What Is A Degenerative Disease Of The Liver Characterized By Scarring
Serosis is a chronic degenerative liver condition marked by scarring. The scars may be visible on the surface of the liver or may only be detectable under the skin, in other words, subclinical. They cant be cured but they can be treated.
The most common cause of serous liver disease is alcohol consumption. Other causes include taking certain medications, such as phenacetin , acetaminophen , chloramphenicol , and methotrexate having autoimmune disorders such as primary biliary cirrhosis or primary sclerosing cholangitis and genetic conditions such as Hereditary Hemorrhagic Telangiectasia . HHT is a rare genetic disorder that affects the blood vessels, causing them to develop an abnormal number of holes. This disease can lead to liver cancer if not treated.
Liver disease is a major concern for people who drink alcohol regularly because alcohol affects both healthy and diseased livers in similar ways. It can cause severe damage to healthy liver tissue, leading to cirrhosis.
About Article Author
Ashley Shields
Ashley Shields has been in the health industry for over 10 years. She has worked as an intern for both hospitals and medical schools, gaining experience in every aspect of medicine and health. She loves to share her knowledge of health with others through blogging or speaking at conferences, where she can share what shes learned during her time in the field.
Disclaimer
Overview Of Liver Structure
At the cellular level, portal triads consist of adjacent and parallel terminal branches of bile ducts, portal veins, and hepatic arteries that border the hepatocytes. Terminal branches of the hepatic veins are in the center of hepatic lobules. Blood flows from the portal triads past the hepatocytes and drains via vein branches in the center of the lobule, rendering the center of the lobule the area most susceptible to ischemia.
Overview Of Bilirubin Metabolism
The breakdown of hemoglobin produces bilirubin and other bile pigments. Bilirubin must be made water soluble to be excreted. This transformation occurs in 5 steps: formation, plasma transport, liver uptake, conjugation, and biliary excretion.
Formation: About 250 to 350 mg of unconjugated bilirubin forms daily 70 to 80% derives from the breakdown of degenerating red blood cells, and 20 to 30% derives primarily from other heme proteins in the bone marrow and liver. Hemoglobin is degraded to iron and biliverdin, which is converted to bilirubin.
Plasma transport: Unconjugated bilirubin is not water soluble and so is transported in the plasma bound to albumin. It cannot pass through the glomerular membrane into the urine. Albumin binding weakens under certain conditions , and some substances compete for the binding sites.
Liver uptake: The liver takes up bilirubin rapidly but does not take up the attached serum albumin.
Conjugation: Unconjugated bilirubin in the liver is conjugated to form mainly bilirubin diglucuronide . This reaction, catalyzed by the microsomal enzyme glucuronyl transferase, renders the bilirubin water soluble.
Biliary excretion: Tiny canaliculi formed by adjacent hepatocytes progressively coalesce into ductules, interlobular bile ducts, and larger hepatic ducts. Outside the porta hepatis, the main hepatic duct joins the cystic duct from the gallbladder to form the common bile duct, which drains into the duodenum at the ampulla of Vater.
Also Check: What Is Hepatitis B Symptoms
Eat Fruits And Veggies
Eating an abundance of fruits and veggies is vital for protecting your liver from fatty liver progression and worsening liver conditions. Fruits and vegetables are chock-full of protective components like antioxidants, vitamins, and minerals. Antioxidants like polyphenols and carotenoids actually help the liver clear oxidative waste and repair from damage. Incorporate foods like beets, spinach, carrots, celery, sweet potato, apples, and berries into your diet.
Normal Range Of The Liver Stiffness Values And Influence Of Age And Gender
The liver stiffness values in living liver donors ranged from 1.54 to 2.87 kPa, and the mean liver stiffness values measured using three methods were as follows: 2.052 kPa with the 2cm-per-slice method 2.014 kPa with the 1cm-S method and 2.119 kPa using the 70% S method. The liver stiffness value measured using the 70% S method was significantly higher than that of the 2cm-per-slice or of the 1cm-S method . Liver stiffness values measured using the 2cm-per-slice and the 1cm-S method did not differ significantly. The mean liver stiffness values with a 95% confidence interval according to the gender and age groups are summarized in Table . There was no significant difference in liver the stiffness value between the genders or among the age groups in all three measurement methods.
| Gender |
|---|
Bland-Altman plots show the reproducibility and repeatability of the three, different, liver stiffness value measurement methods, i.e., the reproducibility of the 2cm-per-slice method , the 1cm-S method , and the 70% S method and the repeatability of the 2cm-per-slice method , the 1cm-S method, and the 70% S method . The X-axes show the means of the liver stiffness values measured using 3 different methods, and the Y-axes show the differences between the liver stiffness values as a percentage of their mean. Solid lines = mean absolute differences. Dashed lines = 95% limits of agreement.
Read Also: Where Can I Get My Hepatitis B Vaccine
Vascular And Biliary Architecture
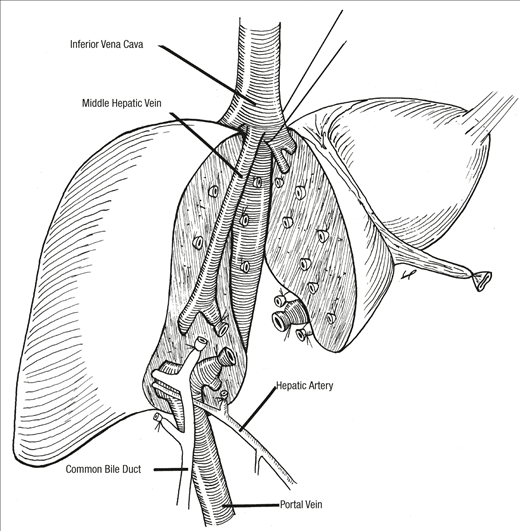
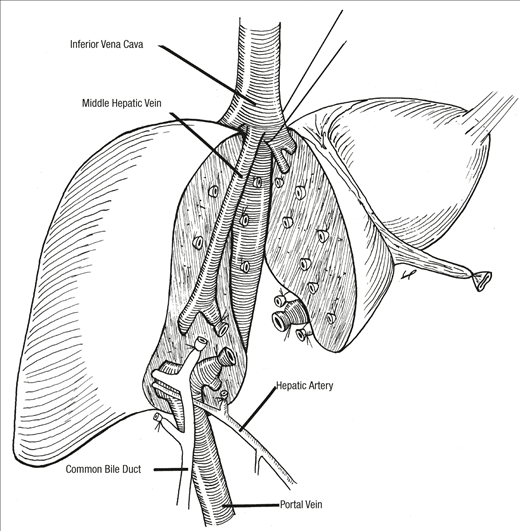
The generally smooth liver parenchyma is traversed by several vascular structures: the portal veins, hepatic veins, hepatic arteries and the bile ducts. The liver is unique in receiving two blood supplies: the hepatic artery provides approximately 25% of the inflow at rest, in the form of oxygenated blood direct from the systemic arterial system the portal vein provides partially deoxygenated blood via the bowel, spleen and other viscera. Both pass through the porta hepatis, along with the bile duct. Venous drainage occurs via the hepatic veins, directly into the upper inferior vena cava to the right atrium of the heart .
The common hepatic artery is normally a branch of the coeliac axis, and divides into left and right branches at or somewhere before the porta hepatis. In around 50% of people variations in its origin occur,3 including separate left and right supplies from the coeliac axis and superior mesenteric artery , or common supply from the SMA alone. Identification of these vessels is important in preoperative assessment of liver transplant recipients. The diameter of the normal common hepatic artery is 5 mm or less. On ultrasound images, the artery is roughly parallel with the portal vein at the porta, but is more tortuous, and is seen coming in and out of the scan plane.
C.J. YOON, J.W. CHUNG, in, 2007
Hepatic Fibrosis And Cirrhosis
CLDs are characterized by ongoing inflammation and fibrosis. Chronic inflammation leads to potentially reversible early hepatic fibrosis and when untreated progresses to cirrhosis with the cross-linking of collagen fibres and the formation of regenerative nodules.34 Regression of hepatic fibrosis can occur, with significant reduction in fibrosis burden, especially when treatment is started early. Hepatitis C can be cured with new antiviral drugs and lifestyle changes can significantly reduce hepatic steatosis. Non-invasive detection and staging of hepatic fibrosis is important in the management of chronic liver diseases.
Recommended Reading: Blood Test Results For Hepatitis
Fate Of Fatty Acids In The Liver
In the fasting state, adipocyte TAG is hydrolyzed to release FFAs, which are transported to the liver where they can serve as substrates for mitochondrial -oxidation. -oxidation of fatty acids is a major source of energy needed to maintain liver viability during fasting. It is also the source of the ketone bodies, acetoacetate and acetone. These are released into the blood and are essential fuel sources for peripheral tissues, when glucose is in short supply. Defects in hepatic -oxidation cause microvesicular steatosis of the liver, increase in oxidative stress due to extramitochondrial oxidative stress. ROS and peroxidation products lead to cytotoxic events, release of proinflammatory cytokines and activation of hepatic stellate cells and fibrosis.
Dont Miss: Is Hepatitis C An Sti
What Is A Progressive Degenerative Disease Of The Liver
Cirrhosis is a chronic liver condition that worsens with time. The two main types of cirrhosis are caused by alcohol abuse or infection with the bacteria Hepatitis C or B. Other factors such as autoimmune diseases, medications, and toxins can also lead to cirrhosis.
Alcoholism is a common cause of cirrhosis in people aged 30 to 60. Alcohol causes scarring of the liver, which prevents it from working properly. With time, this repeated injury leads to more severe scarring and eventually cancer.
Hepatitis is an inflammation of the liver caused by certain viruses or bacteria. There are several types of hepatitis, but most can be divided into two categories: acute and chronic. Acute hepatitis usually goes away on its own after causing the body to produce antibodies against the virus or bacteria that caused it. Chronic hepatitis does not go away over time instead, it results in permanent damage to the liver. This can lead to cirrhosis, cancer, or need for a transplant.
Cirrhosis can be diagnosed based on the results of a physical examination and laboratory tests. Diagnostic tools include blood tests, imaging scans, and endoscopy.
Also Check: How Do I Know I Have Hepatitis B
Don’t Miss: Hepatitis B And Fatty Liver
Spectral Ct Examination And Quantitative Indices Measurement
Quadruple-phase contrast enhanced CT was performed14â16. All patients were scanned with spectral imaging mode with scanning parameters as follows: fast switch tube voltage 80/140 kVp, automatic tube current from 100 to 600 mA with noise index set as 9, 8 cm detector, slice thickness of 5 mm, rotation speed of 0.5 s, helical pitch of 0.992:1, and 40% Asir. Nonionic contrast media were injected through antecubital vein at a rate of 5 mL/sec, with a total volume of 80â120 mL . Hepatic arterial phase imaging was determined by automatic scan triggering software when trigger attenuation threshold reached the level of supraceliac abdominal aorta, while portal venous and equilibrium phase was initiated at 45 and 120 s after AP phase, respectively. All raw data were reconstructed with 2.5 -mm-thick slices. Then, monochromatic images at 70 keV, water- and iodine-based material decomposition images were analyzed. All post-processions were performed in Advanced Workstation .
Iodine density measurement
Regions of interest measurement of quantitative indices. Multiple ROIs were placed in liver parenchyma , aorta and portal vein in arterial phase and venous phase , with average area about 100 mm2, respectively. The averages were calculated as the iodine density.
Liver volume measurement
Other Tests To Confirm Fatty Liver Disease
An ultrasound examination isnt the only tool used when diagnosing fatty liver disease. Numerous other tests can confirm the presence of fat within the liver.
- Other imaging tests: Magnetic resonance imaging and computed tomography scans can also evaluate the fat content in liver cells and evaluate the health of the parenchymal liver, which is liver tissue that carries out biological functions.
- Liver biopsy: A liver biopsy requires taking a small sample from your liver and having it analyzed for abnormalities. A liver biopsy is one of the most accurate methods of diagnosing fatty liver disease.
- Liver enzymes test: A blood test can reveal the levels of liver enzymes, particularly aspartate aminotransferase and alanine aminotransferase . High levels of transferases in the blood indicate liver inflammation thats consistent with fatty liver disease.
- Palpation: A physician may manually detect enlargement of the liver, which signifies inflammation in the liver. If your liver is larger than a normal liver size, this is a good sign that you have liver inflammation or fat buildup in liver cells.
Don’t Miss: Hepatitis C-positive Organ Transplant
Evaluation Of Liver Histology
All liver tissue samples were at least 1cm3 surgical hepatic specimens from the right hepatic lobe. Those specimens were fixed in formalin and embedded in paraffin, and 4-μm-thick sections were stained with hematoxylin and eosin . All pathologic slides were evaluated by an experienced hepatopathologist âblinded to clinical information and imaging findingsâwith regard to degree of fibrosis, inflammation, and hepatic steatosis. The degree of hepatic steatosis was also classified into four semiquantitative groups: that is, normal is less than 5%, mild is between 5% and 29%, moderate is between 30% and 59%, and severe is if more than 60% of the hepatocytes have fat vacuoles within the cytoplasm.
What Are The Forms Of Fatty Liver Disease
There are two main forms of fatty liver disease:
Alcohol-induced fatty liver disease
Alcohol-induced fatty liver disease is caused by heavy drinking. About 5% of people in the U.S. have this form of liver disease.
Non-alcohol related fatty liver disease
Non-alcohol related fatty liver disease occurs in people who arent heavy drinkers. The condition affects one in three adults and one in 10 children in the United States. Researchers havent found the exact cause of non-alcohol related fatty liver disease. Several factors, such as obesity and diabetes, can increase your risk.
Also Check: How To Order Hepatitis B Titer
Steatosis And Fibrosis Progression In Hcv
High levels of TNF- have also been observed in human chronic hepatitis C patients. TNF- has been shown to induce IR in experimental animals and cultured cells. Inhibition of tyrosine phosphorylation of IRS 1 and 2 may be one of the mechanisms by which a high level of TNF- causes IR. Administration of an anti-TNF- antibody restores insulin sensitivity. These results provide direct experimental evidence for the contribution of HCV in the development of IR. There are experimental arguments for a direct role of insulin in fibrosis progression in HCV infection.
Epidemiological studies indicating that the state of IR now associated with NASH is also associated with an increased risk of HCC. It is worth mentioning that diabetes increases the risk of chronic liver disease and HCC.
What Gets Stored In A Cookie
This site stores nothing other than an automatically generated session ID in the cookie no other information is captured.
In general, only the information that you provide, or the choices you make while visiting a web site, can be stored in a cookie. For example, the site cannot determine your email name unless you choose to type it. Allowing a website to create a cookie does not give that or any other site access to the rest of your computer, and only the site that created the cookie can read it.
Read Also: What Is Hepatitis C Positive
Immunohistochemical Evaluation With Ki67
For immunohistochemical analysis, the tissue slices were embedded in formalin and fixated in paraffin, and submitted to the immunohistochemical technique. This technique consists of the following steps: deparaffinization, rehydration, antigen retrieval, inactivation of endogenous peroxidase, and blockage of unspecific reactions. The primary antibody was incubated for 12 hours at 4°C, as per the specific dilution indicated on the package insert of each antibody used. Next, the streptavidin-biotin-peroxidase complex was applied it was developed with diaminobenzidine tetrahydrochloride chromogen and carried out in contrast with 3% hematoxylin. The antibody used was Ki67 , assessed in hepatic tissue by pathologists.
Analysis of the slides was based on the immunomarker intensity. The number of hepatocytes marked positively by the Ki67 was determined by manual count in five random visual fields, with a 10x magnification by a professional blinded to the intervention performed.
Fatty Liver Disease Has A Genetic Component
The likelihood of developing fatty liver disease is influenced in part by genetics. But the heritability of fatty liver is not so simple to determine. Research has shown that there is not just one gene that determines the risk of developing fatty liver disease, but rather an interaction of many genes in your DNA.
Research published in Clinical and Molecular Hepatology describes three genes PNPLA2, GCKR, and TM6SF2 that may influence the likelihood of fat accumulation in the liver. Specific variants of each gene are associated with increased risk of conditions associated with fatty liver disease, such as insulin resistance and type 2 diabetes. Of the three genes, PNPLA3 is the most well-studied gene and directly plays a role in liver metabolic processes. Moreover, a certain variant of the PNPLA3 gene is associated with a higher risk of fatty liver disease progression to NASH, fibrosis, and cirrhosis.
You May Like: Where To Get Tested For Hepatitis B
Recommended Reading: What Is The Definition Of Hepatitis C
Which Fruit Is Best For Liver
Fill your fruit basket with apples, grapes and citrus fruits like oranges and lemons, which are proven to be liver-friendly fruits. Consume grapes as it is, in the form of a grape juice or supplement your diet with grape seed extracts to increase antioxidant levels in your body and protect your liver from toxins.
Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease, sometimes called NAFLD, is not connected to alcohol intake. Instead, nonalcoholic fatty liver disease arises from the chronic consumption of unhealthy foods. Conditions like obesity, insulin resistance, hypertension, high triglycerides and cholesterol, and type 2 diabetes are risk factors for developing fatty liver disease.
Read Also: What Happens To Your Body When You Have Hepatitis C
Delivery Of Fatty Acids From Peripheral Stores To The Liver
Triglycerides are stored in adipose tissue and released as FFAs into the circulation through the actions of lipoprotein lipase. FFAs released from peripheral stores are hydrophobic and are strongly bound to circulating albumin. FFAs are transported by albumin to the liver where they can then be used as a substitute for -oxidation, stored as TAG, or exported as VLDL.
Excess glucose is converted to the liver, the backbone of most amino acids, can be converted to pyruvate and then to acetyl-coenzyme A , which feeds directly into cytosolic fatty acid synthesis.
Processes that can lead to excessive FFAs delivery or impaired -oxidation or secretion can lead to hepatic steatosis, increased mitochondrial reactive oxygen species and lipid peroxidation products.
Lose Weight If Needed

A higher body mass index increases the likelihood that you will have fatty deposits in your liver. When you lose weight, you also lose fat content in your liver. You can encourage weight loss by cutting back on portion sizes, increasing your physical activity, and eating whole foods instead of packaged and processed foods.
Read Also: How You Contract Hepatitis C
Echogenic Liver May Accompany Other Conditions
In addition to fatty liver disease, an echogenic liver might accompany other root causes. Here are a few examples:
- Viral hepatitis: Hepatitis A, hepatitis B, and hepatitis C are viral infections that target the liver. Hepatitis A and B are not so common in the United States. Hepatitis C tends to be more common. When untreated, chronic hepatitis may lead to fatty deposits, fibrosis, and cirrhosis.
- Genetic disorders: Certain genetic disorders may cause fat accumulation within liver cells, leading to fatty liver disease and other conditions.