Clinical Course And Disease Progression
Acute hepatitis C virus infection is usually subclinical, and there are no reliable predictive factors for chronic infection. The relatively small size of the virus’s RNA polyprotein, rapid viral replication, and high mutation rates all contribute to the virus’s genetic heterogeneity and allow it to escape the host’s immune response, resulting in chronic infection for most patients . Progression of the disease is variable, and despite inherent limitations, histological evaluation of serial liver biopsy specimens remains the only reliable method to determine changes in severity of disease over time. On the basis of various study designs and models that predict rates of fibrosis progression, 20% to 30% of patients may be expected to develop cirrhosis over 20-30 years. This is reflected in the steady rise in the incidence of complications related to chronic liver disease, such as hepatocellular carcinoma, in many countries that are beginning to reach peak hepatitis C virus seroprevalence, such as Japan. Several host and viral factors affect disease progression, although determinants of individual risk and precise mechanisms of liver injury have yet to be determined . Better understanding of host-viral interactions may allow for targeted antiviral or other therapy aimed primarily at those at greatest risk of disease progression.
Box 2 Screening recommendations for hepatitis C virus infection
History of injecting drug use
HIV infection
Haemophilia
Hepatitis C Virus Infection
Historically, HCV infection was treated with interferon and ribavirin. Interferon-derived therapy resulted in a 50% regression in cirrhosis in the 30% who achieved a sustained virologic response . However, in those with advanced cirrhosis, only 5% saw regression of their liver disease over a 10 year period.62 Lower baseline stage of fibrosis, sustained viral response, age < 40 years, BMI < 27, and viral load < 3.5 million copies per mL were independently associated with regression of fibrosis after treatment.82
Read Also: Hepatitis B Surface Antigen Test
Do All Patients With Liver Disease Need To Have Fibrosis Testing
Fibrosis testing is relevant for the clinical care of patients with chronic liver disease, including hepatitis B, hepatitis C , non-alcoholic fatty liver disease , co-infections, primary biliary cirrhosis, primary sclerosing cholangitis, and other chronic metabolic diseases of the liver.
- Knowing the severity of fibrosis can help with prognosis and understanding the degree of liver damage.
- More rapid development of fibrosis and more advanced stages of fibrosis are more predictive of cirrhosis, and therefore liver-related illnesses and mortality.
- The severity of liver disease is a factor in determining the urgency for HCV treatment and HBV treatment.
- Understanding the fibrosis stage impacts clinical care decisions. Patients with advanced fibrosis or cirrhosis need more frequent follow up visits and labs, avoidance of some medications, and surveillance for hepatocellular carcinoma and gastroesophageal varices.
Don’t Miss: Hepatitis C Symptoms In Females
Why Are Genotypes Important For Treatment
Knowing your HCV genotype is important information that can help patients and doctors find the most effective treatment. Understanding of HCV genotype is very important it is the initial part of a treatment that can help doctors to find out most recommended effective treatment for their patients. It helps to determine patients hormones, which medicines are chosen, and how long treatment should be. Almost all the Hep C genotypes can create a serious liver problem. However, in certain cases, most of the peoples who are infected with HCV Hepatitis C genotype 1, have the higher chance of developing cirrhosis. Generally, Hep C genotype 1 and 3 can cause the risk of liver cancer. All oral and direct acting antivirals are capable enough to prevent the occurrence of Hep C virus. Today, it is mostly cured by direct-acting antivirals, medication to protect HCV easily. It allows detecting virus on the immune system and boosting your body with essential proteins. Direct acting antiviral block steps in the life cycle of virus and cure all level of genotype with the constant rate.
What Fibrosis Score Results Mean
After you have one or more tests, your doctor may tell you how much fibrosis is in your liver by telling you a âstage.â The higher the number, the more fibrosis you have. A fibrosis stage of 2 or higher means thereâs a lot of fibrosis in your liver. If your fibrosis stage is 3 or 4, your fibrosis is advanced. You have cirrhosis if your fibrosis stage is 4.
Your doctor can also use results from your FibroScan test alone or combined with other tests to figure out your fibrosis score. FibroScan fibrosis scores cover five possible stages of liver damage, from none or mild all the way to severe cirrhosis. They are broken down into these groups:
F0 to F1: No scarring in your liver, or just a little.
F2: Some scarring, between a little and a lot.
F3: A lot of scarring.
F4: Cirrhosis.
FibroScan scores are estimates, meaning the measurements are not exact. Other health problems or things you do can make your score less accurate. These include tumors in your liver, heart failure, obesity, or drinking alcohol.
Once your doctor gets your fibrosis test results, they may decide to do more tests to be sure of your diagnosis. Some fibrosis measurements also combine blood test results with a special calculator tool to figure out your risk for fibrosis. These tests are called APRI and FIB-4. But these tests can only tell if you might have fibrosis, not what stage it is.
You May Like: Pro Plan Hepatic Dog Food
Don’t Miss: Hepatic Arterial Infusion Side Effects
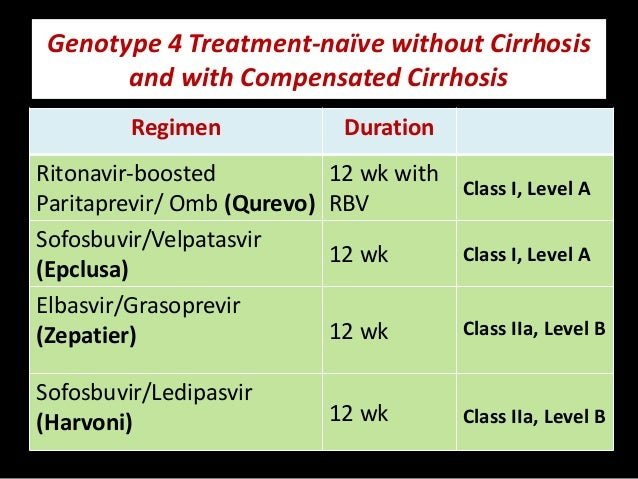
Reviewmanagement Of Hepatitis C Virus Genotype : Recommendations Of An International Expert Panel
HCV has been classified into no fewer than six major genotypes and a series of subtypes. Each HCV genotype is unique with respect to its nucleotide sequence, geographic distribution, and response to therapy. Genotypes 1, 2, and 3 are common throughout North America and Europe. HCV genotype 4 is common in the Middle East and in Africa, where it is responsible for more than 80% of HCV infections. It has recently spread to several European countries. HCV-4 is considered a major cause of chronic hepatitis, cirrhosis, hepatocellular carcinoma, and liver transplantation in these regions. Although HCV-4 is the cause of approximately 20% of the 170 million cases of chronic hepatitis C in the world, it has not been the subject of widespread research. Therefore, this document, drafted by a panel of international experts, aimed to review current knowledge on the epidemiology, natural history, clinical, histological features, and treatment of HCV-4 infections.
- Previous article in issue
How Genotypes Affect Treatment
Medications known as direct acting antivirals, or DAAs, stop the hep C virus from making copies of itself. Some DAAs appear to work well on all hepatitis C genotypes. Others work on only one or some.
Your doctor will probably prescribe some combination of these medications:
- Velpatasvir
Some pills combine two drugs into one pill.
You’ll probably take these meds for anywhere from 8 to 12 weeks. But they may not be right for everyone because of things like cost or other illnesses.
Your specific genotype can tell your doctor important things about how to use those medications, what to watch for, and other drugs you might need.
For example, you may have a higher chance for cirrhosis if you have genotype 1.
Genotype 3, the second most common subtype worldwide, may not respond as well to DAAs alone. In addition, this type might suggest that:
- Liver cancer is more likely.
- Insulin resistance might happen. When your body resists or doesn’t respond to insulin as well as normal, you have a higher chance of heart disease and diabetes.
- You might need longer, more challenging treatment
Your doctor might adjust or change your DAA treatment if you have:
Show Sources
American Association for the Study of Liver Diseases: âInitial Treatment of Adults with HCV Infection,â âHCV Guidance: Recommendations for Testing, Managing, and Treating Hepatitis C.â
CDC: âHepatitis C Questions and Answers for the Public.â
Infohep.org: âHepatitis C treatment factsheet: Harvoni .â
Recommended Reading: Early Signs Of Hepatitis C And Treatments To Know
Cost Of Drug Treatments
The newer direct-acting antiviral medicines for hepatitis C can be very expensive listed at tens of thousands of dollars.
While pricing is often negotiated by insurance companies and other agencies, the process is not especially transparent and can be confusing.
If you need help paying for medicines, speak with your doctor. For more information about available financial assistance, visit the American Liver Foundation.
Additional reporting by Deborah Shapiro.
Why Do Genotypes Matter For Treatment
Knowing your HCV genotype is important information that can help patients and doctors find the most effective treatment.
All HCV genotypes cause the same amount of liver damage. However, people infected with genotype 1, particularly subtype 1b, may have a greater chance of developing cirrhosis, or severe liver scarring, than other genotypes. Genotypes 1b and 3 may increase the risk of liver cancer.
HCV can now be cured by all oral, direct-acting antivirals , medications that prevent the hepatitis C virus from make copies of itself. DAAs do this by sticking to proteins in the virus and blocking steps in the virus life cycle. This allows your immune system to clear the virus out of your body. How well a DAA works depends on where it sticks to the target proteins in the virus.
Some of the latest DAA treatments are pangenotypic, which means they can cure all genotypes at nearly the same rates.
Also Check: How Do You Catch Hepatitis
What Is Liver Fibrosis
Your liver is one of the biggest internal organs. It has many jobs, including aiding digestion, storing energy, making blood clotting components, and removing waste and microorganisms. The liver is also able to regenerate, or regrow, itself to repair damage.
Normally, the liver can make new cells when something harms it. The new cells replace the old ones that have died. However, this does not work the way it should with a diseased liver or if liver injury is continuous or severe.
Instead, the attempts at repair cause scarring in place of functioning liver cells. Scars are fibrous tissue, hence the name fibrosis. Another name for liver fibrosis is hepatic fibrosis.
In the United States, the most common conditions that result in liver fibrosis are alcohol-related , chronic hepatitis, and nonalcoholic . Having these conditions puts you at risk of developing liver fibrosis.
Blood tests and imaging exams can help find signs of liver fibrosis. When found early, it is possible to cure or reverse liver fibrosis. If liver fibrosis remains undetected and the damage continues, it can progress to cirrhosis.
The difference between liver fibrosis and cirrhosis is that cirrhosis is permanent, irreversible scarring. The liver becomes smaller and mostly consists of hard scar tissue. Once cirrhosis develops, symptoms and problems can appear.
Factors To Consider Prior To Choosing Retreatment Regimen
For retreatment of adults with HCV genotype 3 infection, several factors influence the regimen choice, including the prior regimen used when treatment failure occurred, the presence or absence of cirrhosis, and cost or insurance considerations. It is also worth noting that the clinical data for treatment-experienced individuals with HCV genotype 3 is more limited for the newest DAAs, such as glecaprevir-pibrentasvir, since these individuals have been encountered less frequently in recent years due to the efficacy of earlier DAA regimens. Therefore, the optimal duration of therapy for retreatment of persons with HCV genotype 3 with glecaprevir-pibrentasvir is not well established. The retreatment of individuals with HCV genotype 3 who have decompensated cirrhosis, renal impairment, acute HCV, or post-liver transplantation is not addressed in this lesson.
Read Also: Can Hepatitis B Be Cured Totally
Also Check: Hepatitis B Viral Load Quantitative
Background In Hcv Treatment
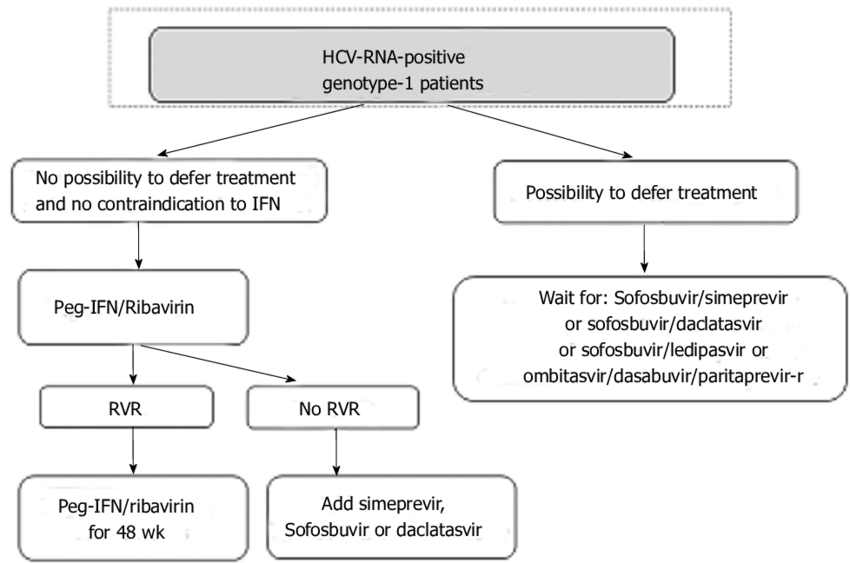
At the start of the millennium, two major advances in the management of HCV took place: one, the approval by the FDA of PEG-IFN for the treatment of HCV infection, which allowed weekly subcutaneous injections instead of the previous daily or thrice weekly injections with standard IFN and the use of weight-based RBV. By the mid-2000s, it was established that PEG-IFN-2a or PEG-IFN-2b could be combined with weight-based RBV for GT-1 infected patients, or with flat-dosed RBV for GT-2 or GT-3 infected patients, and that combination was better than treatment with standard IFN and RBV. HCV-GT-4 response to treatment with PEG-IFN/RBV has been considered better than GT-1, and worse than GT-2 and GT-3.
With the introduction of the HCV-GT-1 effective protease inhibitors boceprevir and telaprevir in 2011, HCV-GT-4 became the most difficult to treat, as both protease inhibitors are not indicated for treatment of GT-4. Many studies used 48 wk duration of combined therapy to treat HCV-GT-4, and a few of them compared responses between 24-wk treatment and 48-wk treatment response rates. Figures and summarize the results of those studies after using standard-dose PEG-IFN and RBV. The results show sustained virologic response rates with 24 wk of therapy to be far less than rates with 48-wk, making the longer duration the standard of care.
Evaluation Of Fibrosis Progression Rate
The 378 patients contributed 558 pairs of consecutive biopsies. Fibrosis progression by 1 stage was detected in 203 consecutive biopsies and progression by 2 or 3 stages was observed in 47 consecutive biopsies . We used a multistate Markov model to estimate the progression rates between different fibrosis stages, after accounting for possible misclassification in the assessment of liver fibrosis, based on the observed transition frequencies . The estimated progression rate from stage 0 to stage 1 was the highest, and it was 3.08 times higher than the progression rate from stage 1 to stage 2. The progression rate from stage 2 to stage 3 was the lowest. The estimated sojourn time was the shortest for fibrosis stage 0 and the longest for fibrosis stage 2 . This explains the lower estimated probability for transition from stage 0 to stage 1 after 10 years . Additionally, we conducted a subgroup analysis on the patients who underwent > 2 biopsies. The estimated fibrosis progression rates were 0.34 between stages 0 and 1, 0.09 between stages 1 and 2, 0.07 between stages 2 and 3, and 0.10 between stages 3 and 4 and are consistent with the data obtained on the overall data set.
Probability of remaining at the same fibrosis stage 2, 5, and 10 years after the initial fibrosis assessment.
You May Like: Can Hepatitis B Be Cured With Antibiotics
How To Prevent Cirrhosis
The best way to prevent alcohol-related cirrhosis is to drink within the recommended limits.
The guidelines recommend:
- men and women should not regularly drink more than 14 units of alcohol a week
- you should spread your drinking over 3 days, or more, if you drink as much as 14 units a week
Stop drinking alcohol immediately if you have alcohol-related cirrhosis. Drinking alcohol speeds up the rate at which cirrhosis progresses, regardless of the cause.
A GP can offer help and advice if youâre finding it difficult to cut down the amount you drink.
What Are Hepatitis C Genotypes
A variable for those with chronic hepatitis C virus is the genotype, or the strain of the virus when they contracted an infection. The genotype is determined by a blood test.
The genotype doesnt necessarily play a role in progression of the virus, but rather as a factor in selecting the right medications for treating it.
According to the
Also Check: Treatment For Liver Cirrhosis Hepatitis B
Whats The Difference Between Hepatitis C Genotypes
As mentioned, the different HCV genotypes and subtypes have different distributions throughout the world.
Genotype 1 is the most common HCV genotype in the United States. Its found in nearly 75 percent of all HCV infections in the country.
Most of the remaining people in the United States with HCV infection carry genotypes 2 or 3.
The HCV genotype isnt absolutely related to the rate of liver damage, or the likelihood of eventually developing cirrhosis. However, it can help predict the outcome of treatment.
The genotype can help predict the outcome of anti-HCV therapy with interferon-based treatment regimens. Genotype has also helped to determine treatment.
In some formulations, the recommended doses of ribavirin and pegylated interferon are for people with specific HCV genotypes.
Disease Progression In Chronic Hepatitis C: Modifiable And Nonmodifiable Factors
- E. Jenny HeathcoteCorrespondenceAddress requests for reprints to: E. Jenny Heathcote, MD, FRCPC, Fell Wing, 6B-154, University Health Network, The Toronto Western Hospital, 399 Bathurst Street, Toronto, Ontario, M5T 2S8 Canada. fax: 603-6281.
Abbreviations used in this paper:
J Viral Hepat.Clin Liver Dis.A Spanish multicentre experience, Eur J Gastroenterol Hepatol.
- Delarocque-Astagneau E.
|
|
Donât Miss: What To Do If You Have Hepatitis C
Read Also: If You Have Hepatitis B Do You Have Hiv
Indications For Liver Biopsy
Prior to the development of widely used noninvasive tests that estimate hepatic fibrosis, such as aspartate aminotransferase-to-platelet ratio index , FibroSure, FibroTest, and transient elastography , liver biopsy was used to estimate liver fibrosis. Traditionally, the primary reasons for doing a liver biopsy have been to provide information on fibrosis stage which can help guide therapeutic HCV management decisions, diagnose coexisting liver diseases, and help identify cirrhosis that would necessitate routine cancer surveillance. In the current era, liver biopsy is used less frequently. The following outlines certain circumstances that may warrant consideration of liver biopsy when evaluating a person with chronic HCV.
- Two indirect markers show discordant results. For example, when an APRI score is in the 0.5 to 1.5 range and the FibroSure/FibroTest is less than 0.48, then a liver biopsy is warranted to determine the presence or absence of advanced fibrosis/cirrhosis and the need for routine hepatocellular cancer surveillance and follow-up.
- There is a second cause of liver disease is suspected.
- Indirect, direct, and transient elastography tests are unavailable, or not advisable for specific reasons.