Whats The Prognosis For Hepatitis B
Your doctor will know youâve recovered when you no longer have symptoms and blood tests show:
- Your liver is working normally.
- You have hepatitis B surface antibody.
But some people don’t get rid of the infection. If you have it for more than 6 months, youâre whatâs called a carrier, even if you donât have symptoms. This means you can give the disease to someone else through:
- Unprotected sex
- Contact with your blood or an open sore
- Sharing needles or syringes
Doctors donât know why, but the disease does go away in a small number of carriers. For others, it becomes whatâs known as chronic. That means you have an ongoing liver infection. It can lead to cirrhosis, or hardening of the organ. It scars over and stops working. Some people also get liver cancer.
If youâre a carrier or are infected with hepatitis B, donât donate blood, plasma, body organs, tissue, or sperm. Tell anyone you could infect — whether itâs a sex partner, your doctor, or your dentist — that you have it.
Show Sources
CDC: âHepatitis B Questions and Answers for Health Professionals,â âHepatitis B Questions and Answers for the Public.â
Mayo Clinic: âHepatitis B.â
UpToDate: âHepatitis B virus: Screening and diagnosis.â
CDC.
HealthyPeople.gov: âHepatitis B in Pregnant Women: Screening.â
Annals of Internal Medicine: âScreening for Hepatitis B Virus Infection in Nonpregnant Adolescents and Adults: U.S. Preventive Services Task Force Recommendation Statement.â
How Many People Have Hepatitis B
In the United States, an estimated 880,000 to 1.89 million people are chronically infected with HBV. New cases of HBV infection in the United States had been decreasing until 2012. Since that time, reported cases of acute hepatitis B have been fluctuating around 3,000 cases per year. In 2020, 2,157 cases of acute hepatitis B were reported however, because of low case detection and reporting, the Centers for Disease Control and Prevention estimates that there were 14,000 acute hepatitis B infections. The rate of acute cases of HBV decreased by 32% after 2019 which may be related to the disruptions of the COVID-19 pandemic. For the most recent surveillance data visit CDC Viral Hepatitis Surveillance.
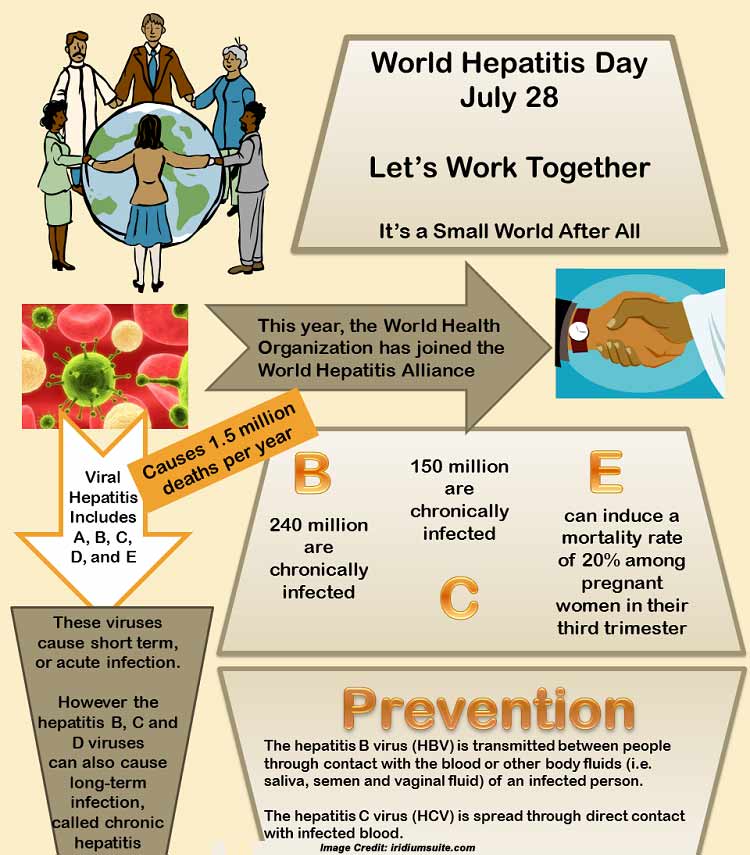
Globally, HBV is the most common blood-borne infection with an estimated 296 million people infected according to the World Health Organization .
Medical Treatment For Hepatitis A B & C
Treatment for hepatitis A, B, or C is based on which type of hepatitis is present in the bloodstream and the severity of the resulting liver damage. Depending on the results of diagnostic tests, our specialists at NYU Langone may recommend antiviral medication to stop the virus from replicating and protect your liver from further damage.
Read Also: How Do You Get Infected With Hepatitis B
How Is Hepatitis B Prevented
Testing & Vaccination
- The hepatitis B vaccine offers excellent protection against HBV. The vaccine is safe and highly effective. Vaccination consists of 3 doses of vaccine over the course of 6 months. Protection lasts for 20 years to life.
- The American Academy of Pediatrics recommends that all children should receive hepatitis B vaccine starting at birth. .
- The CDC recommends hepatitis B vaccine for persons traveling to countries where HBV is common .
- If you have one or more risk factors for hepatitis B infection, you should get a simple HBV blood test. The blood test will determine whether you are:
- immune to hepatitis B or
- susceptible to hepatitis B and need vaccination or
- infected with hepatitis B and need further evaluation by a physician
Perinatal Hepatitis
- California law requires testing of all pregnant women for hepatitis B infection
- If the mother is HBV-infected, she will pass the infection to the baby during the birth process, unless the baby gets immunized within hours of birth
- Giving the infant HBIG and HBV vaccine right away will reliably prevent infection of the infant
- Other family members should best tested for hepatitis B too, and given vaccine if they are not already infected or immune
Healthy Habits
After Exposure to Hepatitis B
Perinatal Hepatitis B Prevention Program
PERINATAL HEPATITIS B PREVENTION PROGRAM
Disease Burden of Perinatal Hepatitis B
Each year in the United States approximately 24,000 Hepatitis B surface antigen positive women give birth1. Out of these births, approximately 924 infants will become infected with the Hepatitis B virus from perinatal transmission. In the District of Columbia, an estimated 39 – 69 births to HBsAg+ women are expected this year.
Infants are particularly vulnerable as 90% of those infants who get Hepatitis B within the 12 months of birth become chronically infected and have a higher chance of developing liver cancer or liver failure. Individuals who become infected with Hepatitis B after five years of age only have a 5% chance of chronic infection.
Prevention of Perinatal Hepatitis B
It is the mission of the District of Columbia Department of Health to identify hepatitis B surface antigen-positive pregnant women or infants at delivery and to work with care providers to administer appropriate treatment to prevent the spread of the hepatitis B virus .
Recommendations from the Center for Disease Control for perinatal Hepatitis B prevention include:
Perinatal and Postnatal Hepatitis B Reporting
You May Like: How Do You Get Hepatitis C Symptoms
Hbv Infection Following Vertical Transmission
In neonates infected by mother to child transmission , the risk of developing CHB depends on the HBeAg status of the mother. Neonates whose mothers were HBeAg positive during the perinatal period have a 90% chance of developing chronic infection, whereas this risk is < 15% in neonates with HBeAg-negative mothers . Neonatal vaccination can be effective in reducing the risk of MTCT and is discussed below. Both the immune tolerant phase and the HBeAg-positive CHB phase are prolonged in individuals infected in the neonatal period, with HBeAg clearance typically occurring during the third or fourth decade . This longer course of infection increases the risk of developing HBV-related liver complications.
Transmission Route Of Hbv And Outcomes Of Hbv Infection At Different Ages
To prevent HBV infection effectively, it is crucial to understand its route of transmission. HBV infection is transmitted through either a horizontal route or through a mother-to-infant route. Mother-to-infant transmission was called vertical transmission in the past, but this term is less frequently used now because it caused confusion with genetic transmission, which does not occur with HBV. In endemic areas, perinatal mother-to-infant transmission is the most important route of transmission HBV infection is encountered mainly during infancy and early childhood.
Age at infection and source of infection affect the outcome of HBV infection . Without immunoprophylaxis, perinatal transmission from highly infectious hepatitis B carrier mothers results in chronic infection in 90% of their infants . In contrast, only 5% of infants of HBeAg-negative HBsAg carrier mothers become chronic carriers and a small fraction may develop acute or fulminant hepatitis B . Among 2- to 4-yr-old toddlers, 25% will become chronic carriers . In contrast, only 2.7% of the newly HBV-infected 18- to 19-yr-old university students became chronic carriers . Thus, the younger the age at infection, the higher the HBV carriage rate .
Read Also: New Drug To Cure Hepatitis C
Do I Need To Be Tested For Hepatitis B Before Getting The Vaccination
In some cases, your provider may decide to test your blood for antibodies to hepatitis B, but this is not mandatory for everyone.
If the test shows that you have antibodies to hepatitis B, it means that you were infected with hepatitis B in the past, have current hepatitis B infection, or you were previously vaccinated for hepatitis B. It is important to discuss the results of your test with your provider. If you already have antibodies to hepatitis B, you don’t need to get hepatitis B vaccination.
What Are The Treatments For Hepatitis B
If you think you may have been exposed to hepatitis B, its important to talk with a healthcare professional as soon as possible.
A doctor or other healthcare professional may administer the first dose of the hepatitis B vaccine and a shot of hepatitis B immunoglobulin. This is a combination of antibodies that provide short-term protection against the virus.
Though both can be given up to a week after exposure, theyre most effective at preventing infection if administered within 48 hours.
If you receive a diagnosis of acute hepatitis B, a doctor may refer you to a specialist. They may advise you to get regular blood tests to ensure you dont develop chronic hepatitis.
Many people with acute hepatitis B dont experience serious symptoms. But if you do, it can help to:
- get plenty of rest
- take over-the-counter pain mediation, like naproxen, when needed
Other lifestyle changes may also be needed to manage your infection, such as:
- eating a nutritious, balanced diet
- avoiding substances that can harm your liver, such as:
- certain herbal supplements or medications, including acetaminophen
If blood tests show you still have an active infection after 6 months, your doctor may recommend further treatment, including medications to help control the virus and prevent liver damage.
Also Check: Can Hiv Lead To Hepatitis
Prevention Of Mother To Child Transmission
PEP, initiated at birth, is recommended for all infants of HBV infected mothers . PEP using a combination of HBIG and an accelerated course of HBV vaccine has been shown to be effective in preventing perinatal HBV transmission in 90% of cases . Many countries, including the USA and the UK, have introduced routine antenatal screening of all pregnant women to identify HBsAg-positive mothers and maximize opportunities to prevent mother to child transmission of HBV infection .
Prevention Tips For Hepatitis B
Hepatitis B Prevention Measures
Hepatitis B is a vaccine-preventable disease. More than 1 billion doses of the hepatitis B vaccine have been given worldwide, and it is considered to be a very safe and effective vaccine to protect infants, children and adults from hepatitis B. Learn more.
All sexual partners, family and close household members living with a chronically infected person should be tested and vaccinated. It is important to remember that hepatitis B is not spread casually! It is not spread by coughing, sneezing, hugging, cooking and sharing food. It is spread through direct contact with infected blood and bodily fluids.
Additional Prevention Measures
In addition to vaccination, there are other simple ways to help stop the spread of hepatitis B:
- Wash your hands thoroughly with soap and water after any potential exposure to blood
- Use condoms with sexual partners
- Avoid direct contact with blood and bodily fluids
- Clean up blood spills with a fresh diluted bleach solution
- Cover all cuts carefully
- Avoid sharing sharp items such as razors, nail clippers, toothbrushes, and earrings or body rings
- Discard sanitary napkins and tampons into plastic bags
- Avoid illegal street drugs
- Make sure new, sterile needles are used for ear or body piercing, tattoos, and acupuncture
You May Like: What Organ Does Hepatitis B Affect
What Is Hepatitis B
Hepatitis B is a contagious liver infection caused by the hepatitis B virus . The natural course of hepatitis B disease is different from one person to another.
Treatment with anti-viral drugs works for some people with HBV who are starting to develop liver damage. Whether treatment will be successful depends on many factors, and these are best discussed with a physician who specializes in liver diseases. When treatment is successful, liver scarring and the potential for liver cancer are reduced.
How Are Hepatitis B And Hepatitis C Spread From Person To Person
Like HIV, the hepatitis B and hepatitis C viruses spread:
- Perinatally: Pregnant people can pass these infections to their infants. HIV-HCV coinfection increases the risk of passing on hepatitis C to the baby.
- Sexually: Both viruses can also be transmitted sexually, but HBV is much more likely than HCV to be transmitted sexually. Sexual transmission of HCV is most likely to happen among gay and bisexual men who have HIV.
Also Check: Common Symptoms Of Hepatitis C
What Other Problems Can Hepatitis B Cause
In rare cases, acute hepatitis B can cause liver failure.
Chronic hepatitis B can develop into a serious disease that causes long-term health problems such as cirrhosis , liver cancer, and liver failure.
If you have ever had hepatitis B, the virus may become active again, or reactivated, later in life. This could start to damage the liver and cause symptoms.
To Prevent Perinatal Transmission:
You May Like: Does Hepatitis Cause Weight Loss
The Earliest Universal Hbv Mass Immunization Program
The first universal hepatitis B mass vaccination program in the world was launched in Taiwan in July 1984. Pregnant women were screened for HBsAg and then HBeAg. Infants of mothers negative for HBeAg or HBsAg received the plasma-derived hepatitis B vaccine only at 0, 1, 2, and 12 mo. The vaccine was shifted to a recombinant hepatitis B vaccine at 0, 1, and 6 mo after October 1992. The immunization program in the initial 2 years covered only infants of HBsAg carrier mothers. From the third year on, all of the infants were covered. Infants of highly infectious mothers with positive HBeAg received HBIG within 24 h after birth in addition to the hepatitis B vaccine. The coverage rate of hepatitis B vaccine for neonates was 94% in initial years, and was 99% recently. Catch-up vaccination was also given to preschool and then school children .
How Is Hepatitis B Transmitted
Hepatitis B is spread in several distinct ways: sexual contact sharing needles, syringes, or other drug-injection equipment or from mother-to-child at birth.
In the United States, in 2018, injection drug use was the most common risk factor reported among people with an acute HBV infection, followed by having multiple sex partners. Less commonly reported risk factors included accidental needle sticks, surgery, transfusions, and household contact with a person with HBV infection. In the United States, healthcare-related transmission of HBV is rare.
Mother-to-child transmission of HBV is especially concerning, because it is preventable. An estimated 25,000 infants are born to mothers diagnosed with HBV each year in the United States, and approximately 1,000 mothers transmit HBV to their infants. Without appropriate medical care and vaccinations, 90% of HBV-infected newborns will develop chronic infection, remaining infected throughout their lives. Up to 25% of people infected at birth will die prematurely of HBV-related causes. For this reason, the standard of care for pregnant women includes an HBV test during each pregnancy so that the appropriate steps can be taken to prevent HBV-positive mothers from transmitting the disease to her infant.
You May Like: Is Hepatitis C Serious Disease
What Should You Do If Exposed To The Hepatitis B Virus
If you know you were recently exposed to the hepatitis B virus, you may get protection from an injection of hepatitis B immunoglobulin , which is different from hepatitis B vaccine. HBIG is given only when it is suspected or known that someone has been infected with hepatitis B, and it is given within 24 hours after the exposure. HBIG will protect you for 3 to 6 months, but it is strongly recommended that you also begin the hepatitis B vaccination series within 7 days of your exposure.
Who Is At Risk For Hepatitis B
Anyone can get hepatitis B, but the risk is higher in:
- Infants born to mothers who have hepatitis B
- People who inject drugs or share needles, syringes, and other types of drug equipment
- Sex partners of people with hepatitis B, especially if they are not using latex or polyurethane condoms during sex
- Men who have sex with men
- People who live with someone who has hepatitis B, especially if they use the same razor, toothbrush, or nail clippers
- Health care and public-safety workers who are exposed to blood on the job
- Yellowish eyes and skin, called jaundice
If you have chronic hepatitis B, you may not have symptoms until complications develop. This could be decades after you were infected. For this reason, hepatitis B screening is important, even if you have no symptoms. Screening means that you are tested for a disease even though you don’t have symptoms. If you are at high risk, your health care provider may suggest screening.
Recommended Reading: How Do You Test For Hepatitis B
Prevention Against Hbv Infection: Immunization And Other Strategies
HBV immunization can be classified into passive and active immunization. Passive immunization using hepatitis B immunoglobulin provides temporary immunity, whereas active immunization by the vaccine yields long-term immunity. Because in endemic areas the major infection route comes from maternal transmission, and the outcome of perinatal transmission results in a very high rate of chronic infection, the best timing of initial HBV immunization, therefore, should be within 24 h after birth, followed by subsequent doses of HBV vaccine during infancy.
Other prevention strategies, such as screening the blood products, proper sterilization of injection needles and syringes, and avoidance of risky behaviors, such as parenteral drug abuse, tattoo, or skin piercing, may preclude HBV horizontal transmission. Education to avoid high-risk behaviors should be advocated in addition to vaccination. In addition to the program for infants, many countries with low prevalence of HBV infection also have HBV vaccination programs for adolescents to prevent exposure to HBV by sexual contacts or other risk behaviors.