune system . This alteration in the immune system directly alters the natural course of HCV infection, giving more room for the virus to replicate while suppressing its immune-mediated damage to hepatocytes, which is demonstrated by the surprising finding of increasing viral RNA load with concomitant decreasing ALT levels .
It was reported that estrogen suppresses the intra-thymic T-cell differentiation while activating the extra-thymic pathways during pregnancy . After delivery, the maternal immune system regains its baseline activity with the resultant decrease in viral load and increase in immune-mediated hepatocyte damage and consequently ALT level . Spontaneous resolution of HCV viremia postpartum has also been reported .
Another maternal obstetric complication of HCV is the earlier and more frequent development of cholestasis in HCV infected than non-infected women, which could be attributed to the altered transport of sulfated hormones in the liver, a failure in the transport of toxic substances, and a defect of the bile salt export pump .
You May Like: What Are The Side Effects Of Hepatitis