Specific Hcv Rna Assays And Range Of Detectable Virus
HCV RNA tests use target amplification techniques. Several assays exist for HCV RNA testing. Methods include polymerase chain reaction , transcription mediated amplification , and branched chain DNA tests. Results are expressed as international units/mL . The different methods and different commercial assays each have a lower limit of quantification and lower limit of detection , therefore a patient’s results could be reported differently depending on the assay used. HCV RNA tests must have an LLOQ of 25 IU/mL or lower when used to assess treatment response with DAAs.
LLOQ = the lowest HCV RNA level that is within the linear and analytically acceptable range of the assay.
LLOD = the lowest level of HCV RNA that is detected 95% of the time.
Common Hepatitis C Terms
Hep C is considered an acute condition if caught early enough. According to the CDC, early enough is less than six months after becoming infected with the hep C virus.1
But, in most cases, hep C isnt caught within that six-month window, and it turns into a chronic infection. Theres another added layer to this, however, because you can live with chronic hep C for months or years without knowing.
So, a chronic hep C infection can also cause chronic liver disease. That means youd have more than one chronic health condition until your hep C is cured.
Symptoms And Signs Of Acute Hepatitis C
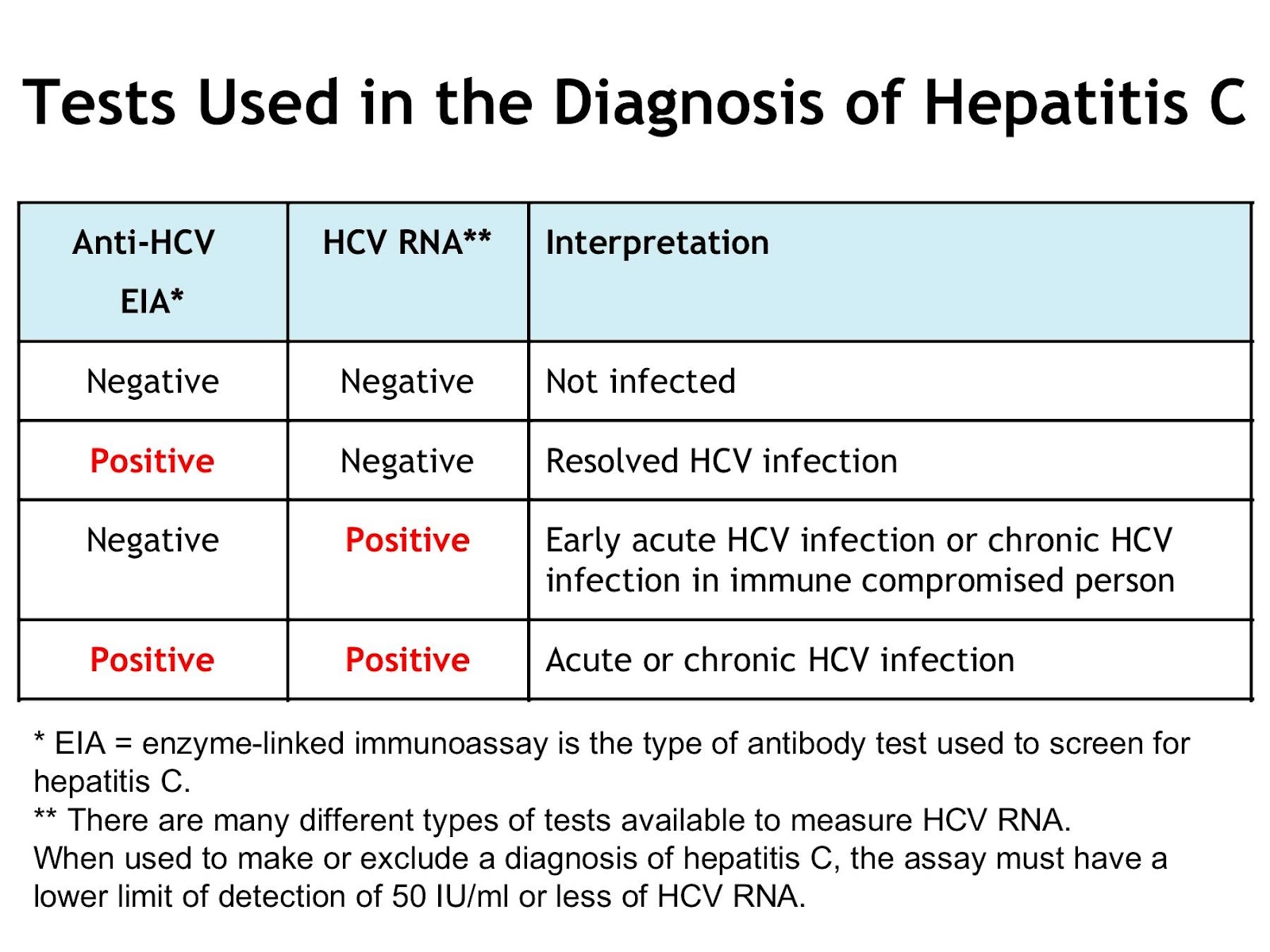
If the anti-HCV test is positive, HCV RNA is measured to distinguish active from past hepatitis C infection .
In hepatitis C, serum anti-HCV represents chronic, past, or acute infection the antibody is not protective. When cases are unclear or when suspicion for hepatitis C is high, HCV RNA is measured. Anti-HCV usually appears within 2 weeks of acute infection but is sometimes delayed however, HCV RNA is positive sooner.
Also Check: How Does Someone Get Hepatitis
Acute Hepatitis B Infection
If you are newly infected with hepatitis B, your infection is considered acute. An acute hepatitis B infection may last up to six months and you may pass the virus to others during this time.
Your doctor will order follow up testing to determine whether you have successfully gotten rid of the virus. Until your health care provider confirms that the blood test shows that there is no more hepatitis B virus in your blood, it is important to protect others from a possible infection.
Hepatitis B can be spread to others through blood and bodily fluids. If your sexual partner and household members are not vaccinated, they should be tested for hepatitis B. If they have not been infected then they should also start the hepatitis B vaccine series. You should use condoms for all sexual activity, wash hands after any potential exposure to blood, and avoid sharing sharp objects such as razors, nail clippers, earrings, and toothbrushes.
Most people experience only mild symptoms or none at all. Symptoms may appear 60-150 days after infection, with the average being 90 days. The majority of acute infections are treated by rest and managing symptoms.
Most common symptoms include:
Rarely, people may experience severe symptoms such as:
- Nausea
- Jaundice
- Bloated stomach
A rare, life-threatening condition called fulminant hepatitis can occur with a new acute infection and requires immediate, urgent medical attention since a person can go into sudden liver failure.
What Use Of These Terms Means For Your Health
Broadly speaking, acute conditions occur suddenly, have immediate or rapidly developing symptoms, and are limited in their duration . Chronic conditions, on the other hand, are long-lasting. They develop and potentially worsen over time .
These descriptions can vary somewhat, though, depending on who you speak to or what sources you reference. While the terms may apply in specific circumstances, they don’t always, and they often fall short in describing what you may be faced with if given an acute or chronic diagnosis.
Read Also: How Do You Contract Hepatitis A
Symptoms Of Hepatitis C
Each patient with hepatitis C is important to us at Health Services of North Texas. Symptoms can be subtle, but over time, the hepatitis C virus can destruct and damage the liver. Some of the most commons symptoms that your body is fighting the hepatitis C virus are:
-
Pain in the abdomen, usually the upper right side
-
Jaundice in the whites of eyes and skin
-
Fatigue
Acute Vs Chronic Hepatitis C: What Is The Difference
When you have hepatitis C, a manageable viral disease, our professional team at Health Services of North Texas can help. Our health centers have an experienced infectious disease management team that offers confidential hepatitis C treatment. Our goal is to help our patients live a healthy and active life, regardless of whether or not they have hepatitis C. Hepatitis C is a disease that is primarily contracted through the blood. Regardless of how someone contracted hepatitis C, there is hope and, in most of the cases we see, the possibility of a cure with medication. Our team can help you understand the differences between acute hepatitis c vs. chronic hepatitis c and how each is treated effectively.
Read Also: Can Hepatitis C Be Transferred Sexually
Meaning Of Hcv Viral Load
The number of HCV RNA international units per milliliter of blood must be measured before treatment and during the course of treatment, to assess response. Before treatment, however, the HCV viral load is not related to the patient’s liver disease severity or HCV prognosis. This is important for patients and providers to understand.
Note: In hepatitis B, unlike hepatitis C, a higher HBV DNA viral load does correlate with increased disease severity and increased likelihood of outcomes such as hepatocellular carcinoma.
Relationship Of Symptoms And Spontaneous Clearance
Overall, when combining data from multiple historical studies, approximately 25 to 35% of person with acute HCV infection have spontaneous clearance of HCV. The rates of spontaneous clearance are significantly lower in persons who are Black and in those individuals who have HIV coinfection. In contrast, rates of spontaneous clear are higher in females and in persons who acquired HCV in childhood. It has also been demonstrated that patients who present with symptomatic acute HCV infection and jaundice have higher rates of spontaneous clearance of HCV, in the range of 35 to 50%. The presence of jaundice is believed to reflect hepatic inflammation caused by a more robust initial immune response against HCV.
You May Like: Types Of Hepatitis B Virus
Acute Vs Chronic Hepatitis B
A hepatitis B infection can result in either an acute infection or a chronic infection. When a person is first infected with the hepatitis B virus, it is called an “acute infection” . Most healthy adults that are infected do not have any symptoms and are able to get rid of the virus without any problems. Some adults are unable to get rid of the virus after six months and they are diagnosed as having a “chronic infection.” A simple blood test can diagnose an acute or chronic hepatitis B infection.
The risk of developing a chronic hepatitis B infection is directly related to the age at which a person is first exposed to the hepatitis B virus. The younger a person is when they are first infected, the greater the risk of developing a chronic hepatitis B infection:
- More than 90% of infants that are infected will develop a chronic hepatitis B infection
- Up to 50% of young children between 1 and 5 years who are infected will develop a chronic hepatitis B infection
- 5-10% of healthy adults 19 years and older who are infected will develop a chronic hepatitis B infection
The recommendation for hepatitis B vaccination of babies and children is so important because they are at the greatest risk of developing a chronic infection if they are not protected against the hepatitis B virus as soon as possible.
Laboratory Studies For Evaluation Of Initial Infection
The key laboratory studies utilized in the evaluation of possible acute hepatitis C are HCV RNA, anti-HCV, and alanine aminotransferase . Patients who become infected with hepatitis C virus typically develop abnormal laboratory findings in the following order: detectable HCV RNA, followed by elevation in ALT, and then anti-HCV . Patients who develop a clinical illness with acute HCV infection usually have onset of symptoms well after the onset of viremia, but soon after or concomitant with increases in ALT levels.
HCV RNA
Antibodies to HCV
Antibodies to HCV typically become detectable at about 50 to 60 days after infection the detection of HCV-specific antibodies significantly lags behind detectable HCV RNA levels. After 12 weeks, more than 90% of patients will have a positive HCV antibody test. The time period from initial infection until seroconversion is often referred to as the serologic window period . The use of only an HCV antibody test to diagnose acute HCV is not reliable, since only approximately 50 to 70% of patients have detectable HCV antibodies at the onset of symptoms. Further, a positive HCV antibody test does not differentiate acute from chronic HCV infection.
Hepatitis C Core Antigen
Alanine Aminotransferase
Don’t Miss: How Can Someone Contract Hepatitis C
Difference Between Acute And Chronic Hepatitis C
Hepatitis is a medical condition of the liver, characterized by inflammation of the liver which might possibly result in scarring, fibrosis, Cirrhosis and hepatic malignancies. There are 5 major entities of the virus, responsible for causing Hepatitis known as Hepatitis A, B, C, D and E. This article discusses,
1. What is Acute Hepatitis C Cause, Signs and Symptoms, Diagnosis and Treatment
2. What is Chronic Hepatitis C Cause, Signs and Symptoms, Diagnosis and Treatment
3. Difference Between Acute and Chronic Hepatitis C
Hepatitis C Virus Infection
Steatosis is a hallmark of genotype 3 HCV liver injury. Studies directly comparing genotype-specific injuries are rare, although genotype differences have been studied in the setting of definite hepatic steatosis and non-alcoholic steatohepatitis . Gene expression profiling has identified genotype 3-specific genes SOCS1 and IFITM1, and genotype 1-specific genes CCL3, CCL4, IFNAR, and PRKRIR . Importantly, fibrotic injury did not have a genotype-specific signature . Unique HCV-associated fibrosis signatures have been identified and have led to the correlation of the corresponding proteins of three of these genes inter- inhibitor H1, serpin peptidase inhibitor clade F member 2, and transthyretin being correlated with stages of fibrosis development . Clearly, such proteins may well be useful biomarkers of HCV fibrosis development in the future.
Grzegorz W. Telega, in, 2018
Recommended Reading: What Does Hepatitis Feel Like
Recommendations For Medical Management And Monitoring Of Acute Hcv Infection
RECOMMENDED RATING After the initial diagnosis of acute HCV with viremia , HCV treatment should be initiated without awaiting spontaneous resolution. I, B Counseling is recommended for patients with acute HCV infection to avoid hepatotoxic insults, including hepatotoxic drugs and alcohol consumption, and to reduce the risk of HCV transmission to others. I, C Referral to an addiction medicine specialist is recommended for patients with acute HCV infection related to substance use. I, B
Patients with acute HCV infection should be treated upon initial diagnosis without awaiting spontaneous resolution, using a test and treat strategy and according to the simplified approach, if eligible. Real-world data have demonstrated a reduction in HCV viremia prevalence and incidence with unrestricted access to HCV therapy . In addition, mathematical modeling suggests that DAA treatment scale-up, especially among those at highest risk of transmission, can reduce HCV incidence and prevalence . Moreover, delay introduced by waiting for spontaneous clearance may be associated with loss to follow up.
There is no need to alter concomitant medications that are metabolized by hepatic enzymes unless there is concern for developing acute liver failure . Acetaminophen and alcohol consumption should be avoided during acute HCV infection .
Recommended Regimens For Patients With Acute Hcv Infection
RECOMMENDED RATING Owing to high efficacy and safety, the same regimens that are recommended for chronic HCV infection are recommended for acute infection. IIa, C
A number of studies have evaluated DAA treatment of acute HCV infection. Small single-arm, uncontrolled studies have evaluated 6 or 8 weeks of ledipasvir/sofosbuvir. One such study demonstrated 100% SVR with 8 weeks of ledipasvir/sofosbuvir among 27 men with acute HCV and HIV-coinfection . Investigators conducting another study evaluated 6 weeks of ledipasvir/sofosbuvir in a similar cohort . Among participants with genotype 1 infection, 79% achieved SVR12 71% of those with genotype 4 infection achieved SVR12 with this shortened regimen. Among the 6 individuals whose treatment did not lead to SVR12, there were 3 relapses . Three participants achieved SVR4 but were lost to follow-up . A phase 2 study followed a similar treatment protocol among 20 individuals with genotype 1 HCV monoinfection, all of whom achieved SVR12 .
An open-label, single-arm, multicenter pilot study evaluated the efficacy of 6 weeks of the pangenotypic regimen glecaprevir/pibrentasvir among persons with acute/recent HCV infection . SVR12 was 90% a single virological failure occurred in a man with genotype 1a, HIV coinfection, and a viral load of 7.7 log10 IU/mL. This patient was successfully retreated .
- Related References
- Additional Reading
Recommended Reading: Most Common Symptoms Of Hepatitis C
Terminology Related To Acute Hcv Infection
Clinical reviews and research studies have used numerous terms to refer to acute hepatitis C infection, including acute infection, acute phase infection, very early infection, recent infection, and newly acquired infection. Overall, consensus does not exist regarding the terminology and criteria for defining acute HCV infection. Very early infection typically refers to patients with a positive HCV RNA and documented HCV antibody seroconversion, with this scenario being the most definitive for diagnosing acute HCV infection. Some experts have suggested limiting the multiple possible terms to acute infection and recent infection with the following definitions:
- Acute Infection: estimated duration of infection less than 6 months
- Recent Infection: estimated duration of infection longer than 6 months, but shorter than 2 years.
Where Definitions Fall Short
As tidy as the definitions may seemsix months or more for chronic versus less than six months for acutethese timeframes in no way suggest what you may be faced with if diagnosed with an acute or chronic illness.
After all, an acute bout of the flu does not compare to an acute hepatitis C infection. Neither does HIV compare to multiple sclerosis .
In the end, labeling an illness as acute or chronic cannot describe the nature of a disease, nor predict outcomes.
This non-specificity of definitions not only affects healthcare providers and patients but also researchers who look for concise ways to evaluate the course of a disease. Thresholds are frequently changed from six months to three months or extended to a year or more, which only adds to confusion.
Even pubic health authorities aren’t immune to these discrepancies. The U.S. Department of Health and Human Services , for instance, lists 20 diseases as chronic including stroke, autism, and cancerwhile the Centers for Medicare and Medicaid Services lists 19, many of which are different from the HHS list.
Within this context, the definition can often bend to fit the situation. With the HHS, chronic is used to describe a public health concern for surveillance purposes. With the CMMS, the term broadly describes a disease for healthcare utilization purposes.
Read Also: Hepatitis B And C Can Be Spread By
Pathophysiology And Natural History
There are six known genotypes of HCV. The most common genotypes in the United States, comprising 97% of all U.S. HCV infections, are 1 , 2, and 3.9
The mechanism of hepatocyte damage induced by HCV infection is not completely understood but may involve direct cell injury and a local immune-mediated mechanism that causes a chronic inflammatory state.10,11 Acute HCV infection progresses to chronic disease in 50% to 80% of patients and clears spontaneously in 20% to 50% of patients.10 Of persons with chronic disease, 20% will develop cirrhosis, end-stage liver disease, and/or hepatocellular carcinoma.12
Figure 1 illustrates the natural history of HCV infection.10
Figure 1.
Natural history of hepatitis C virus infection.
Reprinted with permission from Pawlotsky JM. Pathophysiology of hepatitis C virus infection and related liver disease. Trends Microbiol. 2004 12:97.
Figure 1.
Natural history of hepatitis C virus infection.
Reprinted with permission from Pawlotsky JM. Pathophysiology of hepatitis C virus infection and related liver disease. Trends Microbiol. 2004 12:97.
Recommended Testing For Diagnosing Acute Hcv Infection
RECOMMENDED RATING HCV antibody and HCV RNA testing are recommended when acute HCV infection is suspected due to exposure, clinical presentation, or elevated aminotransferase levels . I, C
Recommendations for HCV testing are also found in the Testing and Linkage to Care section.
Diagnosis of acute HCV infection enables estimation of annual incidence rates and transmission patterns, thereby facilitating implementation and assessment of prevention programs. At the individual level, a diagnosis of acute infection expedites linkage to care, counseling regarding high-risk behavior, and timely interventions to reduce virus transmission and liver disease progression . Some persons involved in high-risk behaviors practice serosorting, defined as using HCV antibody serostatus to determine whether to engage in high-risk behaviors with certain individuals . Thus, undiagnosed acutely infected persons may be at greater risk of transmitting HCV to their presumably seronegative contacts than would be expected by chance.
The best laboratory evidence to support a diagnosis of acute HCV infection is a positive HCV RNA test in the setting of a negative HCV antibody test , or a positive HCV antibody test after a prior negative HCV antibody test . There are rare instances in which these approaches may be misleading, such as in immunosuppressed individuals with impaired antibody production .
Discrete Exposure
No Discrete Exposure
Also Check: July 28 World Hepatitis Day
Cdc Case Definition For Acute Hcv
The Centers for Disease Control and Prevention has established criteria for the 2020 case definition of acute Hepatitis C. This definition utilizes clinical criteria, laboratory criteria for diagnosis, criteria to distinguish a new case from an existing case, and a case classification . The following summarizes the 2020 CDC Case Definition for Acute HCV.