How Is An Attack Of Acute Porphyria Diagnosed
For diagnosis of an attack of acute porphyria and identification of the type of porphyria, samples of urine, blood and stool need to be carefully tested in a laboratory that has expertise in porphyrias . The tests measure the concentration of porphyrins and their precursors ALA and PBG which will be very high in a patient with an attack of acute porphyria. It is important that these tests are carried out as soon as possible after the start of the illness as an accurate diagnosis may be difficult to establish after recovery from an acute attack, particularly after several months or years.
In a patient who is known to have inherited an acute porphyria, it may be difficult to decide whether symptoms are due to an attack of porphyria or an unrelated cause. In this situation, a urine test may help your doctor decide whether you are suffering from an acute attack or not. It is important that people with porphyria should not attribute all their illnesses to porphyria otherwise common but potentially serious conditions like appendicitis may be overlooked.
Missed Diagnosis And Misdiagnosis
In the urgent care setting, porphyria is often overlooked as a diagnostic possibility, because the symptoms are those of far more common conditions. When the initial screening tests for the common conditions are negative, patients usually are discharged with a diagnosis of viral gastroenteritis, irritable bowel syndrome, addiction withdrawal, or psychosomatic pain. A recent study of U.S. patients with genetically confirmed acute porphyria found that the diagnosis was delayed by an average of 15 years from the onset of symptoms . The case presented above is unusual, in that a perceptive resident physician thought of the diagnosis and ordered the correct test, a urine PBG.
The number of people who have been misdiagnosed and believe, erroneously, that they have acute porphyria far exceeds those with a confirmed diagnosis. When they come to an ED, very few will have documentation of their diagnosis. In this situation, a rapid PBG would be definitive but, as discussed above, is not available. Although neurological complications are not a concern in this group, a test that excludes acute porphyria would redirect attention to other possible causes of the patient’s complaints and potentially avoid an expensive and unproductive hospitalization.
Diagnosing Acute Hepatic Porphyria
The type of test that should be done depends on whether the person is having symptoms at the time. When a person is having symptoms from AHP, a spot urine test for porphobilinogen , a porphyrin, may be used. This test simply involves urinating in a specimen container, often asmall cup. The sample is then tested in the lab for PBG levels. If PBG levels are high, a healthcare provider can tell that a person has AHP.
Other tests that may be done include a urine test for aminolevulinic acid as well as testing for total porphyrins in the urine, blood, or stool. If someone has severe kidney disease, a blood test for PBG may also be done. This is due to the kidney being unable to properly filter urine. As AHP is caused by a gene defect, genetic testing can also be used to diagnose the condition. Unlike the urine tests mentioned above, the genetic test can be done when a patient is not experiencing symptoms. Genetic testing is also helpful for diagnosing the condition in family members of those with known AHP. The genetic test looks for problems in 4 different genes and can diagnose the specific type of AHP that one may have .
Don’t Miss: What Kills The Hepatitis C Virus
What Can I Do To Reduce My Risk Of Having An Acute Attack
Some acute attacks are precipitated by avoidable factors such as drugs, alcohol, fasting or dieting.
DrugsPeople with acute intermittent porphyria must take great care with medication, as some medicines are capable of triggering an acute attack. It is important ALWAYS to check the safety of any medicine or remedy with your doctor. This includes prescription medicines as well as over-the-counter treatments, supplements purchased over the internet, tonics and herbal remedies, some of which have been known to cause attacks. Although many drugs are considered suspect, good alternatives can almost always be found. Even though acute attacks are very rare before puberty, it is safest for children if they also keep to drugs that are known to be safe in porphyria.
Sometimes people with porphyria need a drug, perhaps for a serious illness like cancer, that carries some risk of provoking an acute attack or which has been introduced so recently that there is little information about its safety in porphyria. In this situation, your doctor, after fully discussing and evaluating the risks in consultation with a porphyria specialist, may decide to prescribe the drug for you with special follow-up.
AlcoholThere is evidence that alcohol can cause acute attacks, so you should not drink if you have any porphyria symptoms. Even if you have never had a porphyria attack, it is sensible to keep alcohol intake low.
Diet And Exercise When You Have Porphyria

There is no specific diet recommended for porphyria disorders other than eating healthily and making sure meals are taken regularly. This is more important for people who have acute porphyria as they are more sensitive to the effects of certain foods and beverages. This means keeping up a steady intake of calories by eating plenty of carbohydrates.
People who have acute porphyrias commonly suffer fatigue. This may be due to symptoms affecting muscles and joints and the sleep disturbance this may cause. In some cases the effects of medication used to control symptoms may contribute to bouts of tiredness.
It is important that your muscles do not get out of condition or reduce in size . For this reason it is likely doctors will encourage you to follow a daily exercise routine or to take part in moderate physical activity a few days a week to keep your muscles in shape and to help you sleep better.
Read Also: Hepatitis B Surf Ab Quant 3.1 Low
Signs And Symptoms Of Acute Hepatic Porphyria
- Signs and symptoms of AHP often mimic many other more common diseases , so these patients often repeatedly present with severe abdominal pain and they typically go through the usual evaluations for more common diseases such as acute abdomen, infections, inflammatory bowel disease, acute cholecystitis, appendicitis, and pancreatitis.1-5
- Note that there are no pathognomonic signs or symptoms, and atypical presentations are common.6-8
Why sign up with Medthority?
Develop your knowledge with our disease and condition focused Learning ZonesAccess content from credible sources, including expert-led commentary, videos, podcasts, and webinars as well as clinical trials, treatment information and guidelines Personalised dashboard providing updates and recommendations for content within your areas of interest
Acute Hepatic Porphyria: Pathophysiological Basis Of Neuromuscular Manifestations
- Division of Neuromuscular Diseases, Department of Neurology and Neurosurgery, Federal University of São Paulo , São Paulo, Brazil
Acute hepatic porphyria represents a rare, underdiagnosed group of inherited metabolic disorders due to hereditary defects of heme group biosynthesis pathway. Most patients have their definite diagnosis after several years of complex and disabling clinical manifestations and commonly after life-threatening acute neurovisceral episodes or severe motor handicap. Many key studies in the last two decades have been performed and led to the discovery of novel possible diagnostic and prognostic biomarkers and to the development of new therapeutic purposes, including small interfering RNA-based therapy, specifically driven to inhibit selectively delta-aminolevulinic acid synthase production and decrease the recurrence number of severe acute presentation for most patients. Several distinct mechanisms have been identified to contribute to the several neuromuscular signs and symptoms. This review article aims to present the current knowledge regarding the main pathophysiological mechanisms involved with the acute and chronic presentation of acute hepatic porphyria and to highlight the relevance of such content for clinical practice and in decision making about therapeutic options.
Read Also: Hepatitis C Virus Ab 0.1
When Is The Best Time To Be Tested For Acute Prophyria
The best time to be tested for porphyria is at the earliest opportunity. In practice, this means that families should be offered screening for acute porphyria as soon as possible after a relative has been found to have the condition. When one or other parent is already known to have an acute porphyria, their children should be tested as soon as possible, and in some countries babies can be tested at or soon after birth. It may be necessary to wait until your child is older, but it is recommended that testing takes place before onset of puberty. It is extremely rare for children to have a porphyria attack but there are two main advantages of early diagnosis. First, those who are found to have inherited one of the acute porphyrias can be advised about how to reduce their risk of an acute attack. Second, if an acute attack does develop, your doctor will be able to confirm the diagnosis and start treatment early.
Pathophysiology Of Acute Hepatic Porphyrias
Porphyrin precursors, in particular ALA, are likely neurotoxins , whereas porphyrins are light absorbing chemicals that act as photosensitizers, resulting in skin damage. In VP and HCP, both porphyrin precursors and porphyrins accumulate, and patients with these types can present with both neurovisceral attacks and cutaneous symptoms.
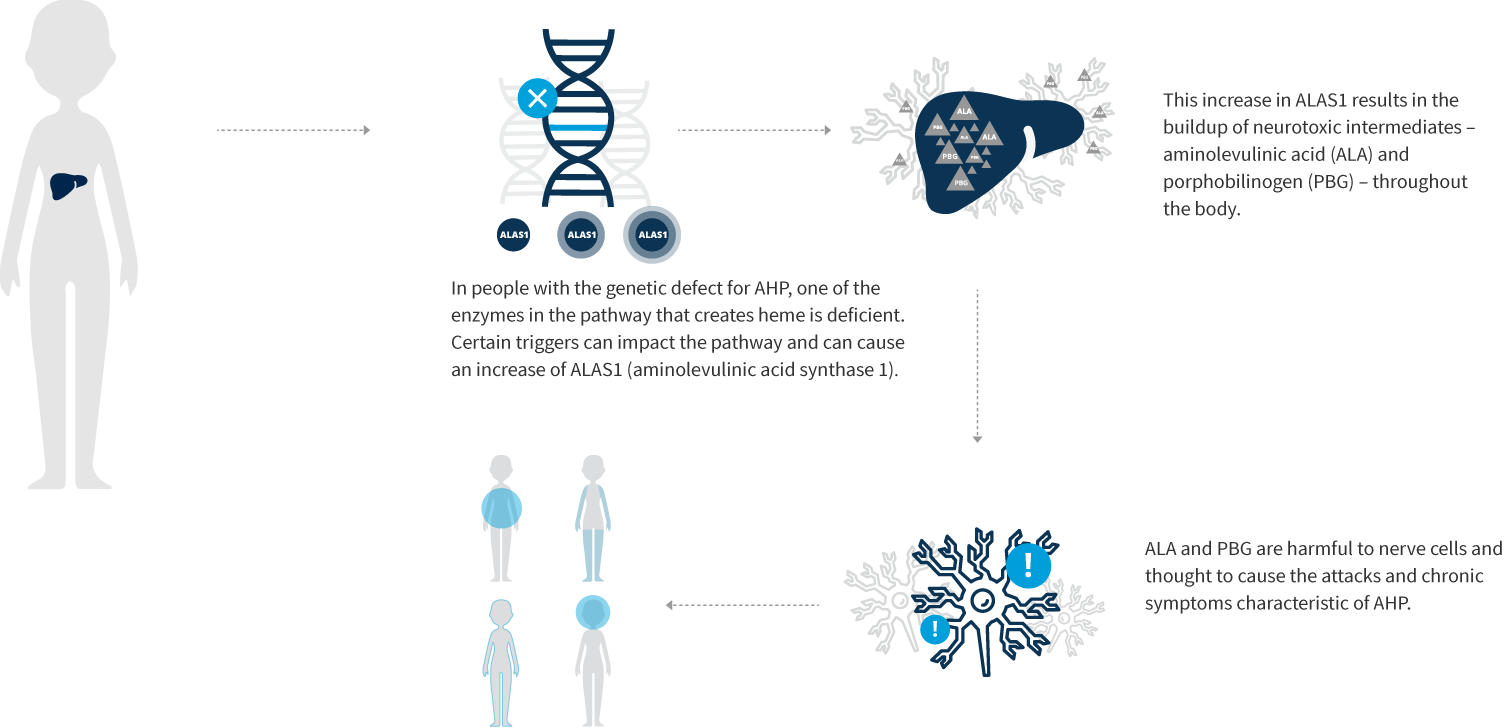
In AHP, the severity of the overproduction of intermediates is dependent on the demand for heme. When the need for heme production is low, ALAS1 typically remains the rate-limiting step in the pathway even with the presence of a partially defective enzyme downstream, and there is minimal accumulation of heme intermediates. Under inducing conditions that increase demand for heme synthesis, ALAS1 expression increases, and the defective enzymatic step becomes the rate-limiting step. With persistence of the demand for heme, ALAS1 expression remains elevated, resulting in abnormal accumulation of ALA and PBG. In HCP and VP, the accumulation of coproporphyrinogen III and protoporphyrinogen IX, respectively, inhibits the function of hepatic hydroxymethylbilane synthase . This is the metabolic setting for an acute attack of AHP.
While several hypotheses have been proposed regarding the pathogenesis of episodic acute attacks in AHP patients, including relative heme deficiency in nerve tissue, recent data has pointed to excess circulating ALA as the etiology.
Recommended Reading: Hepatitis C And Liver Failure
Treating Acute Hepatic Porphyria
When someone with AHP is experiencing an acute attack, treatment with intravenous hemin in the hospital can help with symptoms. At that time, it is also important to try to identify what may have caused the attack so that they can be avoided in the future.
A drug called Givosiran was approved by the U.S. Food and Drug Administration in 2019 for the treatment of adults with AHP. It is a medicine that is injected under the skin once a month. In clinical trials, patients on givosiran had fewer acute attacks from AHP when compared to those given a placebo. A placebo is a pill or treatment with no active ingredients. While taking givosiran, patients should have their liver and kidney tests monitored by their healthcare team. For patients with AHP who suffer from repeated severe attacks, do not respond to IV hemin or givosiran, or have a very poor quality of life, liver transplantation can be considered as a last resort.
Adapted from IFFGDs publication #581 Understanding Acute Hepatic Porphyria by Christopher V. Almario, MD, MSHPM Cedars-Sinai Medical Center, Karsh Division of Gastroenterology and Hepatology
Icular Issues For Women
Women are about five times more likely than men to experience an acute attack, due mostly to female hormones, particularly progesterone. This hormone is found in the combined oral contraceptive , as well as in hormone replacement therapy which is frequently prescribed for post-menopausal women. Oral contraceptive and HRT preparations containing progesterone or related compounds should be avoided if at all possible by women with an acute porphyria. Injectable and implantable long-term hormone preparations are very dangerous and must always be avoided. Barrier contraceptives are safe in porphyria. Hormonal IUDs which release small amounts of progesterone directly into the womb are usually well tolerated in patients with acute porphyria.
In special circumstances where the risk is low and the benefits high, your doctor may consider, after discussion with you and if possible with a porphyria specialist, that the use of progestogen-containing preparations is justified, particularly in replacement doses given through the skin from patches.
PregnancyThough nearly all pregnancies are uneventful, there is a small increased risk of having an acute attack during or after pregnancy. However, the chances and dangers of such an acute attack are much reduced if porphyria has been previously diagnosed. It is therefore very important for the doctors providing care during pregnancy to know that you have an acute porphyria.
Don’t Miss: Can You Get Hepatitis C Twice
Prevalence Of Acute Hepatic Porphyria
The prevalence of AIP has been estimated at 510 cases per 100,000. However, this is based largely on people with symptoms, who represent only a small fraction of those who carry a relevant mutation and are at risk of an attack. In one study of mutation prevalence from France, 3,350 healthy blood donors were screened for HMBS deficiency. The test was positive in four, and a known AIP mutation was documented in two. Thus, the prevalence of mutations in this group was at least 1:1,675 far larger than is generally assumed. Another study from northwestern Russia and Finland screened patients who were admitted to a neurology ward with acute polyneuropathy or encephalopathy and abdominal pain. Out of 108 patients, 11% proved to have previously undiagnosed acute porphyria. While these studies are small, they suggest that people coming to an Emergency Department with recent onset abdominal pain may have a mutation for AIP more often than is generally assumed.
Recurrent Attacks Of Porphyria
A few patients, mostly those with AIP, develop a pattern of recurrent attacks, usually defined as four or more attacks requiring admission to hospital for treatment in one or more years. In women these attacks may be related to the normal hormone changes of the menstrual cycle with symptoms typically starting in the week or so before menstruation, but in many patients, there is no clear trigger for their attacks. Patients with recurrent porphyria attacks should be referred to a specialist porphyria centre if possible so they can get the best possible care. The main treatment is to give regular infusions of hemin to try to prevent attacks. In very severe cases, liver transplantation may be considered. A new treatment for recurrent attacks of porphyria gave very promising results in clinical trials but is not yet available to patients in all countries.
Also Check: Hepatitis C Causes Symptoms And Treatment
Biochemical Diagnosis Of Acute Porphyria
In all three autosomal dominant acute porphyrias, attacks are accompanied by a clear increase in PBG , which, for convenience, is generally assessed in urine rather than blood. In active AIP, the type most commonly associated with acute attacks, the PBG is at least 10-fold the upper limit of normal, more typically 20- to 100-fold. A urine PBG of > 50 mg/g creatinine in a patient with pain symptoms of unknown cause is highly specific for the diagnosis occasional genetic carriers have PBG levels in this range even when feeling well and thus represent false-positive cases. While this is unusual, it highlights the importance of having baseline information from urine samples that are collected when the patient is feeling well. ALA should be evaluated at the same time to identify cases of lead poisoning, which can mimic acute porphyria. It would also identify the rare individual with ALA dehydratase deficiency.
Effective Prophylaxis Has Transformed Patients’ Lives Beyond Management Of Acute Attacks
byCrystal Phend, Contributing Editor, MedPage Today December 29, 2021
While the road to a diagnosis of acute hepatic porphyria can be long, preventive treatment now available to patients has been “transformative.”
Acute attacks of the inherited disorder occur due to overproduction of neurotoxic porphyrin molecules in the liver during heme production. Then, symptoms strike suddenly, characterized by severe pain that responds poorly to analgesics, along with a constellation of accompanying nausea, vomiting, constipation, tachycardia, seizures, peripheral neuropathy, and severe muscle weakness that can even lead to respiratory failure or death.
Initial management of such attacks calls for giving fluids, antiemetics, analgesics, and antiseizure medication for the some 20% of patients who have seizures, as a review in the New England Journal of Medicine pointed out. However, a number of anticonvulsants are considered unsafe in acute porphyria, and patients’ medication lists should also be reviewed for oral contraceptives, progestins, spironolactone, carisoprodol, and others that are likewise risky.
The only specific treatment that can speed up resolution of acute attacks is intravenous hemin treatment in the hospital, which typically takes effect within 3 to 4 days.
Hemin has been sometimes used off-label as monthly prophylaxis, but long-term use leads to iron accumulation that can induce liver fibrosis.
Disclosures
Also Check: Is Hiv The Cause Of Hepatitis B
Acute Motor Axonal Neuropathy
Acute flaccid paralysis presenting as acute to subacute symmetric proximal quadriparesis due to motor axonal polyradiculopathy or neuronopathy represents the most common neuromuscular presentation of AHP in the Emergency Department and Intensive Care Unit , resembling clinical and neurophysiological features of GuillainBarré syndrome and representing one of the main factors for medical and financial burden of AHP .
Classically, the peripheral neuropathy in AHP usually starts with muscle pain and weakness commonly preceded by abdominal pain and psychiatric disturbances that may further progress over a 2-week period for tetraplegia or death, with some patients requiring mechanical ventilation due to paresis of respiratory and bulbar muscles. The acute motor axonal neuropathy can occur in up to 68% of patients and is usually symmetric and starts in the upper limbs with frequent association with autonomic disturbances. Cranial nerve involvement is more rarely observed, and sensory neuropathy is usually identified by mild distal lower limb paresthesias or with a painful bathing suit proximal distribution. Some patients may disclose permanent quadriplegia after severe acute attacks, even after proper early therapy introduction .
The motor symptoms in the context of a chronic motor axonal neuropathy in AHP are associated with irreversible damage or severe compromise to the axonal compound of the peripheral nerve after acute decompensation .