Treatment For Hepatitis C Related Glomerulonephritis
In the current understanding of HCV related glomerulonephritis , HCV is the infectious agent which cause GN. The renal disease shows injury from immune complex deposition and cryoglobulins. According to the recent AASLD/IDSA/IAS-USA hepatitis C guideline, HCV patients with type 2 or 3 essential mixed cryoglobulinemia and end-organ manifestations , proteinuria, nephrotic syndrome, or membranoproliferative glomerulonephritis are included in the highest priority for anti-HCV treatment due to the high risk for severe complications. Progressive renal disease, proteinuria to the extent of nephrotic syndrome and hypertension are the main manifestations of GN. Therefore a multi-prong approach to the management of HCV related GN involves controlling the clinical manifestations and protecting the kidneys, eradicating HCV, and also reducing the formation and deposition of HCV containing immune complexes in the glomeruli. Anti-hypertensive and anti-proteinuric medications are reno-protective agents, which will delay progression of renal disease while anti-hyperlipidemic therapy may also be required. Diuretics administered together with angiotensin converting enzymes inhibitors and/or angiotensin receptor blockers were proven to be effective.
Hepatitis C And Acute Kidney Injury
Acute kidney injury is when your kidneys stop working suddenly, within a very short period of time. Usually, if the cause of AKI is treated quickly, your kidneys will start working again. Sometimes hepatitis C can cause AKI, but this does not happen very often.
Hepatitis C is connected to AKI because:
- Hepatitis C can cause vasculitis. Vasculitis is the inflammation of blood vessels, arteries and veins. If the blood vessels of your kidneys get inflamed , this can cause acute kidney injury.
- In a few rare cases, some medicines for hepatitis C were connected to an increased chance of having AKI.
How Do You Know You Have Kidney Disease
You might not! Beyond the symptoms of hepatitis C, kidney-specific symptoms may or may not be present and it’s not unusual to have the silent disease, unbeknownst to the patient. As described above, patients could see blood in the urine, but that might not always be the case. Similarly, protein in the urine might not be apparent or be attributed to other ailments that you might have .
Needless to say, none of these findings are enough to confirm or refute hepatitis C-related kidney damage. However, a good healthcare provider will order tests of kidney function in a patient with hepatitis C, while a nephrologist managing a patient with any of the above telltale features should start looking for hepatitis C as a potential cause. Specifically, there are a few other tests which could be helpful:
- Testing for cryoglobulins
- Rheumatoid factor testing
- Testing the Complement levels
Since the disease happens at a microscopic level and can come in different variations, a kidney biopsy is often the only way to confirm what is going on.
Read Also: How Do You Contact Hepatitis C
What Is The Diagnosis Of Chronic Hepatitis
- In its most critical stages, cirrhosis can lead to death and liver failure unless a liver transplant can be done. The probability of developing cirrhosis depends on the severity of the disease and the response to treatment. When a biopsy shows more severe treatment, damage can be essential to help reduce the chance of developing cirrhosis even if you don’t have signs. Other factors that affect the prognosis include other medical illnesses, age, the subtype of the alcohol use and virus.
- Anyone with cirrhosis also has an enhanced prospect of developing liver cancer and must be screened regularly with an ultrasound examination and blood test of the liver. The risk of developing cirrhosis depends on the cause of hepatitis and the degree of inflammation. Signs and symptoms of cirrhosis may develop in fifteen per cent to thirty per cent of people who had chronic hepatitis infection for more than twenty years.
Read more on Miscellaneous
Antiviral Therapy In Ckd And Hemodialyzed Patients
The current recommendations for the initiation of antiviral therapy in CKD and dialysis patients are based upon similar factors as they are for the general population. The most important parameter in this regard seems to be the viral replication level . The critical level for therapy initiation has been proven to be 2,000 IU/ml. In some cases, the therapeutic decision should not be based on the HBV-DNA level alone. Additionally, the severity of liver disease should be considered, and the antiviral therapy should only be initiated if significant fibrosis or necroinflammatory activity is present . Therefore, antiviral therapy should be initiated in HBeAg-positive as well as in HBeAg-negative disease only if HBV-DNA 2,000 IU/ml therefore, HBV-DNA should be tested annually or in case of any unexplained ALT elevation . In HBeAg-negative disease, the replication may be present due to mutations in the BCP or pre-C regions of the HBV genome . These mutations block the secretion of HBeAg into the serum of the infected individuals.
The ideal objective of the treatment is the seroconversion to anti-HBs. This status is called closest to cure as at the molecular level, HBV infection is an incurable disease because cccDNA persists in the hepatocytes of every HBV-exposed person for their entire lives. The real aim of the treatment, which is achievable by the current treatment options, is the long-term suppression of HBV replication .
You May Like: Hepatitis B How Many Shots
How Common Is Hepatitis A
In the United States, hepatitis A has become relatively uncommon. After the hepatitis A vaccine became available in 1995, the rate of hepatitis A infections declined by 95 percent in the United States. The number of reported cases of hepatitis A fell to 1,239 in 2014, the lowest yearly number of cases reported since the disease could be tracked.1 However, the number of reported cases increased to 3,366 in 2017, almost 3 times higher, mostly due to outbreaks among people who use drugs and people experiencing homelessness.1 Early reports suggest that the numbers of cases and outbreaks of hepatitis A increased further during 2018 and continue at these higher rates in 2019.2
Hepatitis A is more common in developing countries where sanitation is poor and access to clean water is limited. Hepatitis A is more common in parts of Africa, Asia, Central and South America, and Eastern Europe than it is in the United States.
Is There A Link Between Hepatitis And Kidney Disease
World Hepatitis Day is coming up on July 28th. The aim of this event is to raise awareness about the disease because hundreds of millions of people worldwide are affected by viral hepatitis and many of them are undiagnosed. To help spread awareness among kidney patients, we are taking the opportunity to explore how hepatitis and kidney disease are linked.
You May Like: What Is Chronic Viral Hepatitis C
Chronic Kidney Disease Linked To Hepatitis B
Hepatitis B virus infection is associated with an increased risk of chronic kidney disease , according to a new study.
The study included 299,913 adults free of CKD at baseline who underwent health screening examinations from January 2002 to December 2016 in South Korea. In a fully adjusted model, individuals who tested positive for hepatitis B surface antigen had a significant 11% increased risk of incident CKD compared with those who tested negative, Yun Soo Hong, MD, of the Johns Hopkins University Bloomberg School of Public Health in Baltimore, and colleagues reported in BMC Nephrology. The investigators defined incident CKD as development of an estimated glomerular filtration rate below 60 mL/min/1.73 m2 and/or proteinuria.
HBsAG positivity was associated with a significant 23% increased risk of incident proteinuria and a non-significant 11% decreased risk of an eGFR below 60 mL/min/1.73 m2.
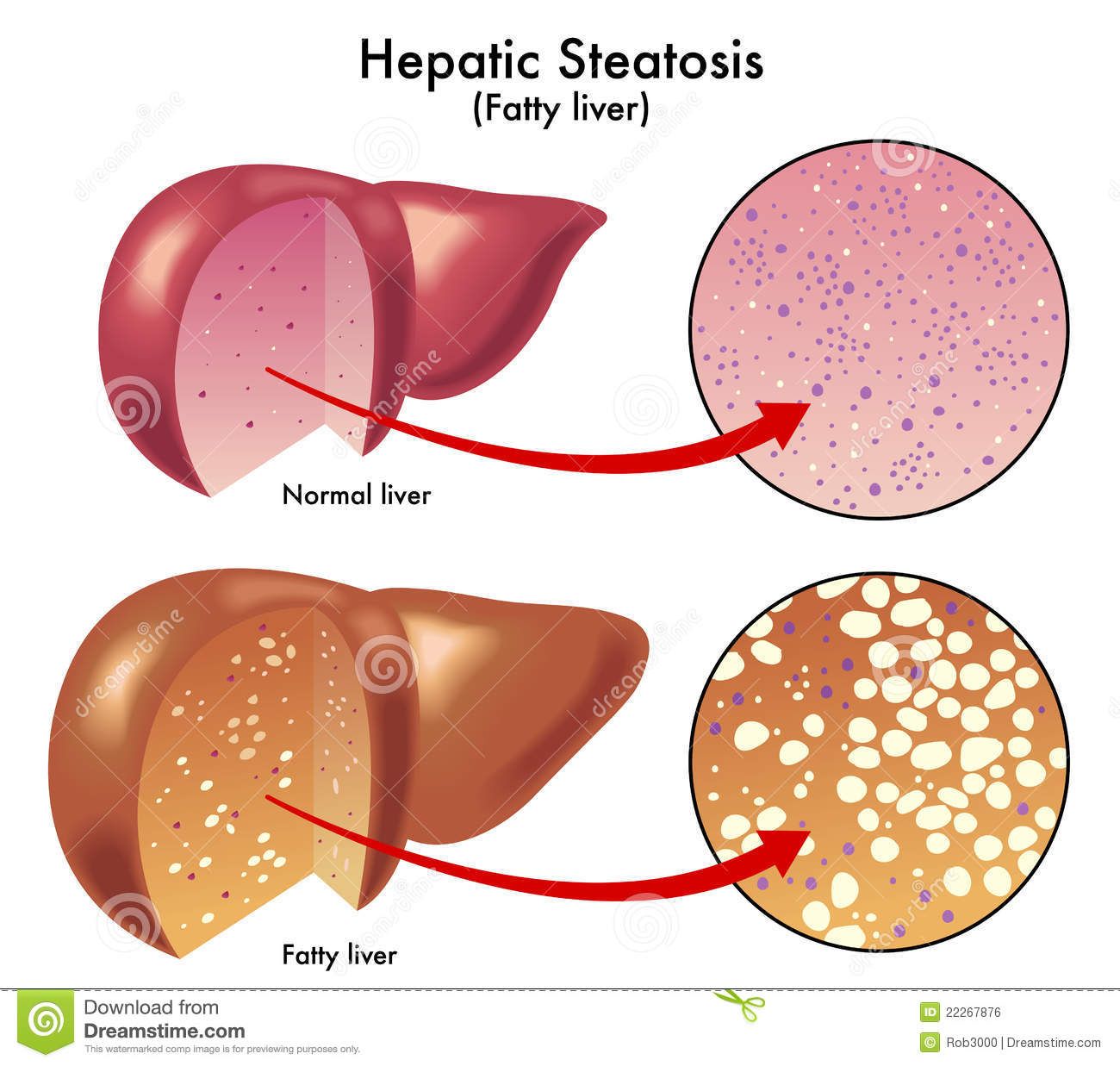
The investigators adjusted for age, sex, screening center, baseline eGFR, smoking status, alcohol consumption, education level, physical activity level, and the presence of hypertension, diabetes, and fatty liver disease.
Of the 299,913 study participants, 11,209 tested positive for HBsAG. These patients were significantly older than those who tested negative and more likely to be male . The HBsAG positive group also had a significantly higher proportion of current smokers .
Also Check: How Do You Get Autoimmune Hepatitis
What Does Hepatitis C Do To The Kidneys
Once the above mechanisms have been set in motion, the kidneys begin to get damaged. The most frequent site of damage is the kidney’s filter, called the glomerulus . This happens because the filter is essentially a microscopic ball of tiny blood vessels. As mentioned above, the hepatitis C virus does have a tendency to induce vasculitis, an immune injury to the blood vessels. This conglomeration of blood vessels inside the glomerulus is prone to a major hit.
Healthcare providers typically divide hepatitis C-related kidney disease into the following categories:
Don’t Miss: Chronic Hepatitis B Virus Infection
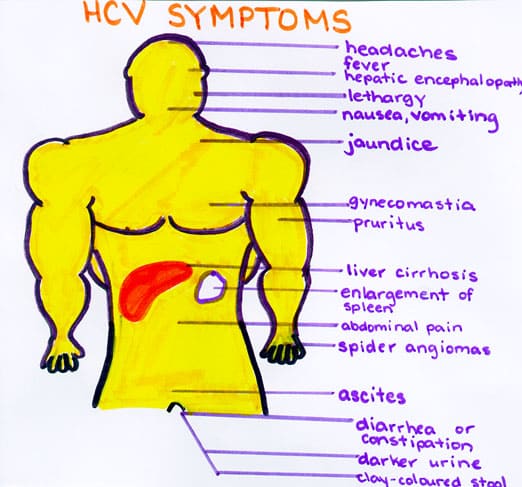
When Do Symptoms Develop
Many patients experience no symptoms and, for those who do, symptoms may not show up for years or even decades. Chronic liver disease in HCV-infected people usually progresses slowly without detection. Many times, HCV infection is not recognized until it is identified when people are screened for blood donations or through routine examinations.6 HCV is not routinely screened for in regular examination, so its important that someone who may have been exposed talk to a doctor. When left undiagnosed, HCV can lead to serious liver problems, including cirrhosis and liver cancer, and is the most common reason for liver transplantation in the United States.1
Outcomes Of Interest And Follow
The CKD was defined as having eGFR 60 mL/min/1.73 m2 or any urine protein/creatinine ratio 150 mg/g in 2 separate occasions three months apart. The eGFR was calculated by Chronic Kidney Disease Epidemiology Collaboration equation . Annual changes in eGFR were recorded for every patient. The developments of new CKD , absolute/relative changes of eGFR and percentages of patients having 50% decline of eGFR at 3rd years from the baseline were accurately recorded during the follow-up period.
Recommended Reading: What Are The Signs And Symptoms Of Hepatitis C
Read Also: What Does Hepatitis B Surface Antibody Ql Reactive Mean
Hepatitis C And Chronic Kidney Disease
Chronic kidney disease is when there is lasting damage to the kidneys that can get worse in time. Sometimes hepatitis C can cause CKD, but this does not happen very often.
Hepatitis C is connected to CKD because:
- Hepatitis C can cause a type of kidney disease called glomerulonephritis. Your kidneys are made up of thousands of tiny filters called glomeruli. Glomerulonephritis is the inflammation of the kidney filters , which causes permanent damage. When your kidney filters are damaged, this can lead to CKD.
- When you have hepatitis C, you have a higher chance of getting diabetes. Diabetes is the leading cause of kidney disease and kidney failure.
Since there is a connection between hepatitis C and kidney disease, doctors recommended that patients with hepatitis C be tested for kidney disease every year.
- If you have hepatitis C and kidney disease, your health may be worse than kidney patients without hepatitis C.
- Having hepatitis C can lead to a faster progression of CKD into kidney failure compared to people without hepatitis C.
This is why getting tested and treated for hepatitis C is so important for your health.
Demographic And Clinical Characteristics Of The Study Participants
A total of 2,435 subjects completed the survey and examination in this study. The mean age was 50.3±10.3 years, and 52.5% of patients were women. The study subjects were divided into four groups based on the types of viral hepatitis, according to the following distribution: HCV infection , HBV infection , HBV/HCV co-infection , and uninfected controls . The demographic and clinical characteristics of the study subjects in the four groups are summarized in Table . The HCV infection group had an older mean age , higher rates of diabetes mellitus and CKD , and higher levels of hemoglobin , alanine aminotransferase , total bilirubin , serum urea nitrogen , and serum creatinine compared to the HBV group, which had a mean age of 46.0±10.2 years and CKD prevalence of 19.7%. Notably, the uninfected control group had higher levels of platelets , albumin , triglycerides , and cholesterol compared with the HCV infection, HBV infection, and HBV/HCV co-infection groups.
Table 1 Baseline characteristics of chronic hepatitis patients and controls.
You May Like: How Can You Contact Hepatitis B
Patients With Renal Impairment
Chronic hepatitis C is independently associated with the development of chronic kidney disease . A meta-analysis demonstrated that chronic HCV infection was associated with a 51% increase in the risk of proteinuria and a 43% increase in the incidence of CKD . There is also a higher risk of progression to end-stage renal disease in persons with chronic HCV infection and CKD, and an increased risk of all-cause mortality in persons on dialysis .
Successful HCV antiviral treatment improves clinical outcomes. Antiviral therapy was associated with a survival benefit among persons on dialysis in a nationwide Swedish registry study . In a retrospective cohort analysis utilizing the Truven Health MarketScan Database , HCV treatment was associated with a 30% decreased risk of developing CKD . Persons with HCV infection experienced a twofold and a 17-fold higher risk of membranoproliferative glomerulonephritis and cryoglobulinemia , compared with persons without HCV .
Assessment Of Hepatitis C And Liver Disease Status In Renal Patients
The clinical tools used in assessing HCV and the liver disease in non-uremic patients are generally applicable to renal patients apart from a few notable differences. HCV infected patient on hemodialysis tend to have normal alanine transaminase possibly due to high lactate level, which cause rapid consumption of NADH co-enzyme or enzyme during dialysis.
All anti-HCV-positive CKD patients should be assessed for HCV RNA viral load, HCV genotyping as well as liver fibrosis. HCV genotype is a strong predictor of response to anti-HCV treatment. KDIGO recommended special steps in drawing blood sample for HCV RNA tests in hemodialysis patients because heparin is an inhibitor of polymerase chain reaction. In order to avoid contamination with heparin which is used in hemodialysis session, the blood sample for HCV RNA should be taken from a peripheral vein before the dialysis session.
We look into several studies that analysed liver biopsy findings in this group of patients. These studies revealed that about 22%-81% of HCV positive ESRD patients had histological evidence of liver fibrosis on biopsy while a smaller percentage of approximately 13%-25% had biopsy proven cirrhosis.
Patients with clinical or histological evidence of cirrhosis should have further assessments to look for the complications of cirrhosis such as upper endoscopy for varices and liver ultrasound for hepatocellular carcinoma surveillance.
Recommended Reading: Hepatitis B Surface Antibody Qualitative
Antiviral Therapy In Kidney Transplant Recipients
Posttransplant administration of IFN-α to HCV-positive recipients with liver disease and stable renal function improved liver function in 50% of patients, and led to negative HCV RNA in 25% of cases .
A meta-analysis of 12 trials of IFN-based therapy in 102 kidney transplant patients showed that SVR response was very heterogeneous, ranging from 0% to 50%, and the rate of drop-out was remarkably high . Even in the kidney transplant settings, the SVR response to antiviral therapy depends upon the HCV genotype, HCV1 being the more resistant . The beneficial effect on liver disease can, however, be associated with 15% to 60% increased risk of acute cellular or vascular rejection, and the rate of graft loss may rise up to 20% . Graft rejection is frequently irreversible and steroid-resistant . Induction of cell surface expression of HLA alloantigens, intracellular cytokine gene expression, as well as increase in antibody production by B cells are possible mechanisms through which IFN may trigger acute graft rejection .
However, after discontinuation of the therapy a rebound of the HCV viral load to pretreatment levels was documented . It has therefore been recommended to avoid IFN in HCV-positive renal transplant patients because of the potential to precipitate graft rejection or the relapse of infection upon drug withdrawal.
Liver Disease Rash: A Symptom And A Sign
What is a liver disease rash?Dermatologists find that our skin often shows what is happening inside of the body. A liver disease rash could indicate a further health problem. An example of where this effects your liver would be jaundice, where the skin and the whites of the eyes become yellow. Although yellowing skin is not the only skin change that indicates liver disease, darkening of the skin and bronzing of the skin can point to liver disease or failure and rashes can point to a number of liver health problems.
Whats in this article
A liver disease rash and hepatitis C
Skin rashes may be a sign of hepatitis C, and should not be ignored. Rashes that appear on your skin as a result of hepatitis c show that your body is busy trying to fight the infection on its own. This rash is called urticaria and is the most common rash for those suffering from acute hepatitis c virus. This is a short-term infection, according to the National Digestive Diseases Information Clearinghouse, acute HCV typically lasts for six months or less. Urticaria can also cause the skin to swell, rashes on your face and often comes in rounds that can last for several hours. Urticaria can also develop as a result of certain allergic reactions.
Signs & symptoms
If a rash is due to liver damage skin symptoms may include:
Additional symptoms may include stomach swelling and bleeding that does not stop.
Also Check: Blood Test For Hepatitis C Screening