Pathophysiology Of Acute Hepatic Porphyrias
Porphyrin precursors, in particular ALA, are likely neurotoxins , whereas porphyrins are light absorbing chemicals that act as photosensitizers, resulting in skin damage. In VP and HCP, both porphyrin precursors and porphyrins accumulate, and patients with these types can present with both neurovisceral attacks and cutaneous symptoms.
In AHP, the severity of the overproduction of intermediates is dependent on the demand for heme. When the need for heme production is low, ALAS1 typically remains the rate-limiting step in the pathway even with the presence of a partially defective enzyme downstream, and there is minimal accumulation of heme intermediates. Under inducing conditions that increase demand for heme synthesis, ALAS1 expression increases, and the defective enzymatic step becomes the rate-limiting step. With persistence of the demand for heme, ALAS1 expression remains elevated, resulting in abnormal accumulation of ALA and PBG. In HCP and VP, the accumulation of coproporphyrinogen III and protoporphyrinogen IX, respectively, inhibits the function of hepatic hydroxymethylbilane synthase . This is the metabolic setting for an acute attack of AHP.
While several hypotheses have been proposed regarding the pathogenesis of episodic acute attacks in AHP patients, including relative heme deficiency in nerve tissue, recent data has pointed to excess circulating ALA as the etiology.
Classification Of The Porphyrias
Traditionally, the porphyrias have been classified as either hepatic or erythropoietic depending on the primary site of overproduction and accumulation of porphyrin precursors or porphyrins, although some porphyrias have overlapping features., The hepatic porphyrias are characterized by overproduction and initial accumulation of the porphyrin precursors, ALA and PBG, and/or porphyrins primarily in the liver, whereas in the erythropoietic porphyrias, overproduction and initial accumulation of the pathway intermediates occur primarily in bone marrow erythroid cells. Here, for simplicity, we have classified the 8 major porphyrias into 3 groups: the 4 acute hepatic porphyrias, the single hepatic cutaneous porphyria PCT, and the 3 erythropoietic cutaneous porphyrias . It should be appreciated that there is some overlap, as patients with the acute hepatic porphyrias, hereditary coproporphyria , and variegate porphyria may have cutaneous lesions, and the rare homozygous dominant forms of acute intermittent porphyria , HCP, and VP, as well as the rare homozygous recessive form of PCT, hepatoerythropoietic porphyria, have erythropoietic manifestations.
How Is An Acute Porphyria Diagnosed
Porphyria may be suspected clinically, but must be confirmed by laboratory tests .
The most important immediate test is a measurement of light-protected urinary porphobilinogen.
- A normal porphobilinogen in an unwell patient excludes acute porphyria.
- A false positive can occur in dehydrated patients with concentrated urine a quantitative urinary porphobilinogen corrects for creatinine and can overcome this problem.
Urinary porphyrins may also rise in an acute attack, but are less specific as urinary porphyrins may occur in infections, hepatobiliary disease, haematological disorders, heavy metal exposure, and lead poisoning.
Once an acute attack is confirmed, blood and faecal samples are tested to determine the subtype of porphyria. Samples should be sent to an accredited laboratory or one familiar with porphyria testing .
A skin biopsy of cutaneous lesions in variegate porphyria and hereditary coproporphyria has similar findings to porphyria cutanea tarda.
Screening of relatives is essential as the majority of people with the geneticmutation will have clinically latent disease but are at risk of developing acute attacks and should heed the same advice regarding triggers.
Read Also: How Do You Get Infected By Hepatitis C
Advances In Diagnosis And Treatment Of Acute Intermittent Porphyria
ABSTRACT
REFERENCES
Stein PE, Badminton MN, Rees DC. Update review of the acute porphyrias. Br J Haematol 2017 176:527-538. doi:10.1111/bjh.14459
Whatley SD Badminton MN. Role of genetic testing in the management of patients with inherited porphyria and their families. Ann Clin Biochem 2013 50:204-16. doi:10.1177/0004563212473278.
Elder G, Harper P, Badminton M, Sandberg S, Deybach JC. The incidence of inherited porphyrias in Europe. J Inherit Metab Dis 2013 36:849-57. doi:10.1007/s10545-012- 9544-4
Mykletun M, Aaesand AK, Støle E, Villanger JH, Tollånes MC, Baravelli C, et al. Porphyrias in Norway. Tidsskr Nor Lægeforen 2014 134:831-6. doi:10.4045/tidsskr.13.0649
Chen B Solis-Villa C Hakenberg J Qiao W Srinivasan RR Yasuda M et al. Acute intermittent porphyria: Predicted pathogenicity of HMBS variants indicates extremely low penetrance of the autosomal dominant disease. Hum Mutat 2016 37:1215-22. doi:10.1002/humu.23067
Jeans JB, Savik K, Gross CR, Weimer MK, Bossenmaier IC, Pierach CA, et al. Mortality in patients with acute intermittent porphyria requiring hospitalization: a United States case series. Am J Med Genet 1996 65:269-73.
Kostrzewska E, Gregor A. 35 Years of effort to improve the diagnosis of porphyria. Przegl Lek 1999 56:576-8.
Kauppinen R, Mustajoki P. Prognosis of acute porphyria: occurrence of acute attacks precipitating factors and associated diseases. Medicine 1992 71:1-13.
Heme Biosynthesis And Regulation
Heme is required for a variety of hemoproteins, including hemoglobin, myoglobin, respiratory cytochromes, and the cytochrome P450 enzymes. Hemoglobin synthesis in erythroid precursor cells accounts for 85% of daily heme synthesis in humans. Hepatocytes account for most of the rest, primarily for synthesis of cytochrome P450 enzymes, which are especially abundant in the liver endoplasmic reticulum, and turn over more rapidly than many other hemoproteins, such as the mitochondrial respiratory cytochromes.
Read Also: How Serious Is Hepatitis C
The Erythropoietic Cutaneous Porphyrias
The erythropoietic cutaneous porphyrias, congenital erythropoietic porphyria and EPP, and its recently recognized X-linked form, XLP, are characterized by elevations of porphyrins in bone marrow and erythrocytes and usually present with cutaneous photosensitivity in infancy or early childhood,, or in the case of CEP, even in utero as nonimmune hydrops fetalis.
Diagnosis And Management Of Porphyria
Although porphyria is a relatively uncommon condition, it should be considered in patients presenting with an atypical medical, psychiatric, or surgical history. Acute attacks are associated with a substantial morbidity and mortality there is a need for rapid and accurate diagnosis of the neuropsychiatric porphyrias, particularly because haem arginate can induce a definite remission if given early in an attack. Additionally, porphyrias may present with skin lesions or photosensitivity.
Summary points
The porphyrias form a group of inherited disorders of haem biosynthesis of which there are seven main types
Porphyrias can be classified into acute , cutaneous, and mixed forms
Acute forms can be life threatening, but attacks can be aborted by early administration of haem arginate
When a patient is diagnosed with an acute porphyria the whole family needs to be screened
You May Like: What Hepatitis Is Not Curable
Muscle Weakness And Neurologic Deficits
Muscle weakness and focal neurologic deficits such as tetraparesis may be the presenting feature, especially in women of reproductive age. Limb pain is common. A motor, axon-predominant neuropathy is a strong clue when accompanied by abdominal and psychiatric symptoms. A minority of patients present with paresis only, and no abdominal pain.
The lifetime prevalence of acute intermittent porphyriaassociated seizures has been reported as 2.2% of all those with known acute intermittent porphyria and 5.1% of all those with manifest acute intermittent porphyria. Epileptic seizures among persons with acute intermittent porphyria are less common than has been previously described.
Deterrence And Patient Education
During an acute attack, potentially harmful medications should be discontinued whenever possible. It is strongly advised for clinicians to consult the websites of the American Porphyria Foundation and the European Porphyria Network , which list many medications, including those that are not classified with certainty provide evidence for these classifications, and are regularly updated. Also, these websites should be consulted to avoid prescribing harmful medications in treating concurrent illnesses or symptoms.
Potentially harmful lifestyle factors include smoking and alcohol use. Patients should be counseled to avoid or discontinue smoking, including the use of marijuana, and to avoid alcohol intake. Smoking and alcohol use can both exacerbate acute hepatic porphyrias via induction of hepatic cytochrome P450 enzymes , which, in turn, can diminish the pool of hepatic heme and directly induce enzymes in the porphyrin pathway, leading to increased synthesis of toxic heme precursors.
Acute attacks are also associated with sex hormones , decreased caloric or carbohydrate intake , and metabolic stress due to infections or other illnesses.
Also Check: How Do You Contract Hepatitis B
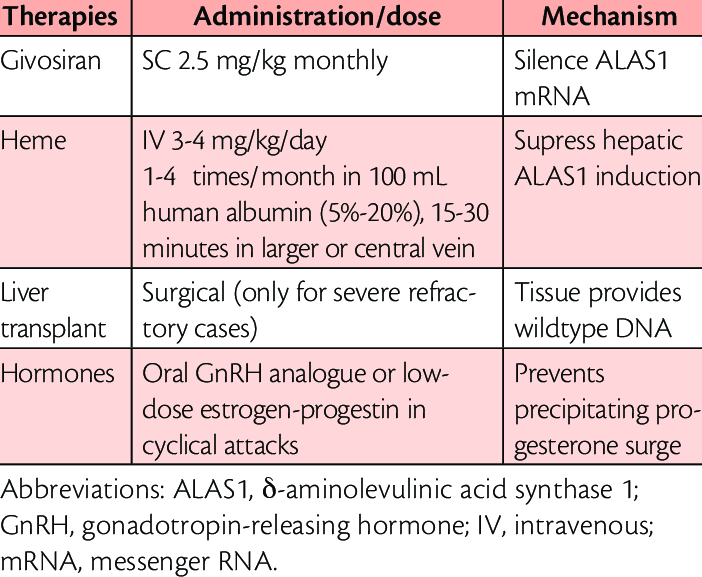
Management And Monitoring Of Aip
Management of acute signs and symptoms of a patient with known or highly suspected AIP involves recognizing the neurovisceral manifestations , treating precipitating factors , withdrawing porphyrinogenic medications, carbohydrate loading, symptom control, and supportive care including safe medications. Vomiting patients need intravenous hydration and may need correction of hyponatremia. Infusion of 10% dextrose, to deliver 300 to 500 g of glucose, may abort an early, mild attack however, this is often not effective for more severe episodes and could worsen hyponatremia. For clinical complications severe enough to necessitate aggressive support in the clinic or ED, and with any new neurological deficit, intravenous infusion of hemin is indicated. Hemin should be reconstituted in 25% albumin and administered by slow infusion to minimize coagulopathy and phlebitis. Patients who need frequent infusions of hemin benefit from placement of a semipermanent central venous catheter. To optimally suppress ALAS1 activity, 3 to 4 mg/kg/day for 4 days is needed. Although serial urine PBG/creatinine determinations during a course of hemin can reflect a biochemical response, clinical manifestations often do not correlate with absolute levels of urine PBG excretion. This is especially true for patients who chronically excrete high levels of urine PBG between episodes.
The Pathophysiology Of Acute Hepatic Porphyria
Figure 3. Diagram disclosing the different pathophysiological mechanisms involved with axonal damage in AHP during acute neurovisceral attacks. Different trigger factors lead to cytochrome P450 induction, heme group degradation, and/or the inhibition of heme synthesis, giving rise to ALA synthase induction and the secondary formation of high contents of neurotoxic ALA and PBG metabolites, leading to acute neurovisceral attack. ALA synthase induction is also associated with abnormal production of hemoprotein and secondary depletion of pyridoxal-phosphate . Legend, ALA, delta-aminolevulinic acid GABA, gamma-aminobutyric acid IL-6, interleukin-6 MPO, myeloperoxidase NO, nitric oxide OXPHOS, oxidative phosphorylation PBG, porphobilinogen PGC-1a, peroxisome proliferator-activated receptor-gamma coactivator-1 alpha SOD, superoxide dysmutase.
There is overproduction of neuroactive metabolites derived from tryptophan in AHP. Animal models showing increased plasma concentration and brain uptake of tryptophan and increased synthesis of serotonin in the central nervous system were explained due to decreased activity of tryptophan pyrrolase, which is a heme-dependent enzyme . This reduced activity leads to increase in serotonin plasmatic levels and can explain some of the neurovisceral features during acute attacks of porphyria .
Also Check: Hepatitis A Outbreak Michigan Restaurant
Identification Of Known Triggers Of Acute Attacks
A number of conditions are known to induce heme synthesis and the expression of ALAS1 in the liver, which can lead to acute attacks. A mainstay in management of acute attacks is identifying and eliminating inducers of acute attacks.
Medications that are known to induce synthesis of cytochrome P450s are a well-known class of triggers for acute attacks. Several drug safety databases are available with lists of drugs that are considered risky as well as those that are thought to be safe .
Prolonged fasting also predisposes to acute attacks. First attacks of acute porphyria have been reported during a fast imposed by abdominal surgery or with extreme measures for weight loss such as a highly restricted diet or gastric bypass . Animal studies have shown that fasting induces the expression of peroxisome proliferator-activated receptor gamma coactivator 1-alpha , which induces the expression of ALAS1 . This is the basis for giving carbohydrates to patients in an acute attack . Conversely, there is no evidence that a diet with excess carbohydrates protects against attacks. Instead, patients who take extra carbohydrates for this purpose can develop obesity. While exercise can affect caloric balance, it has never been implicated in acute attacks.
Clinical Presentation And Chronic Complications Of Aip
The cardinal symptoms of AIP attacks are listed in . The classic triad of severe abdominal pain, peripheral neuropathy, and central or autonomic nervous system manifestations are variable and nonspecific and carry a broad differential diagnosis. Thus, diagnosis can be delayed for many years, and many patients are misdiagnosed or receive unhelpful treatments. Abdominal pain typically builds gradually over hours to days and is often diffuse and associated with nausea, vomiting, constipation, or diarrhea. Sensory neuropathy may be manifested as paresthesia, dysesthesia, hyporeflexia, and musculoskeletal pain in the extremities or trunk. Motor neuropathy often starts with proximal muscle weakness in the upper extremities and may progress to the distal and lower extremities. Respiratory muscle compromise can be life-threatening. Autonomic dysfunction is responsible for tachycardia, hypertension, diaphoresis, fever and chills, and bladder and gut dysmotility. CNS manifestations include insomnia, anxiety, depressed mood, dysphoria, confusion, delirium, seizure, and coma.
Read Also: What Is A Hepatic Diet
Pathogenesis Of The Acute Attacks
For years, the pathogenesis of these attacks was intensely debated., Did they result from: elevated levels of ALA and PBG, one or both being neurotoxic, heme deficiency in the nervous system, or both? Clearly, induction of the acute attacks is related to environmental or hormonal factors, such as drugs, diet, and steroid hormones that induce ALAS1 resulting in the overproduction of ALA and PBG.
Recently, new insight into the etiology of the acute attacks came from several patients with AIP and VP who had chronic attacks that ceased after liver transplantation., Of note, domino transplantation of the porphyric livers into recipients with liver failure who did not qualify for transplantations, corrected their liver function, but made them susceptible to acute attacks. Thus, the debate was resolved. The acute attacks result from the hepatic production of a neurotoxic substance, presumably ALA and/or PBG that may interact with -aminobutyric acid or glutamate receptors.
Why Should Hematologists Know About Porphyrias
The porphyrias are a family of metabolic disorders caused by defects in the activity of one of the enzymes in the heme biosynthetic pathway leading to overaccumulation and excretion of porphyrin precursors in hepatocytes or erythroid cells, leading to extrahepatic or extramedullary cellular, tissue, and end-organ injury. The heme biosynthetic pathway involves 8 enzymatic steps and 7 committed intermediate porphyrin precursors that result in a protoporphyrin ring that incorporates iron to form the heme molecule. Hemoglobin and myoglobin use heme moieties to bind oxygen, and a number of other enzymes contain heme prosthetic groups that react with molecular oxygen and participate in electron transfer reactions.
As clinical hematologists we understand that elevated free protoporphyrin and zinc protoporphyrin are useful biomarkers of iron deficiency and lead poisoning. We might remember that lead inhibits ferrochelatase , the enzyme that catalyzes the insertion of ferrous iron into protoporphyrin IX , thereby allowing PPIX to incorporate zinc ions. We also learned that X-linked sideroblastic anemia is caused by mutations in the 5-aminolevulinate synthase 2 gene , which encodes the erythroid-specific isoform of the enzyme that initiates porphyrin production.
You May Like: Antiviral Medications For Hepatitis C
What Is An Acute Hepatic Porphyria
There are 4 acute hepatic porphyrias. They are characterised by recurrent acute attacks of severe neurovisceral abdominal pain.
The three autosomal dominant acute hepatic porphyrias are:
- Acute intermittent porphyria
- Variegate porphyria
- Hereditary coproporphyria
The presentation, initial diagnosis, and management of acute attacks are identical for AIP, VP, and HCP. Skin lesions can occur in variegate porphyria and hereditary coproporphyria, but do not occur in acute intermittent porphyria .
Delta aminolaevulinic acid dehydratase porphyria, a hepatic porphyria resulting from low levels of the enzyme delta-aminolevulinic acid dehydratase, has autosomal recessive inheritance with very few case reports in the literature and is not considered here.
How Is Porphyria Treated
Treatment for porphyria depends on the type of porphyria you have and your symptoms.
For people living with cutaneous porphyrias, avoiding sunlight is key to recovery. Your doctor may also recommend that you avoid substances, like alcohol, that trigger symptoms. Some people with cutaneous porphyria benefit from therapeutic phlebotomy . This type of blood draw reduces the amount of iron in the liver.
Treatment for acute porphyria involves intravenous heme or glucose infusions . These therapies decrease the number of porphyrins or porphyrin precursors produced in the liver. Other drugs are under investigation and may be available through clinical trials. Ask your doctor if a clinical trial is something to consider for your specific type of porphyria.
Dietary changes, including eating high amounts of carbohydrates and calorie-rich foods, also help manage symptoms.
Patients with acute porphyria who have severe symptoms or who have other types of porphyria may require more invasive treatments to manage symptoms. Treatment options may include blood transfusions, surgery to remove the spleen, and liver and bone marrow transplantation.
Don’t Miss: Hepatitis C Ab W Reflex To Hcv Rna Qn Pcr
The Hepatic Cutaneous Porphyria: Pct
PCT, the most common of the porphyrias, may be either sporadic or familial . For clinical symptoms to manifest in either type, the hepatic URO-decarboxylase activity must be 20% of normal or less. Type 1 PCT patients have no URO-decarboxylase mutations and, when asymptomatic, have normal URO-decarboxylase activity systemically. Type 2 PCT patients are heterozygous for UROD mutations, and asymptomatic patients have approximately half-normal enzyme activity systemically. Of note, although type 2 PCT is an autosomal dominant disease, it is incompletely penetrant the half-normal enzyme activity in type 2 patients is a significant predisposing factor but is insufficient by itself to cause symptomatic PCT. Other genetic and environmental factors contribute to susceptibility in both types 1 and 2 PCT. For this reason, penetrance of this genetic trait is low, and many patients who present with type 2 PCT have no family history of the disease and may appear to have sporadic disease. Although a diagnosis of PCT is usually made by a family physician, internist, and/or dermatologist the most common treatment for this disease is repetitive phlebotomies, so these patients are typically referred to hematologists. Phlebotomies are thought to decrease the hepatic iron load. An alternative oral treatment for PCT is low dose chloroquine treatment .