Hepatitis B Causes And Risk Factors
Itâs caused by the hepatitis B virus, and it can spread from person to person in certain ways. You can spread the hepatitis B virus even if you donât feel sick.
The most common ways to get hepatitis B include:
- Sex. You can get it if you have unprotected sex with someone who has it and your partnerâs blood, saliva, semen, or vaginal secretions enter your body.
- Sharing needles. The virus spreads easily via needles and syringes contaminated with infected blood.
- Accidental needle sticks.Health care workers and anyone else who comes in contact with human blood can get it this way.
- Mother to child.Pregnant women with hepatitis B can pass it to their babies during childbirth. But thereâs a vaccine to prevent newborns from becoming infected.
Hepatitis B doesnât spread through kissing, food or water, shared utensils, coughing or sneezing, or through touch.
What Causes Hepatitis B
The hepatitis B virus causes hepatitis B. The hepatitis B virus spreads through contact with an infected persons blood, semen, or other body fluids. Contact can occur by
- being born to a mother with hepatitis B
- having unprotected sex with an infected person
- sharing drug needles or other drug materials with an infected person
- getting an accidental stick with a needle that was used on an infected person
- being tattooed or pierced with tools that were used on an infected person and werent properly sterilized, or cleaned in a way that destroys all viruses and other microbes
- having contact with the blood or open sores of an infected person
- using an infected persons razor, toothbrush, or nail clippers
You cant get hepatitis B from
- being coughed on or sneezed on by an infected person
- drinking unclean water or untreated water that has not been boiled
- eating food that is unclean or has not been properly cooked
- hugging an infected person
- shaking hands or holding hands with an infected person
- sharing spoons, forks, and other eating utensils
- sitting next to an infected person
Mothers who have hepatitis B can safely breastfeed their babies. If a baby receives hepatitis B immune globulin and starts receiving the hepatitis B vaccine to prevent hepatitis B infection shortly after birth, hepatitis B is unlikely to spread from mother to child through breastfeeding.15
How Can I Prevent Spreading Hepatitis B To Others
If you have hepatitis B, follow the steps above to avoid spreading the infection. Your sex partners should get a hepatitis B test and, if they arent infected, get the hepatitis B vaccine. You can protect others from getting infected by telling your doctor, dentist, and other health care professionals that you have hepatitis B. Dont donate blood or blood products, semen, organs, or tissue.
You May Like: Hepatitis C And Liver Cirrhosis
What Is The Treatment For Hepatitis B
Prevention is recommended by receiving a vaccine for HBV.
Receiving an injection of the hepatitis B immune globulin within 12 hours of coming in contact with the virus may help prevent the development of the disease.
At present, there is no specific treatment for patients with acute hepatitis B. Acute infection is usually short and will often resolve on its own. Your health care provider may recommend rest, and adequate nutrition and fluids to help your body fight the infection. Hospitalization may be required for patients who suffer from severe vomiting and who are unable to maintain adequate nutritional levels. It may also be required to prevent the development of complications.
While chronic infection cannot be cured, there are two standard treatments in Canada that may control the virus and prevent further damage to the liver.
- Antiviral medications can fight the virus and slow damage to the liver.
- Interferon which may be given for short periods and if effective, results in suppression of the virus.
What Occupations Have Increased Risk Of Hepatitis B
In general, occupational groups with increased risk include:
- Health-care workers repeatedly exposed to blood or blood products or those who are at risk of needlestick injury.
- Pathologists, laboratory personnel, or embalmers.
- Dentists, dental assistants, and dental hygienists.
- Certain staff members of institutions for the developmentally handicapped.
- Staff of institutions where workers may be exposed to aggressive, biting residents.
Travellers to regions with intermediate or high rates of endemic HBV infection may also consider being vaccinated.
You May Like: Difference Between Hepatitis B And C
What Other Problems Can Hepatitis B Cause
In rare cases, acute hepatitis B can cause liver failure.
Chronic hepatitis B can develop into a serious disease that causes long-term health problems such as cirrhosis , liver cancer, and liver failure.
If you have ever had hepatitis B, the virus may become active again, or reactivated, later in life. This could start to damage the liver and cause symptoms.
What Are The Types Of Hepatitis B
There are two types of hepatitis B infection: acute and chronic.
Acute
An acute infection happens at the beginning, when you first get infected with hepatitis B. Many people are able to clear it from their bodies and recover. In fact, this is true of about 4 in 5 adults who are infected.
Chronic
If you are not able to clear the infection within six months or longer, you have chronic hepatitis B. It is chronic hepatitis B that leads to inflammation and the serious, and possibly fatal, illnesses of cirrhosis of the liver and liver cancer. Treatment can slow disease progress, reduce the chance of liver cancer and increase your chances of surviving.
Recommended Reading: Hepatitis A And B Shot
Hbv Transmission To And From Health Care Workers
In the past, the risk of acquiring an HBV infection by performing exposure-prone procedures was so high that after several decades of professional activity the majority of health care workers showed markers of previous or ongoing HBV infection. Thus, many physicians became victims of their professional activities, were highly infectious HBV carriers and thereafter a threat for the patients on whom they performed exposure prone procedures. Since the 1970s, there have been numerous reports on HBV transmissions from health care workers with high viremia to patients, usually during surgery. Most critical were thorax, gynecological and oral surgery. The medical community was sluggish to draw the necessary consequences. Initially, the supervising authorities recommended only that HBV carriers should wear double gloves while doing surgery and be particularly cautious.
Medical Impact Of The Vaccine
Taiwan was the first country to begin with universal childhood vaccination in 1984. At that time, the rate of perinatal transmission was extremely high leading to a nation-wide HBsAg carrier rate of ca. 10%. Twenty years later only 1.2% of those borne after beginning of the vaccination campaign were HBsAg carriers. Although HCC is mainly a disease of advancing years, the impact of the vaccination quickly became apparent in children and adolescents because its incidence dropped significantly from 0.57 to 0.17 in 100,000 person years in that age group after the beginning of mass vaccination. Thus, the hepatitis B vaccine was the first successful vaccine against a specific form of cancer . Similar observations were reported from other parts in the world. In low prevalence countries like Italy the vaccination has probably contributed to a very strong decrease of hepatitis B incidence.
Observations in Taiwan and Thailand or in high risk groups of other countries suggest that the protection becomes weaker within 20 years but the immune memory is good enough to mitigate the infection in the ca. 23% of those infected. Those with no or with low anti-HBs are still protected against HBV disease but they get a clinically silent infection with transient HBs antigenemia, or anti-HBc seroconversion or increase of the anti-HBs titer. The necessity or timing of later booster injections is a matter of debate.
Also Check: What Does It Mean To Have Antibodies For Hepatitis C
Hepatitis B Facts And Figures
Hepatitis B is a global public health threat and the worlds most common serious liver infection. It is up to 100 times more infectious than the HIV/AIDS virus. It also is the primary cause of liver cancer , which is the second-leading cause of cancer deaths in the world.
Hepatitis B Around the World
- Two billion people have been infected with the hepatitis B virus .
- Approximately 1.5 million people become newly infected each year.
- Almost 300 million people are chronically infected.
- Approximately 10% of infected individuals are diagnosed.
- An estimated 820,000 people die each year from hepatitis B and related complications such as liver cancer.¹
- Approximately two people die each minute from hepatitis B.
Hepatitis B In the United States
1. In 2019, there were approximately 820 000 people who died from hepatitis B-related causes globally: Web Annex 1. Key data at a glance. In: Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021. Accountability for the global health sector strategies 20162021: actions for impact. Geneva: World Health Organization 2021. License: CC BY-NC-SA 3.0 IGO.
How Do You Know If You Have Hepatitis B
Signs and symptoms can vary, in particular by the age of the individual. Many individuals may not show symptoms . When symptoms develop, they include fever, joint pain, abdominal pain, fatigue, lack of appetite, nausea, vomiting, dark urine, clay-coloured bowel movements, or jaundice.
Most infections are asymptomatic or mild. Occasionally, people with serious cases of hepatitis B require hospitalization. A very small proportion of these patients develop a critical form of the disease called “fulminant” hepatitis B. This condition results from a sudden breakdown of liver function.
Recommended Reading: Royal Canin Hepatic Dry Dog Food
Indication For Interferon Therapy
After 36 years of experience, interferon alpha still has its place in HBV therapy, but the patients need to be carefully selected, because interferon has many severe side effects and contra-indications, and only a minority will show a sustained response. Interferon suppresses HBV replication but the exact mechanism is not known and today more dependable chemical antivirals with less side effects are available. The main advantage of interferon is that it can enhance the bodys own immune defense, and accelerate the sustained resolution of the infection. Thus, patients with active inflammation, i.e. elevated transaminsases, and partially successful immune control are the best candidates for this strenuous therapy. The cccDNA form of the HBV genome is probably as stable as the host chromosome and can currently not be attacked by any available drug. However, interferon may induce innate defense mechanisms e.g. the RNA editing cytidine deaminase APOBEC3G, which may damage the HBV pregenome, or it may enhance apoptosis of infected cells. Accelerated hepatic cell turnover in absence of HBV replication will decrease HBV cccDNA to innocuous levels. Long-term follow-up has confirmed that patients with a sustained viral response regain a normal life expectancy .
The Impact Of Worldwide Hepatitis B Vaccination Programs: Model Of Success
A, Immunization coverage with third dose of hepatitis B in infants in 2019. B, Global immunization 19892019 HepB3 coverage in infants. Global coverage was 84% in 2019. Abbreviations: AFR,African region AMR,Americas region EMR,Eastern Mediterranean region EUR,European region SEAR,South-East Asia region WPR,Western Pacific region. Source: United Nations Children’s Fund /World Health Organization.
The success of HBV vaccination programs has been clearly demonstrated over the recent years in several regions around the world. Countries that have adopted the recommendation had a marked reduction in carrier rates as well as complications from HBV, including HCC. The low prevalence of chronic HBV infection in children younger than 5 years, reducing from 4.7% in the prevaccine era to less than 1% in 2019, can be attributed to the widespread use of hepatitis B vaccine. Due to the implementation of routinely birth-dose vaccination the greatest decrease appears to be in the Western Pacific region, from 8.3% HBsAg prevalence in the prevaccine era to 0.93% in 20022015 . Among health care workers, hepatitis B vaccination is highly effective for the prevention of healthcare associated HBV infection and chronic infection. Using mathematical models, it was estimated that since their implementation, HBV vaccination programs have averted 210 million new HBV infections globally .
Recommended Reading: What Is The Meaning Of Hepatitis
Quantitative Measurement Of Hbv Dna
The assays for HBV infectivity described above were indispensable for HBV research but are too expensive and laborious for the laboratory diagnosis of HB viremia. The best surrogate test is the sensitive and quantitative determination of the number of HBV DNA molecules in plasma or serum. In the early days, the endogenous DNA polymerase reaction developed by Robinson was the first feasible but relatively insensitive and laborious assay. Later this was replaced by various techniques of nucleic acid hybridization using cloned HBV DNA as labeled probes. These techniques were still of insufficient sensitivity and accuracy and could not detect the low viremia of healthy HBsAg carriers or occult HBV infections. They were, however, useful for distinction of high and low infectivity and for HBV monitoring in early therapy studies.
Who Strategy For Hepatitis B Immunization
Although major progress has been achieved in hepatitis B immunization, a number of challenges remain. That is why the WHO called for comprehensive prevention and control of HBV infection and the development of time-specific immunization goals in its member states. The strategy includes the following: universal vaccination of infants within 24 hours of birth, full immunization of infants by routine immunization programs, catch-up vaccination of unimmunized cohorts, and monitoring progress and assessing the impact of immunization .
Universal Vaccination of Infants Within 24 Hours of Birth: a Real Challenge
Full Immunization of Infants by Routine Immunization Programs and Catch-Up Vaccination of Unimmunized Cohorts
Wider provision of the existing, safe and effective HBV vaccine, through universal childhood vaccination and by catch-up vaccination of unimmunized cohorts, will further reduce new hepatitis B infections, reducing rates of chronic illness and death. However, to achieve and/or sustain high coverage, stronger and resilient immunization delivery systems will be needed. Still, some countries adopt risk-grouptargeted vaccination only, instead of adding a universal vaccination program. However, changing demography, increasing immigration, and the current vaccine costs make the cost-benefit ratios in these remaining low-endemicity countries strongly in favor of universal HBV vaccination.
Monitoring Progress and Assessing the Impact of Immunization
Recommended Reading: What Is The Blood Test For Hepatitis C
Discovery Of The Dane Particle
AuAg, however, was not a prion-like agent. While inspecting AuAg immune complexes under the EM in 1970, David S. Dane discovered that AuAg appeared not only on the small pleomorphic particles, but also on larger, virus-like objects 42nm in size with a clearly visible inner core . Shortly thereafter, in 1971, his British colleague June Almeida was able to release the core particles from the so-called Dane particles by treatment with mild detergent, and showed by immune EM that hepatitis B patients formed antibodies against this core antigen . This strongly suggested that the Dane particles were the actual virus causing hepatitis B. AuAg was obviously the surface antigen of the virus envelope, and was named HBsAg thereafter. The infected hepatocyte forms the HBsAg protein in large surplus and secretes it in addition to the complete virus as round or filamentous noninfectious particles of about 20nm in diameter into the blood leading to an approximately three-thousand fold excess of these subviral particles . This was the reason that the Dane particles could not be recognized in AuAg preparations purified by ultracentrifugation or size chromatography.
Figure 1
Electron microscopy images and approximate numbers of HBV associated particles in 1 ml of the serum from a highly viremic chronically infected HBV carrier.
What Are The Risk Factors For Getting Hepatitis B
Due to the way that hepatitis B spreads, people most at risk for getting infected include:
- Children whose mothers have been infected with hepatitis B.
- Children who have been adopted from countries with high rates of hepatitis B infection.
- People who have unprotected sex and/or have been diagnosed with a sexually transmitted infection.
- People who live with or work in an institutional setting, such as prisons or group homes.
- Healthcare providers and first responders.
- People who share needles or syringes.
- People who live in close quarters with a person with chronic hepatitis B infection.
- People who are on dialysis.
Don’t Miss: Hepatitis C Flu Like Symptoms
You Can Have It And Not Know It
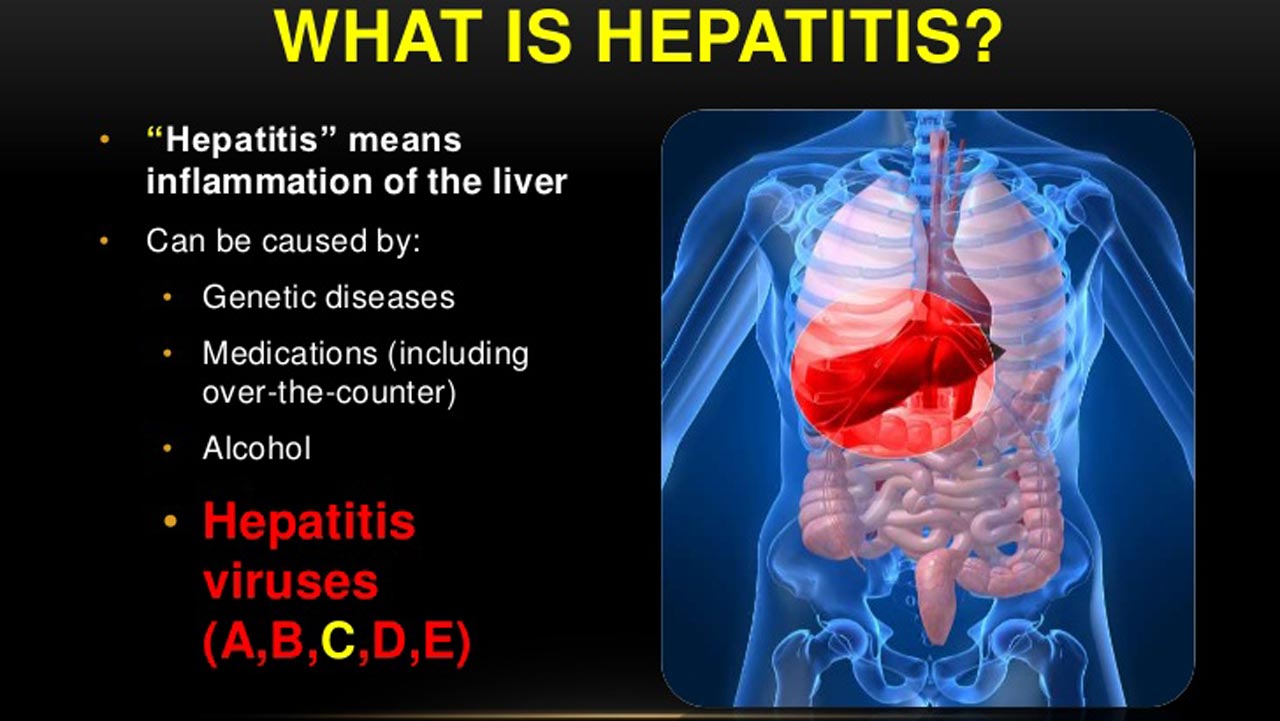
What is hepatitis B?
Hepatitis B is a liver disease caused by the hepatitis B virus . HBV is far more infectious than HIV and can be prevented by a vaccine. People who have not been vaccinated may be at risk of getting infected.
About 95 percent of adults will recover within 6 months of becoming infected and as a result will develop lifelong protection against it. The remaining 5 percent are unable to clear the virus and will become chronically infected. Chronic hepatitis B infection is treatable.
It is estimated that less than 1 percent of Canada’s population is infected with either acute or chronic HBV. People who are infected before the age of 7 are at a higher risk of developing chronic infection. In 2011, the overall reported rate of acute hepatitis B infection in Canada was 0.6 reported cases per 100,000 people living in Canada.
Why is hepatitis B a health concern?
Many people infected with HBV do not know they have the virus because symptoms can take two to six months to appear and only about 50 percent of people develop symptoms. During this time, they can spread the infection to others. You may not know you have this infection until damage has already been done to your liver. Potential complications from chronic HBV infection include cirrhosis of the liver, liver failure, liver cancer and premature death.
Why do I need my liver?
How is hepatitis B spread?
HBV is spread through contact with infected blood and body fluids including semen and vaginal fluid.
Transmission Symptoms And Treatment
How is HBV transmitted?
HBV is transmitted through activities that involve percutaneous or mucosal contact with infectious blood or body fluids , including
- sex with a partner who has HBV infection
- injection drug use that involves sharing needles, syringes, or drug-preparation equipment
- birth to a person who has HBV infection
- contact with blood from or open sores on a person who has HBV infection
- exposures to needle sticks or sharp instruments and
- sharing certain items with a person who has HBV infection that can break the skin or mucous membranes , potentially resulting in exposure to blood.
How long does HBV survive outside the body?
HBV can survive outside the body and remains infectious for at least 7 days .
What should be used to clean environmental surfaces potentially contaminated with HBV?
Any blood spills should be disinfected using a 1:10 dilution of one part household bleach to 9 parts water. Gloves should be worn when cleaning up any blood spills.
Who is at risk for HBV infection?
The following populations are at increased risk for becoming infected with HBV:
- Infants born to people with HBV infection
- Sex partners of people with HBV infection
- Men who have sex with men
- People who inject drugs
- Household contacts or sexual partners of known people with chronic HBV infection
- Health care and public safety workers at risk for occupational exposure to blood or blood-contaminated body fluids
- Patients on hemodialysis
Who should be screened for HBV?
Read Also: How Can You Cure Hepatitis C