Treatment Of Acute Asymptomatic Hepatitis B
As with influenza virus infection, treatment could be used to ameliorate the course of disease rather to prevent chronic infection. Only a minority of patients with acute hepatitis B will even come to medical attention due to the mostly relatively indolent course for most patients however, a few may develop more serious to even fatal disease. It is also important to note that anyone with evidence of HBV exposure might be at risk of HBV reactivation in situations of immunosuppression such as therapy with biologics or chemotherapy .
Treatment Of Cirrhotic Patients
The main goal of antiviral therapy in hepatitis B virus carriers with advanced liver disease is to suppress viral replication to HBV DNA levels that are persistently undetectable by a PCR-based sensitive method . Achievement of SVR is associated with lower incidence of progression to liver disease and hepatocellular carcinoma and increases liver transplant-free survival. However, the risk of developing HCC is not zero and periodical screening should be maintained indefinitely, even after long periods of SVR and even despite improvement in noninvasive hepatic fibrosis test results.
Limited evidence exists of the impact of antiviral therapy on the evolution of patients with compensated cirrhosis and serum HBV DNA levels less than 2000 IU/mL. However, indirect evidence suggests that cirrhotic patients with a viral load less than 2000 IU/mL are at an increased risk of developing HCC. In addition, a beneficial effect of antiviral therapy on the risk of HCC was observed in these patients.
Recommendations
1 Treatment of hepatitis B should only be indicated after 612 months of monitoring ALT levels and viral load .
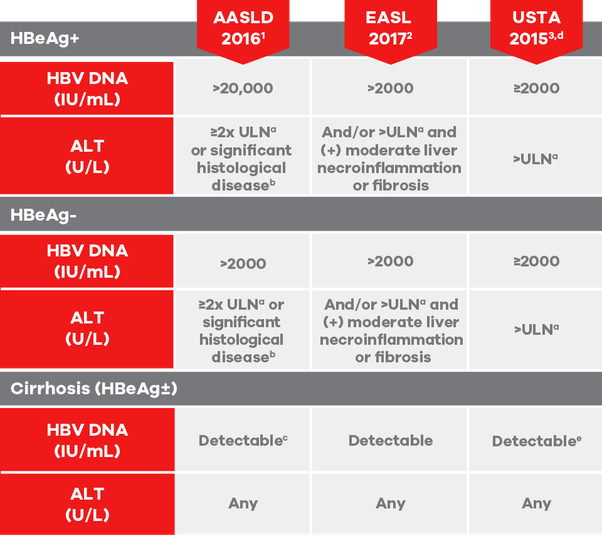
2 Treatment of hepatitis B is recommended for all patients with evidence of HBeAg-positive or -negative immunoactive disease .
3 Immunoactive disease is characterized by ALT > ULN, HBV DNA > 200020,000 IU/mL and evidence of histologically significant disease .
References
Recommendations
Clinical Guidelines For Children With Chronic Hepatitis B
In general, the clinical guidelines for children are the same as for adults – visits are usually scheduled every six months or once a year. Most children do not need drug treatment, but they still need to be monitored regularly to make sure they remain healthy and to detect any problems with their liver as soon as possible. Visits will include a physical exam, blood tests, and possibly an imaging study of the liver .
AASLD guidelines provide guidance for treating children under the Updated Recommendations on the Treatment of Patients With Chronic Hepatitis B, section 9A.
The Hepatitis B Foundation convened the first Pediatric HBV Workshop and invited the nations leading pediatric liver specialists to develop the first national recommendations for children living with hepatitis B to ensure that they receive the best care possible. These recommendations have been published in highly respected, peer-reviewed journals and provide expert guidance for the care of infected children.
Hepatitis B Foundations Clinical Guidelines for Pediatric HBV
HBF’s Pediatric HBV Screening and Monitoring Recommendations Published in Pediatrics in November 2009Haber BA, Block JM, Jonas MM, Karpen SJ, London WT, McMahon BJ, Murray KF, Narkewicz MR, Rosenthal P, Schwarz KB. Recommendations for screening, monitoring, and referral of pediatric chronic hepatitis B. Pediatrics 124:e1007-13.
You May Like: Do I Have Hepatitis B
What Is Involved In A Liver Transplant
A liver transplant is considered necessary when the liver is damaged and cannot function or in some cases of liver cancer. Your liver is very important. It is responsible for many functions related to making sure that your body stays healthy and is able to digest foods.
You may be eligible for a transplant if you have chronic hepatitis B infection or some of the diseases that may result from it, including liver cancer and cirrhosis. You will have to complete testing and be evaluated before being approved for a transplant. It is likely that you will be placed on a waiting list while an appropriate organ is found.
Donated livers come from two types of donors: living and deceased. Because the liver can regenerate, it is possible to use part of a liver for transplant. The remaining sections in both the donor and the receiver will grow into livers of adequate size.
People who get liver transplants must take anti-rejection drugs for the rest of their lives. These drugs make you more susceptible to infection. However, liver transplants have become more successful over time and continue to improve.
Hbv Primary Care Workgroup
The HBV Primary Care Workgroup includes members in the United States from hepatology, infectious diseases, pharmacy, primary care, and public health. The 2020 HBV Primary Care Workgroup Guidance was first released in early 2020 and is accessible on this web site , with the aim to have regular updated versions posted online. The goal of this document is to provide simplified, up-to-date, and readily accessible HBV management guidance for primary care medical providers. Note, this guidance does not incorporate HBeAg status in the initial decision-making process, but persons positive for HBeAg are recommended to undergo monitoring of HBeAg for evidence of HBeAg seroconversion. The 2020 HBV Primary Care Workgroup Guidance recommends initiating HBV treatment in the following situations.
- : Treatment is recommended but persons should be promptly referred to a hepatologist.
- Cirrhosis: Treatment is recommended for all persons with cirrhosis, regardless of HBV DNA level, ALT level, or HBeAg status.
- Without Cirrhosis: For persons without cirrhosis, treatment is recommended if the HBV DNA level is greater than 2,000 IU/mL and the ALT level is elevated, regardless of HBeAg status. For this purpose, elevated ALT is defined as greater than 25 U/L in females and greater than 35 U/L in males that is persistent for at least 3 to 6 months.
You May Like: Types Of Hepatitis B Virus
Overview Of Hbv Serological Markers
There are two figures in this module that provide an overview of hepatitis B serological markers. The first figure is a line graph showing changes in serological markers for acute infection with spontaneous recovery from 0 to 100 weeks after exposure. Hepatitis B surface antigen begins to rise just before 4 weeks after exposure, peaking at less than 12 weeks, after which, it falls to zero at 24 weeks. Hepatitis B e-antigen is present until just after the peak in hepatitis B surface antigen levels at 12 weeks. After this point, hepatitis B e-antigen disappears and hepatitis B e-antibody appears. Symptoms are present when hepatitis B surface antigen reaches its peak and during its decline. The IgM marker of the hepatitis B core antibody begins to rise around 6 weeks after exposure, peaks just before 16 weeks and then declines to zero at 32 weeks. Total hepatitis B core antibody also starts to rise around 6 weeks, then plateaus at about 20 weeks. Hepatitis B surface antibody begins to rise just before 32 weeks, peaks after 36 weeks and then declines.
Chronic Hepatitis B
World Health Organization Recommendations
The 2015 WHO guidelines for the prevention, care, and treatment of persons with chronic hepatitis B infection indicates treatment priority for individuals of all ages who have chronic hepatitis B infection and clinical evidence of compensated/decompensated cirrhosis , regardless of their levels of ALT or HBV DNA, or their HBeAg status.
Treatment is recommended for adults with chronic hepatitis B infection without clinical evidence of cirrhosis , but who have all of the following features , and regardless of HBeAg status :
- Are older than 30 years
- Have persistently abnormal ALT levels
- Have evidence of high-level HBV replication .
In individuals with HBV/human immunodeficiency virus coinfection, the AASLD recommends initiating ART in all those with evidence of severe chronic liver disease, regardless of CD4 count, as well as those with a CD4 count of 500 cells/mm3 or below, regardless of their liver disease stage.
However, the AASLD does not recommend antiviral therapy, indicating it can be deferred, in individuals with all of the following , regardless of HBeAg status or age :
- No clinical evidence of cirrhosis
- Persistently normal ALT levels
- Low levels of HBV DNA replication . ]
Also Check: Hepatitis C Causes Liver Damage
What Is Immune Tolerance
Generally, immune tolerance is defined as the specific non-response state of the immune system after receiving specific antigen. The liver has a unique immune regulation function, which can promote the tolerance to HBV, and this may be the main reason of HBV persistence and chronic infection. In 1972, Dudley et al. firstly proposed that HBV persistent infection was related to immune tolerance, and the liver injury was determined by T cell-mediated immune response . In 1983, Liaw et al. reported that HBeAg clearance was related to the enhancement of host immune response . Based on the above findings, Chu et al. firstly divided the natural history of HBV infection into three phases of immune tolerance, immune clearance, and residual integration , and then divided it into four phases of immune tolerance, immune clearance, inactive carrier status and reactivation . The latter four phases are the current widely used classification of hepatitis B natural history.
Also Check: What Is The Treatment For Hepatitis B
How To Define The Immune Tolerance Phase Of Hbv Infection
The immune tolerance phase of HBV infection has been defined and described in many international CHB management guidelines . Although these guidelines have some differences in the definition of immune tolerance phase of HBV infection, they also have common characteristics, such as positive HBsAg , positive HBeAg, high level of HBV-DNA , persistently normal ALT , as well as no obvious inflammation, necrosis and fibrosis in liver pathology.
At present, the inconsistent definition of immune tolerance phase in different guidelines is mainly manifested in the level of serum HBV DNA and ALT. Because of the controversy in serum HBV DNA and ALT levels, clinicians must pay attention to following details when judging a chronic HBV infection whether in the immune tolerance phase. Firstly, the guidelines require that patients serum ALT level is persistently normal, rather than a certain cross-sectional serum ALT within the normal range. Therefore, in clinical practice, we need patients to provide reliable laboratory reports of dynamic serum ALT and comprehensively evaluate various potential factors that may cause ALT level fluctuations. Secondly, on the premise of meeting other conditions, the higher the serum HBV-DNA level, the more likely the patient will be in the immune tolerance period. Because only the very high serum HBV DNA level can accurately indicate the peaceful coexistence of the virus and the host.
Don’t Miss: Where Can I Get Tested For Hepatitis B
About The Hbv Primary Care Workgroup
This guidance was developed by the Hepatitis B Primary Care Workgroup, a multidisciplinary panel of national experts in the field of viral hepatitis B, including representation from hepatology, infectious diseases, pharmacy, primary care, public health, and other national organizations. The workgroup was organized by the National Taskforce on Hepatitis B in partnership with the San Francisco Hep B Free Bay Area and Project ECHOTM and did not receive any outside funding.
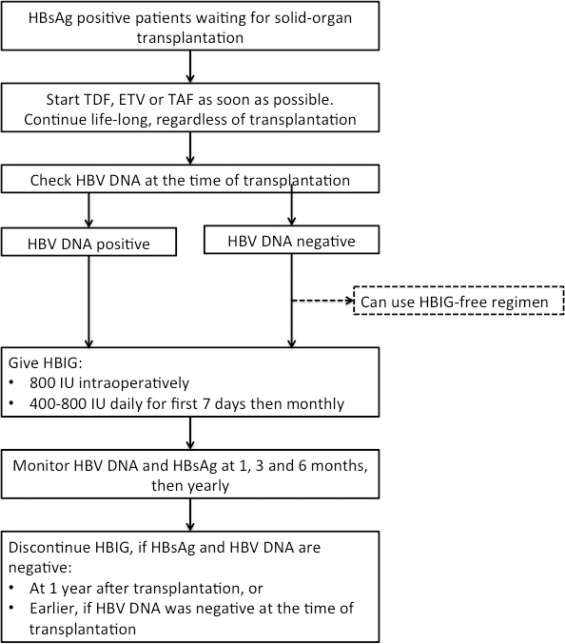
Hepatitis B And Liver Transplantation
Antiviral therapy usually prevents the need for liver transplantation in patients with hepatitis B, even in advanced stage. Nevertheless, decompensated cirrhosis remains an important indication for this procedure. Hepatocellular carcinoma detected in the cirrhotic liver is another common indication.
After transplantation, prophylactic treatment should always be implemented in these patients in order to reduce the risk of HBV recurrence in the graft, ensuring better survival rates of the patient and of the graft. This strategy reduces the rate of reinfection in the transplanted organ to less than 510%. Antiviral therapy with potent nucleoside/ nucleotide analogs such as entecavir, tenofovir or tenofovir alafenamide prevents the recurrence of infection after transplantation but the drugs should be maintained indefinitely.
Most liver transplant centers in the world use anti-HBV immunoglobulin during the early post-transplant period, with variable doses and durations depending on each center. In patients at high risk of HBV recurrence during the post-transplant period , combination therapy, i.e., HBIg combined with a potent NUC, should be initiated and continued indefinitely.
References
Coffin, C. S et al. Virologic and clinical outcomes of hepatitis B virus infection in HIV-HBV coinfected transplant recipients. Am J. Transplant 2010: 10: 1268 -1275.
Read Also: When Was Hepatitis D Discovered
Specific Therapy For Acute Hepatitis Delta Virus Infection
Since the start of vaccination against HBV, a decline in the incidence of acute hepatitis delta virus infection has been observed in many regions . HDV requires ongoing expression of HBV surface genes to be able to infect a host, but it does not require HBV replication. Simultaneous coinfection with both HBV and HDV is associated with more severe disease and higher risk for fulminant hepatitis than acute HBV alone however, HDV superinfection may also present as acute hepatitis . In general, coinfection is more likely to lead to severe acute presentation, but rarely leads to chronicity, while superinfection of HDV usually leads to chronicity . For example, 2 of 218 HDV coinfected patients but none of 128 HDV superinfected patients died from consequences of acute hepatitis .
Chb Immune Tolerant Phase
Previously, most practice guidelines did not recommend antiviral therapy for CHB patients in the immune tolerant phase . Recent data regarding the treatment of CHB patients in the immune tolerant phase suggest that the risk of progression to liver cirrhosis and HCC development could be reduced by antiviral therapy . Therefore, patients needing treatment should be differentiated from truly immune tolerant CHB patients who do not require antiviral therapy. However, initiation of antiviral therapy for patients in the immune tolerant phase remains very controversial further studies are needed to appropriately define the immune tolerant phase, as discussed above.
Read Also: Who Needs To Be Tested For Hepatitis C
What Are The Risk Factors For Getting Hepatitis B
Due to the way that hepatitis B spreads, people most at risk for getting infected include:
- Children whose mothers have been infected with hepatitis B.
- Children who have been adopted from countries with high rates of hepatitis B infection.
- People who have unprotected sex and/or have been diagnosed with a sexually transmitted infection.
- People who live with or work in an institutional setting, such as prisons or group homes.
- Healthcare providers and first responders.
- People who share needles or syringes.
- People who live in close quarters with a person with chronic hepatitis B infection.
- People who are on dialysis.
How Common Is Hepatitis B
Hepatitis B is fairly common in Africa and the western Pacific region. Throughout the world, there are about 292 million people who are infected with chronic hepatitis B. In the U.S., the figure exceeds 2 million people.
The number of infections had been falling in the U.S., but fewer vaccinations among adults combined with the onset of the opioid crisis and injected drug usage has resulted in the numbers rising again. Infected women can pass the infection on to their babies. Children who are infected before age 5 are more likely to have chronic infection than those infected later in life.
Read Also: What Are The Early Signs Of Hepatitis C
Treatment For Acute Hepatitis B
Acute HBV infection has in the past been associated with a number of extrahepatic manifestations. Most of these are believed to be related to immune complex formation with either HBeAg or HBsAg. Therefore, one might consider interferon-based therapies to be potentially more effective than purely antiviral therapies interferon also has been associated with stronger reduction of HBeAg and HBsAg than pure antivirals. Some recent papers, however, have also reported success with direct antiviral therapy, which remains the only option for interferon intolerant patients.
Interestingly, as acute HBV infections decrease, patients presenting with extrahepatic manifestations due to acute HBV infection are also seen less frequently . In our experience, we do not recall any patient with acute hepatitis and significant extrahepatic manifestations such are renal disease of polyarteritis nodosa. Still, it is important to be aware that HBV may be associated with extrahepatic diseases.
Interestingly, while HCV is associated with membranoproliferative glomerulonephritis, glomerulopathies associated with HBV were found to be dominantly membranous glomerulopathy .
Another manifestation reported with HBV is Gianotti-Crosti syndrome. This is a syndrome of skin eruption described as papular acrodermatitis. It is mostly limited to children and not limited to HBV, but reported with acute HBV infection .
Deterrence And Patient Education
Patient education remains one of the most important components in preventative measures regarding HBV infection.
Education should be provided to expecting parents about the importance of vaccination and to clarify erroneous beliefs about vaccinations.Patient education should also include counseling about the avoidance of risky behaviors that predispose an individual to be infected, including promiscuous sexual activity or intravenous drug abuse. They should also be advised not to share items such as shaving razors, toothbrushes, or hair combs due to possible transmission via mucosal contact or through microtrauma to protective barriers.
Recommended Reading: How You Get Hepatitis B And C
Resolution Time And Clinical Course Of Infection
The majority of immunocompetent adults will recover within 6 months and develop lifelong immunity the remainder will be chronically infected. Immunocompromised adults are at a particular risk of developing chronic infection. The risk of developing chronic infection is also much higher for those who acquired the infection in infancy or before 7 years of age .Endnote 3, Endnote 13, Endnote 14
Acute HBV does not require antiviral treatment. Management should focus on relief of symptoms, monitoring and prevention of hepatic complications, as well as counselling aimed at preventing transmission. Persistence of HBsAg for 6 months indicates chronic infection.
Baseline laboratory testing to assess liver function and screen for other infections:
- Bilirubin , albumin, INR , creatinine
- Testing for STIs, including HIV, and for HCV, where appropriate
- Repeat HBsAg at least 6 months after baseline, to confirm / rule out chronic infection. . See Module 6 for additional testing recommendations for those with confirmed chronic HBV