What Is The Connection Between Hiv And Hcv
Because both HIV and HCV can spread in blood, a major risk factor for both HIV and HCV infection is injection drug use. Sharing needles or other drug injection equipment increases the risk of contact with HIV- or HCV-infected blood.
According to the Centers for Disease Control and Prevention , approximately 21% of people with HIV in the United States also have HCV. Infection with both HIV and HCV is called HIV/HCV coinfection.
In people with HIV/HCV coinfection, HIV may cause chronic HCV to advance faster. Whether HCV causes HIV to advance faster is unclear.
Hepatitis C & Hiv Coinfection
People living with HIV are more likely to have been exposed to hepatitis C than people who are HIV-negative.
If youre living with hepatitis C and HIV:
- You may have more difficulty getting an accurate hepatitis C test result
- You may have a higher concentration of the hepatitis C virus in your body fluids
- You may have higher HIV viral loads but probably wont experience faster HIV disease progression
- You can safely treat both infections, although usually not beginning at the same time since this can make side effects worse.
- You must have your liver enzymes monitored regularly since HIV medications can cause liver inflammation or damage.
As Hiv Funding Goes Down Hiv Infections In Canada Increase We Can Stop This
Why have HIV infections been increasing when we have more and better prevention options at our disposal than ever before?
Ask our federal decision-makers, who have not increased funding for the HIV response since 2008, and even fell short on spending the funds that had been allocated to the federal HIV initiative.
You May Like: Hepatitis B Surface Antibody Quant
What Is Hepatitis C
Hepatitis C is a liver infection caused by the hepatitis C virus . The abbreviation HCV can stand for either the virus or the infection it causes.
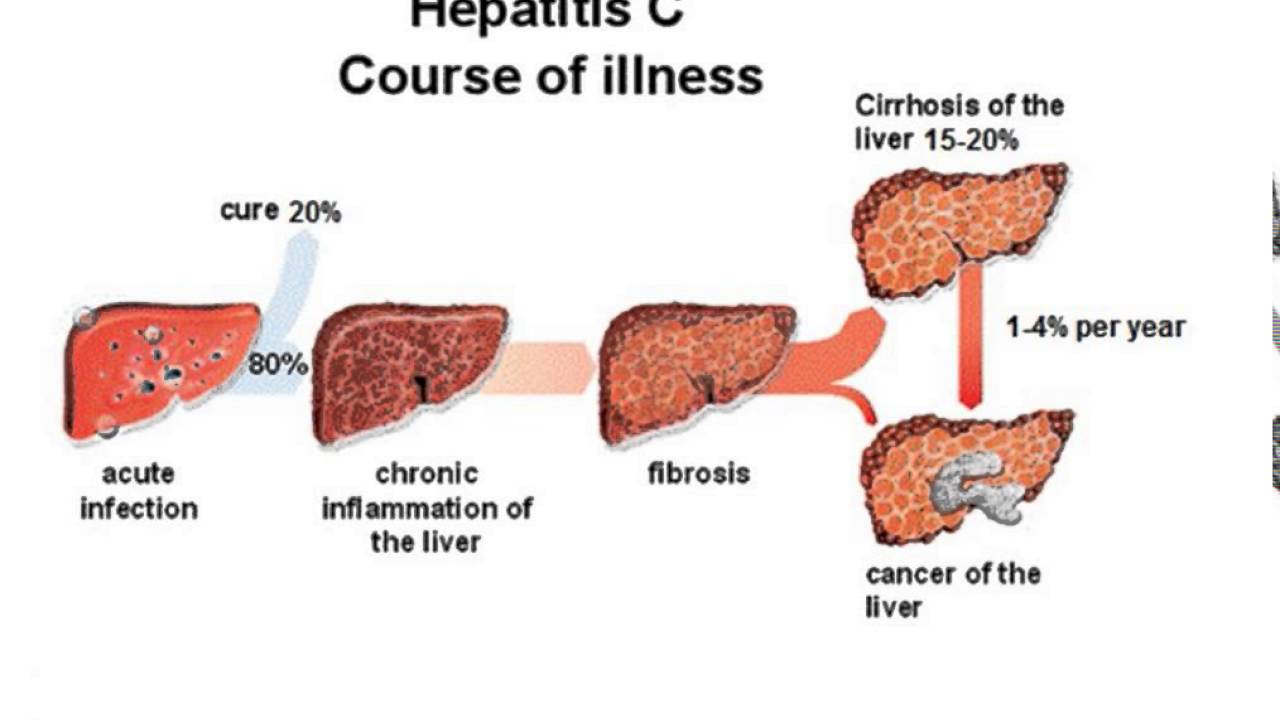
HCV can be either a short-term or a long-term illness:
- Acute HCV occurs within 6 months after exposure. In most people, acute HCV becomes chronic HCV.
- Chronic HCV can last a lifetime. Without treatment, chronic HCV can cause liver cancer or severe liver damage that can lead to liver failure.
- HCV is a contagious infection that can spread from person to person.
Intergovernmental Committee On Hiv/aids Hepatitis C And Related Diseases
This report published in Communicable Diseases Intelligence Volume 26, No 3, September 2002 describes the role and activities of the Intergovernmental Committee on HIV/AIDS, Hepatitis C and Related Diseases.
Page last updated: 03 October 2002
A print friendly PDF version is available from this Communicable Diseases Intelligence issue’s table of contents.
Also Check: What Is Hepatitis C Antibody Mean
Symptoms Of Hepatitis C
Many people with hepatitis C have no symptoms at all. When symptoms do occur they often involve the following:
- tiredness
- stomach problems
- jaundice a yellowing of the skin and eyes.
Some people will clear the virus without treatment, but this is less likely in the case of people living with HIV.
For most people, hepatitis C continues to reproduce in the body long after infection, turning into a chronic infection. This means that they continue to be infectious, although they may not experience any symptoms at all, or not for many years.
Even with a lack of symptoms, the virus may still be damaging the liver, causing fibrosis a hardening of the liver. This can lead to cirrhosis, which is a permanent scarring of the liver. Cirrhosis increases the risk of liver cancer.
Overview Of Hcv Medication Options
The backbone of HCV treatment has long been the combination of pegylated interferon alpha with or without ribavirin. PEG-IFN is a combination of three antivirals that elicits cells to produce a large amount of enzymes able to kill both the virus and infected host cells. Ribavirin, another antiviral agent, interferes with RNA metabolism necessary for viral replication.
A 2018 medical study showed that newer direct acting antivirals are increasingly able to treat a variety of hepatitis C genotypes without the use of PEG-INF and, in many cases, ribavirin. By doing so, the side effects associated with HCV therapy is greatly reduced, as is the duration of treatment.
Among the currently approved DAAs used in the treatment of chronic hepatitis C infection :
| Drug | |||
| genotype 1 with or without cirrhosis | peginterferon + ribavirin, or Sovaldi , where indicated | one capsule daily with food | 24-48 weeks |
You May Like: What Causes Hepatitis Of The Liver
Resources For Drug Interaction
Most persons with HIV infection are taking multidrug antiretroviral therapy, which may pose a problem with drug interactions when initiating HCV treatment. For resources on drug interactions that may occur with HIV antiretroviral medications and HCV treatment medications, access the following sites:
- AASLD-IDSA HCV Guidance: Patients with HIV/HCV Coinfection
Hepatitis C Treatment Programmes
An important first step to providing treatment for people with hepatitis C and HIV co-infection is to diagnose infections. HIV services should routinely screen all patients for hepatitis C.
However, guidelines recommending screening are often poorly implemented, especially in low and middle-income countries. Hepatitis C testing may not be systematically provided to groups which have elevated rates of hepatitis C, such as people who inject drugs, prisoners, sex workers, and men who have sex with men.43
Don’t Miss: Is Hepatitis C An Std
Impact Of Hcv Treatment On Hiv Disease Progression
Treatment of HCV infection has evolved over the last decade with an increasingly higher percentage of patients achieving sustained viral clearance following the introduction of combination based therapies with interferon and ribavirin, and more recently pegylated interferon., Of note, HCV-HIV coinfected patients were all excluded from placebo controlled trials with interferon alpha. However, the results of nine non-placebo controlled trials, showed an equivalent percentage who had a sustained response to HCV therapy in coinfected compared with HCV only infected individuals. This ranged between 8% and 29%, although the interferon dosage and duration varied considerably across the different studies . Side effects of interferon in coinfected patients were comparable with HIV uninfected patients. Over 90% of patients were able to complete their treatment course indicating that interferon is well tolerated even when used in conjunction with antiretroviral therapy. A 5% drop in CD4 cell count occurred in less than 5% of patients treated, and occurred in the first 10 weeks of therapy. However, this decline in CD4 count may be clinically significant and contribute to the subsequent development of opportunistic infections.
The development of a helicase inhibitor, which is anticipated in the near future, together with other novel approaches, are antisense genes, ribozymes, and HCV specific protease inhibitors
Hepatitis C Treatment Guidelines
Guidelines issued by WHO in April 2016 recommend four preferred regimens, each including the drug sofosbuvir, in order to simplify treatment decisions for hepatitis C.36 Depending on the regimen, treatment may last 12 or 24 weeks.
When these guidelines were issued, the choice of drug regimen was dependent on which of the six genotypes the patient had. Different genotypes, each with its own genetic composition of the virus, are more common in different parts of the world. Each patient therefore required genotype testing before treatment could be provided.
In July 2018, WHO updated these treatment guidelines to reflect certain key developments. It recommended that the use of DAA regimens for all people with chronic hepatitis C infection, rather than reserving DAA treatment for people with more advanced disease as had previously been done. In part, this is linked to the continued substantial reduction in , which has enabled treatment to be rolled out rapidly in a number of low- and middle-income countries. In addition, as several new pangenotypic DAA medicines have now been approved, the need for genotyping to guide treatment decisions has been reduced.37
Recommended Reading: Hepatitis C Transmission Routes Cdc
Improving Access For Key Populations
For people from key populations, stigma and structural barriers continue to hinder access to diagnosis, treatment and care for hepatitis C.44 .
To ensure equitable access and engage key populations, clinical services for hepatitis C will need to better adapt their models of care. They may need to provide outreach services, be flexible around appointment requirements, train staff, and consult civil society- and community-led organisations .45
Buyers clubs
Buyers clubs pool resources to buy DAA medicines via the internet. There are many buyers clubs around the world enabling people to access treatment who would otherwise be unable to receive it. They exist as a stopgap response to the failure of public health systems to ensure equitable access to hepatitis C treatment.
However, there are concerns that compromise other important aspects of treatment, including treatment monitoring and management of co-infection.46
People Coinfected With Hiv And Viral Hepatitis
People with HIV/AIDS should be vaccinated against hepatitis A and B and tested for hepatitis B and hepatitis C.
Beginning in 2020, CDC and the Advisory Committee on Immunization Practices began recommending that all people with HIV who are 1 year of age be vaccinated against hepatitis A and receive postvaccination serologic testing 1 month after completing the hepatitis A vaccine series.
Further, CDC and ACIP recommend that unvaccinated people with HIV receive hepatitis B vaccination. Vaccination should be followed by serologic testing to confirm adequate immune response. CDC recommends that people with HIV be tested for hepatitis B.
CDC now also recommends one-time hepatitis C testing of all adults , including those with HIV. CDC continues to recommend people with risk factors, like people who inject drugs, be tested regularly.
People with HIV and Hepatitis A
People with HIV and Hepatitis B
People with HIV and Hepatitis C
You May Like: How Do You Get Hepatitis A B C
Impact Of Highly Active Antiretroviral Hiv Therapy On Hcv Progression
A total of eight studies examined the impact of HAART on HCV progression. Five studies found no evidence for an effect of HAART on HCV replication, while two studies have reported significant transient increases in HCV viral load and transaminases ) following introduction of HAART. A protective effect of HAART on fibrosis progression has also been suggested but needs to be confirmed in large prospective studies. One report has also shown a significant increase in HCV viral load at 96 weeks post HAART compared with baseline, although samples taken at 24 weeks post HAART did not show a significant increase. The mechanism for the higher HCV-RNA levels with HAART despite immune restoration is unclear but is probably not associated with HIV related immune dysfunction. However, the increase in transaminases is associated with an improving immune response as shown by a correlation with a reduction in HIV viral load and increase in CD4 cell count. In one study, multivariate logistic regression analysis demonstrated that a HAART induced CD4 cell count increase of 50 cells or more was independently associated with severe hepatotoxicity in coinfected patients.
Hepatitis C Virus Infection Among Hiv
Melaku Ashagrie Belete
1Department of Medical Laboratory Science, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Abstract
1. Background
Hepatitis C Virus was first recognized in 1989 to be a cause of acute and chronic hepatitis related to transfusion . HCV is the second major viral infection next to human immunodeficiency virus for more than two decades which becomes a major public health problem causing estimated annual deaths of 350,000 patients worldwide . Globally, an estimated 71 million people are chronically infected with HCV globally , of which 5 million people are coinfected with both HIV and HCV . The prevalence of HIV/HCV coinfection is higher in developing nations which disproportionally varies geographically in sub-Saharan Africa from 0% to 22% .
Certain studies have been conducted in Ethiopia, but the magnitude of the problem and the predisposing factors are not well addressed and little is known about HCV/HIV coinfection including the rate of coinfection in our setting, Northeastern Ethiopia. Therefore, the aim of this study was to assess the seroprevalence of HCV infections and associated risk factors among HIV-infected patients on ART at Dessie Referral Hospital, Northeastern Ethiopia.
2. Method and Materials
2.1. Study Design and Setting
2.2. Sample Size Determination and Sampling Technique
2.3. Sociodemographic and Laboratory Data Collection and the Analysis Procedure
2.4. Anti-HCV Antibody Detection and CD4 Determination
Also Check: Is Hepatitis C And Hiv The Same
Hepatitis C Prevention Programmes
Both hepatitis C and HIV are readily transmitted through the sharing of equipment used to inject heroin, crack cocaine and other drugs. Therefore, services use the same approach to prevent transmission of both viruses in people who inject drugs.
should make sufficient quantities of sterile injecting equipment available. Opioid substitution therapy for people with drug dependency reduces the transmission of viral infections because it helps people inject drugs less often. It also helps engage people with healthcare.15
WHO also recommends peer interventions for people who inject drugs.16 Research suggests that combined programmes, rather than singular approaches, are more effective.17
Australia, New Zealand and Western Europe offer integrated hepatitis C, HIV and harm reduction services with promising results, leading to increased access to healthcare among people who use drugs, particularly when programmes involve peer outreach workers.18
Despite the scientific evidence in favour of harm reduction strategies, punitive instead of public health approaches for people who inject drugs are still frequent in many countries. Criminalisation and stigmatisation of people who inject drugs hinders prevention.1920A scale-up of hepatitis C treatment in people who inject drugs would reduce viral loads and make transmission less likely.21
Harm reduction expansion
Preventing Hepatitis C Infection
Here’s how you can protect yourself against hepatitis C:
- Do not share needles, syringes or any other equipment to inject drugs.
- Use latex gloves for fisting, with a new glove with each partner.
- Do not share pots of lubricant.
- Do not share sex toys, or put a new condom on the sex toy each time you use it.
- Properly used condoms provide excellent protection against the transmission of HIV, hepatitis C and other sexually transmitted infections.
- A caesarean delivery can reduce the risk of mother-to-child transmission of the virus.
Theres no vaccine for hepatitis C. Unlike hepatitis A and B, having hepatitis C once doesnt mean youre then immune from getting it again. Its possible to be reinfected with the hepatitis C virus.
Also Check: How To Read Hepatitis B Test Results
Should People With Hiv Get Tested For Hcv
Every person who has HIV should get tested for HCV. Usually, a person will first get an HCV antibody test. This test checks for HCV antibodies in the blood. HCV antibodies are disease-fighting proteins that the body produces in response to HCV infection.
A positive result on an HCV antibody test means that the person has been exposed to HCV at some point in their life. However, a positive antibody test does not necessarily mean the person has HCV. For this reason, a positive result on an HCV antibody test must be confirmed by a second test. This follow-up test checks to see if HCV is present in the personâs blood. A positive result on this test confirms that a person has HCV.
Living With Hepatitis C: Your Lifestyle
People living with HIV and hepatitis C can benefit from adopting a healthy lifestyle, including eating a balanced diet. Try to maintain a healthy weight. Being overweight is linked to fatty liver disease, which can worsen liver damage.
Since people living with HIV and hepatitis may have an increased risk of cardiovascular disease and diabetes, your clinic should regularly monitor your blood fats or lipids and blood sugar .
People living with hepatitis C should limit how much alcohol they drink, and those with liver damage should avoid alcohol altogether. Not smoking and cutting down or stopping recreational drug use are also important for overall health.
- Eat a balanced diet including vegetables, fruit and wholegrains.
- Get regular moderate exercise.
Recommended Reading: How To Contract Hepatitis B And C
Can Hcv Infection Be Prevented
The best protection against HCV is to never inject drugs. If you do inject drugs, always use new, sterile needles, and do not reuse or share needles, syringes, or other injection drug equipment.
People, including people with HIV, can also take the following steps to reduce their risk of HCV infection:
- Do not share toothbrushes, razors, or other personal items that may come in contact with another personâs blood.
- If you get a tattoo or body piercing, make sure the instruments used are sterile.
- Use condoms during sex. The risk of HCV infection through sexual contact is low, but the risk increases in people with HIV. Condoms also reduce the risk of HIV transmission and infection with other sexually transmitted diseases, such as gonorrhea and syphilis.
Hiv And Hepatitis B And Hepatitis C Coinfection
Hepatitis B and hepatitis C are liver infections caused by a virus. Because these infections can be spread in the same ways as HIV, people with HIV in the United States are often also affected by chronic viral hepatitis.
Viral hepatitis progresses faster and causes more liver-related health problems among people with HIV than among those who do not have HIV. Liver disease, much of which is related to HBV or HCV, is a major cause of non-AIDS-related deaths among people with HIV.
Given the risks of hepatitis B or hepatitis C coinfection to the health of people living with HIV, it is important to understand these risks, take steps to prevent infection, know your status, and, if necessary, get medical care from someone who is experienced in treating people who are coinfected with HIV and HBV, or HIV and HCV.
You May Like: Is There Now A Cure For Hepatitis C
How Does Drug Use Affect Symptoms And Outcomes Of A Viral Infection
Drug use can worsen the progression of HIV and its symptoms, especially in the brain. Studies show that drugs can make it easier for HIV to enter the brain and cause greater nerve cell injury and problems with thinking, learning, and memory. Drug and alcohol use can also directly damage the liver, increasing risk for chronic liver disease and cancer among those infected with HBV or HCV.