The Development Of Guidelines: Rigour Of Development/systematic Critical Review Of The Literature
1.2.1 Guideline development group
The development of these clinical guidelines follows a workshop held at the Royal College of Physicians on 3 December 1997. This meeting was jointly coordinated by the NHS Executive, the Royal College of Physicians, the British Society of Gastroenterology, British Liver Trust, and the British Association for the Study of the Liver . The workshop was attended by hepatologists, gastroenterologists, histopathologists, virologists, general practitioners, clinical nurse specialists, patient representatives, health care economists, and NHS managers. Attendants were chosen to represent key professional disciplines and interest groups likely to be affected by the guidelines. The literature was reviewed by a clinician attending the workshop and the guidelines written under the guidance of a steering committee, which met regularly during the development process. The document was circulated to both clinicians and non-clinicians for comments before the final guidelines were drawn up . The guidelines were presented at the 1999 BASL meeting in London where consensus was achieved on some of the more controversial issues.
1.2.2 Strategy
- ARCTs, meta-analyses, or systematic reviews
- Bprospective, retrospective, or cross sectional studies
- Cexpert opinion.
1.2.3 Context and content
1.2.4 Application and presentation
The national guidelines will be used as a framework for local groups to develop according to local needs.
1.2.5 Statement of intent
What Are The Names Of The Medications For Treating Hepatitis C
Since 2014, multiple different antiviral treatments for hepatitis C have been developed. With the many options now available, often there is more than one good choice for a patient. Some of the treatments are recommended as first-line options, some are second-line options, and others are used less commonly in light of all the available choices.
- Elbasvir/Grazoprevir
Second line hepatitis C medications:
- Sofosbuvir/Velpatasvir/Voxelaprevir
The Polymerase Chain Reaction
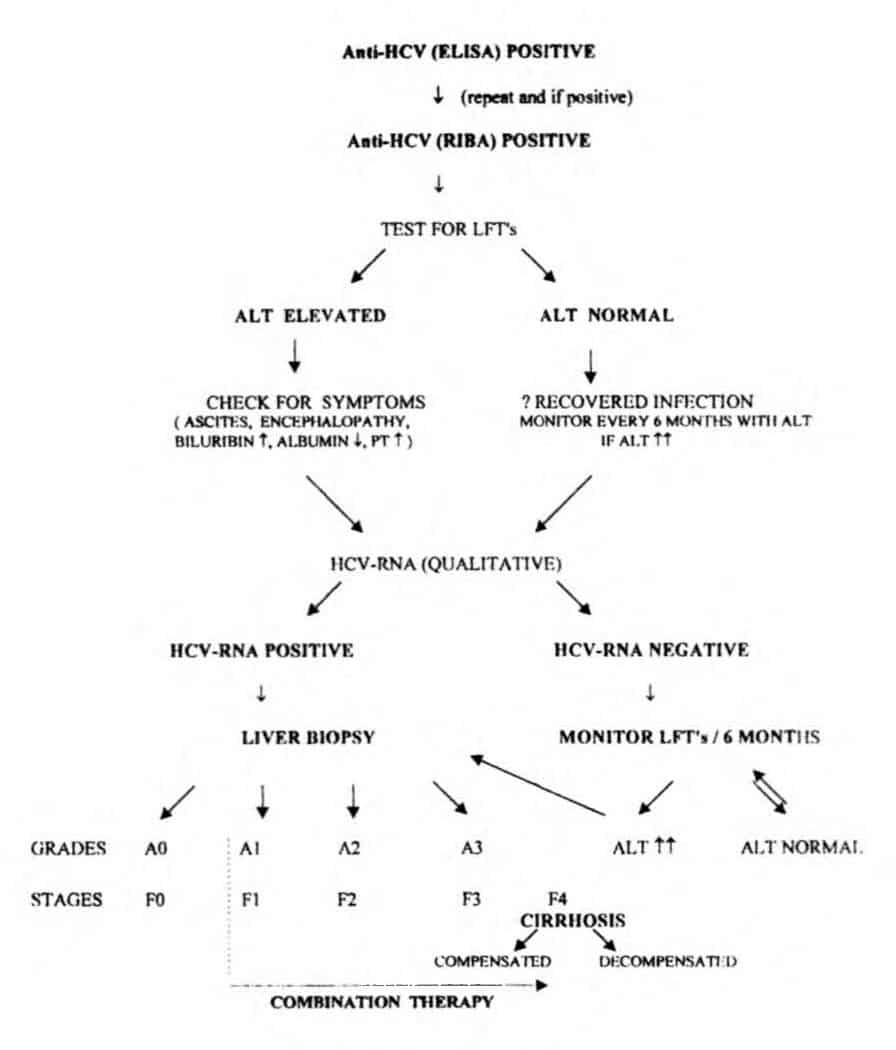
Initial PCR for HCV detection used primers derived from heterogeneous non-structural regions of the virus. The development of primers from the highly conserved 5 non-coding region greatly enhanced the detection of HCV RNA by PCR. The sensitivity of PCR detection was further enhanced by the development of PCR primers producing shorter PCR products. The sensitivities of most PCR assays is in the range of 5001000 equivalents per ml.
Direct detection of the virus using PCR is needed in patients recently infected with the virus and in immunosuppressed individuals who may be antibody negative. In addition, PCR is useful for determining the status of patients with indeterminate antibody profiles and for monitoring antiviral therapies. The sensitivities and specificities of the commercially available PCR tests are very high. Intermittent viraemia is unusual in patients untreated with IFN so enhancing the significance of a negative PCR result.
You May Like: Disease Caused By Hepatitis B
Hepatitis C And Health
How can health-care personnel avoid exposure to HCV?
Avoiding occupational exposure to blood is the primary way to prevent transmission of bloodborne illnesses among health-care personnel. To promote blood safety in the workplace, health-care personnel should consult infectious-disease control guidance from the National Institute for Occupational Safety and Health and from CDC. Depending on the medical procedure involved, Standard Precautions may include the appropriate use of personal protective equipment .
What is the risk of acquiring hepatitis C after being accidentally exposed to HCV-contaminated blood or body fluids in the workplace?
Although sharps injuries have decreased in recent decades due to improved prevention measures, they continue to occur, placing health-care personnel at risk for several bloodborne pathogens like hepatitis C. A recent analysis of several studies revealed an overall 0.2% risk for infection among those exposed to HCV-antibody-positive blood through needlestick or sharps injuries . Updated guidelines for management and treatment of hepatitis Cexternal icon are available to provide guidance for health-care personnel who become infected via exposure to contaminated blood at the workplace.
Other than needlesticks, do other exposures place health-care personnel at risk for hepatitis C?
Should HCV-infected health-care personnel be restricted in their work?
What Are The Symptoms Of Hepatitis C
Most people infected with hepatitis C have no symptoms. Some people with an acute hepatitis C infection may have symptoms within 1 to 3 months after they are exposed to the virus. These symptoms may include
- yellowish eyes and skin, called jaundice
If you have chronic hepatitis C, you most likely will have no symptoms until complications develop, which could be decades after you were infected. For this reason, hepatitis C screening is important, even if you have no symptoms.
Dont Miss: Hepatitis B Virus Symptoms And Treatment
Don’t Miss: What’s The Difference Between Hepatitis B And Hepatitis C
Treatment Of Hepatitis C In The Future New Models Of Care
Treatment of hepatitis C currently occurs in specialist liver clinics, typically within tertiary hospitals. This system is very effective and necessary to manage the complexities of interferon-based treatment. However, capacity is limited. Patients with advanced fibrosis and cirrhosis will need to remain in the tertiary system for management of their liver disease. However, patients who do not have cirrhosis may not need to be managed in a specialist clinic if they can be treated with simple interferon-free regimens. This will allow new models of care involving GPs, nurse practitioners, opioid-substitution therapy clinics and the custodial system. The PBAC has recommended that newer hepatitis C therapies are listed on the general schedule to promote treatment in primary care.
Pregnancy And Hepatitis C
The new hepatitis C medicines have not been tested in pregnancy.
You should not become pregnant while taking treatment as it could be harmful to unborn babies.
If you’re pregnant, you must delay treatment until after your baby is born.
Speak to your doctor before starting hepatitis C treatment if you’re planning to become pregnant in the near future.
You’ll need to wait several weeks after treatment has ended before trying to get pregnant.
Women taking ribavirin should use contraception during treatment and for another 4 months after the end of treatment.
If you become pregnant during treatment, speak to your doctor as soon as possible to discuss your treatment options.
Read Also: Life Insurance For Hepatitis B Carrier
Transmission Of Hepatitis C
- HCV is most commonly transmitted through contact with blood, for example
- sharing needles, syringes or other equipment for injecting drugs among people who inject drugs
- reusing inadequately sterilised medical equipment
- transfusion of unscreened blood and blood products
- occupational exposure to blood or body fluid with HCV in healthcare setting
Box : Global Eradication Of Hcv A Realistic Goal
An estimated 160 million people worldwide are infected with hepatitis C virus with widely varying prevalence among countries. Upcoming combination regimens hold the promise of being able to cure almost any individual patient regardless of the HCV genotype that they are infected with .
One may wonder whether global eradication of HCV might or even should be a realistic goal. The absence of significant non-human reservoirs and the availability of a protective vaccine or at least highly effective treatment are regarded as some of the key preconditions for the eradication of an infectious disease. Pathogens such as smallpox, measles and rubella fulfil these criteria, and indeed smallpox was declared eradicated in 1980 following a major global public health effort. Despite this success, only two other diseases have been formally declared targets for eradication by the World Health Organization : dracunculiasis in 1986 and poliomyelitis in 1988 . As yet neither goal has been achieved, reflecting the enormity of the challenge to achieve complete global eradication even if the above-mentioned preconditions are met. Nevertheless, there are worthwhile goals below the high bar of global eradication for instance, the WHO aims to eliminate measles and rubella in at least five of the six WHO regions by 2020 .
Read Also: Is There Medication For Hepatitis B
Box : Hcv Treatment Terminology
Below is a list of the important terminology used to describe treatment of patients chronically infected with hepatitis C virus and the response to the treatment.
Below is a list of the important terminology used to describe treatment of patients chronically infected with hepatitis C virus and the response to the treatment.
Lead-in phase. The phase in which a limited range of compounds is used to treat patients before giving the actual full combination of compounds. For example, in boceprevir-based triple therapy and ribavirin) there is generally a 4-week lead-in treatment phase with PEG-IFN and ribavirin before boceprevir is introduced.
Rapid virological response . When a patient is HCV RNA negative after 4 weeks of treatment.
Extended rapid virological response: telaprevir ). When a patient is HCV RNA negative between 4 weeks and 12 weeks of treatment with telaprevir.
Extended rapid virological response: boceprevir ). When a patient is HCV RNA negative between 8 weeks and 24 weeks of treatment with boceprevir.
Early virological response . When a patient has 2 log decline in HCV RNA at week 12 of the treatment regimen.
Partial early virological response . When a patient has a 2 log decline in HCV RNA but is not HCV RNA negative at week 12 of the treatment regimen.
Complete early virological response . When a patient is HCV RNA negative at week 12 of the treatment regimen.
Null response. When a patient has a < 2 log decline of HCV RNA at week 12 of the treatment regimen.
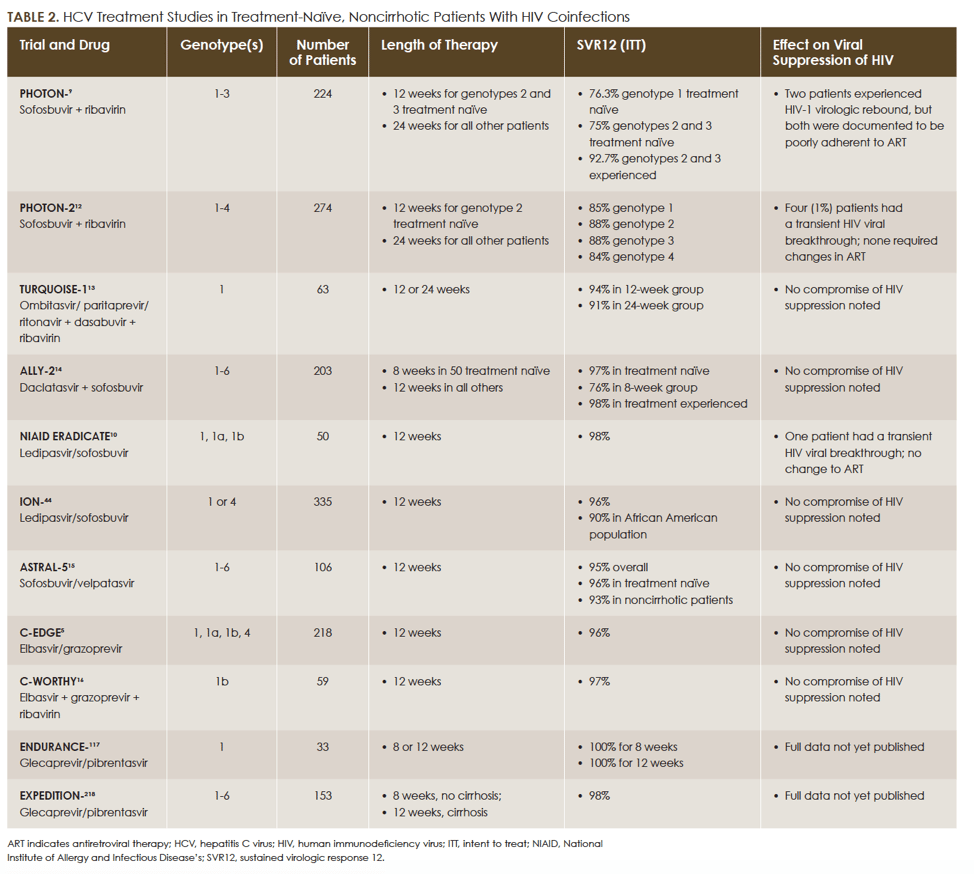
Approach To Choosing Hcv Genotype 1 Treatment Regimen
For individuals with chronic HCV genotype 1 infection, the main factors that influence the choice and duration of therapy are cirrhosis status and prior treatment experience. With the use of certain regimens for persons with HCV genotype 1a, namely elbasvir-grazoprevir, the genotype 1 subtype also impacts the choice of therapy, as elbasvir-grazoprevir is only recommended for persons with HCV genotype 1a who do not have baseline NS5A resistance-associated substitutions . In addition, the HCV RNA level and the patients HIV status can impact the duration of ledipasvir-sofosbuvir, but does not affect the duration of other regimens. Finally, the cost of the regimen, insurance coverage, and provider preference can play a major role in the regimen choice. The following treatment recommendations are based on the AASLD-IDSA HCV Guidance for initial treatment of adults with HCV genotype 1 and for retreatment of adults in whom prior therapy failed, including those with HCV genotype 1.
Also Check: Blood Test For Hiv And Hepatitis
Treatment Of Hepatitis C
- Currently, direct-acting antivirals are first-line drugs of hepatitis C treatment.
- Highly effective
- Oral administration
- Treatment usually takes around 8 – 12 weeks
- Minor side effects
Sustained virological response is an indicator of treatment success. A sustained virological response occurs when the blood test shows no detectable RNA in 12 weeks after treatment. People having achieved SVR after treatment are considered as cured, and will not transmit the virus to others.
How Effective Is Treatment
Direct-acting antivirals cure 9 out of 10 patients with hepatitis C.
Successful treatment does not give you any protection against another hepatitis C infection. You can still catch it again.
There’s no vaccine for hepatitis C.
If treatment does not work, it may be repeated, extended, or a different combination of medicines may be tried.
Your doctor or nurse will be able to advise you.
You May Like: Hepatitis A Is It Curable
Monitoring Counseling And Nonpharmacologic Considerations
Stringent monitoring of treatment efficacy, AEs, medication adherence, and DDIs is recommended for all patients undergoing antiviral therapy for HCV. Four weeks after therapy initiation, CBC, LFTs, and serum creatinine should be assessed. Quantitative tests for HCV RNA are recommended at weeks 4 and 12 and may be considered at week 24 .9 Thyroid-stimulating hormone levels should be evaluated at the beginning and end of therapy if IFN-based treatment is administered. If ribavirin is being considered in women of childbearing age, a serum pregnancy test prior to treatment initiation is recommended.
Prior to therapy initiation, patients should be extensively educated regarding their HCV medications, monitoring plan, and reduction of transmission or reinfection. Patients should be cautioned to avoid the use of alcohol, which can lead to further liver decompensation, including progression of cirrhosis or development of end-stage liver disease.28 Once therapy has started, patients should be monitored by telephone or in person for medication adherence. Patients should be counseled to report any new prescription or OTC medications to assess for new DDIs during therapy or the potential for new medications to cause hepatotoxicity. Other nonpharmacologic considerations include vaccination for hepatitis A and hepatitis B in susceptible patients.9
What Is The Impact Of Hepatitis C
- 58 million people have hepatitis C
- 75% of people with hepatitis C live in low- and middle-income countries
- About 50% of all people with hepatitis C live in 4 countries: China, Pakistan, India, and Egypt
- 79% are unaware they are infected
- only 13% have had access to treatment
- 2.3 million people have both HIV and hepatitis C
- 1530% of those chronically infected develop cirrhosis of the liver within 20 years
- 800 people die every day
Hepatitis C is found throughout the world. There are six different major strains of hepatitis C, known as genotypes, distributed across different regions, with genotype 1 being most prevalent in high-income countries and genotype 3 most prevalent in low- and middle-income countries. Genotype 3 accounts for 30% of global hepatitis C infection.
Don’t Miss: Human Hepatic Stellate Cell Line
Helpful Tips While Taking Hepatitis C Medications
- Always follow your health care providers’ advice, particularly the instructions on taking your medicine.
- If you have to cancel an appointment, call your provider and schedule a new one as soon as possible.
- Take good care of yourself. Eat well, drink 8 to 10 glasses of water each day, and try to get a full night’s sleep.
- Learn about the hepatitis C medications you are taking. This includes special risks and warnings.
- If taking ribavirin, use sunscreen, wear long sleeves and a hat, and limit sun exposure.
- Write down your doctor’s name and phone number. Carry this information with you at all times.
- Write the names and amounts of the medicines you are taking. Carry this information with you at all times.
Drugs And Combinations Under Development
There is fierce ongoing competition to bring drugs to the market that will replace PEG-IFN, ribavirin and/or the first-generation protease inhibitors . As of May 2013, over 1,600 studies evaluating drugs for the treatment of hepatitis C are listed on the ClinicalTrials.gov website. These trials are investigating a multitude of compounds in different patient populations or subpopulations. There is widespread agreement that no single agent will achieve cure of chronic HCV infection in the foreseeable future. Thus, the rapidly shifting landscape is made even more complex by the many combinations that are being evaluated.
Figure 4: Selection of anti-HCV drugs in advanced development.
A schematic of drugs approved for treating hepatitis C virus infection as well as drugs in advanced development with tentative future launch dates. PEG-IFN, peglyated-interferon r, ritonavir.
In the following sections we discuss the different classes of anti-HCV drugs under development, their general advantages and limitations, as well as a selection of current key compounds. Many novel DAAs are being developed both as combinations with PEG-IFN plus ribavirin and as part of all-oral regimens.
Don’t Miss: What Does Hepatitis C Non Reactive Mean
Similar Articles Being Viewed By Others
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
27 August 2019
Gregory C. Fanning, Fabien Zoulim, Antonio Bertoletti
20 October 2020
Ohad Etzion, Harel Dahari, Amir Shlomai
12 October 2021
Man-Fung Yuen, Jeong Heo, T. Jesse Kwoh
17 May 2018
volume 12, pages 595610
How Will My Provider Monitor Me During The Treatment
Your provider will meet with you during treatment to review how well you are tolerating treatment and review laboratory results. Laboratory tests help keep tabs on your health, track the viral load, and determine your response to treatment. You will be given specific dates to go get your blood tested at the lab during and after the treatment.
Don’t Miss: Hepatica Herbal Liquid Extract Supplement
Studies Of Initial Treatment Of Adults With Hcv Genotype 1
The following summarizes key studies that support the recommendations in the AASLD-IDSA HCV Guidance for initial treatment of patients with chronic hepatitis C and genotype 1 infection, including those without cirrhosis and those with compensated cirrhosis the medication regimens are listed in alphabetical order.
Box : Hcv And Host Diversity
Genetic variation in both the hepatitis C virus and its human host affect the natural history of the infection and the degree of response by patients to treatment.
As a small RNA virus with an error-prone RNA polymerase HCV exhibits enormous genetic variability. Viral isolates have been grouped into six major genotypes that differ in 3035% of nucleotides across the genome,. Genotypes are further divided into subtypes that differ by 2025% of nucleotides across the genome,. Even within an infected host HCV exists as a heterogeneous population of related variants often referred to as a quasispecies swarm. The predominance of HCV genotypes varies among geographical regions with genotype 1 dominating in Europe and the Americas followed by genotypes 2 and 3 . HCV genotypes are clinically relevant, as genotypes 1 and 4 are less responsive to interferon-based therapy than genotypes 2 and 3. Moreover, subgenotype 1a is associated with a more rapid emergence of resistant-associated variants under treatment with HCV NS3/4A protease inhibitors compared with subgenotype 1b . Finally, patients infected with genotype 3 are more likely to develop hepatic steatosis, progress more rapidly to hepatic fibrosis and are at a higher risk of developing hepatocellular carcinomas,.
Don’t Miss: Hepatitis B In Blood Test