Diagnosis Of Hepatitis B In Hiv Infection
It is important to accurately diagnose and assess the state of HBV infection in the HIV-infected individual because therapeutic management is dependent on the correct diagnosis and staging . All patients who are HIV-infected should be screened for hepatitis B with tests for HBsAg, anti-HBs, and antibody to hepatitis B core antigen . Those persons who are negative for anti-HBs and HBsAg are at risk for acquiring HBV and should receive the HBV vaccine. Those who are diagnosed with chronic hepatitis B, as marked by the presence of HBsAg for at least 6 months, should have their disease stage evaluated with testing for HBeAg, antibody to HBeAg , HBV DNA, serum ALT, bilirubin, albumin, prothrombin time, and platelet count.
Can Hbv Infection Be Prevented
Yes. The best way to prevent HBV is to get the hepatitis B vaccine.
CDC recommends that people with HIV and people who are at risk for HIV get the HBV vaccine . The housemates and sexual partners of people with HBV should get the HBV vaccine, too.
People, including people with HIV, can also take the following steps to reduce their risk of HBV infection:
- Use condoms during sex to reduce the risk of HBV infection and infection with other sexually transmitted diseases, such as gonorrhea and syphilis.
- Do not inject drugs. But if you do, do not share needles, syringes, or other drug injection equipment.
- Do not share toothbrushes, razors, or other personal items that may come in contact with another person’s blood.
- If you get a tattoo or body piercing, make sure the instruments used are sterile.
Type 2 Diabetes Linked To Decreased Physical Functioning Among Men With And Without Hiv
Want to receive publications straight to your inbox?
- As people with HIV live longer they become at risk for health conditions such as Type 2 diabetes
- A U.S. study with 2,240 men found that the risk of diabetes was similar regardless of HIV status
- The effects of diabetes on hand grip strength were lower among participants with HIV on antiretroviral treatment
Combination drug treatment for HIV is highly effective when used as prescribed. In the average person, several months after initiating ART, HIV levels fall so low that they cannot be detected with routinely used lab tests. This suppression of HIV while on ART usually allows the immune system to effect repairs, and the result is a significantly reduced risk for AIDS-related infections and cancers. The power of ART is so profound that researchers predict that many ART users will have near-normal life expectancy.
As people with HIV age, their risk for other health conditionssuch as cardiovascular disease and Type 2 diabetesincreases.
You May Like: Can You Get Rid Of Hepatitis B
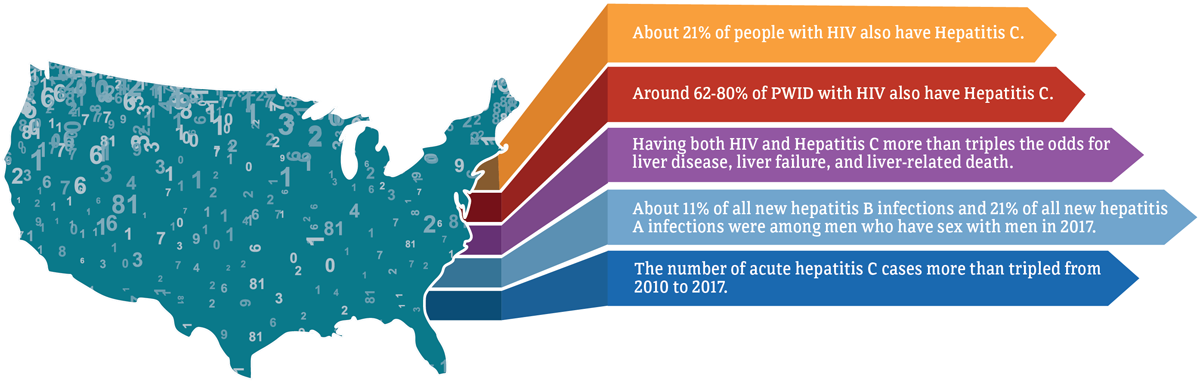
Initial Evaluation And Treatment Recommendations For Patients With Hepatitis C Virus/hiv Coinfections
Prior to initiating ART, screen patients with HIV infection for HCV using sensitive immunoassays licensed for the detection of antibody to HCV in blood to confirm the presence of chronic infection, persons who are HCV seropositive should be tested for HCV ribonucleic acid using a qualitative or quantitative assay.
Advise patients with HCV/HIV to avoid alcohol and receive HAV and HBV vaccines, if screened negative via serology.
Drug-induced liver injury following ART is more common in HIV/HCV coinfection eradication of HCV infection may decrease the likelihood of antiretrovirus-associated DILI.
It is important to monitor alanine aminotransferase and aspartate aminotransferase levels at 1 month and then every 3 months after the initiation of ART.
ART should be started in persons co-infected with HCV and HIV in accordance with the recommendations for initiating ART in treatment-naive patients. ART should be started at least 4-6 weeks before hepatitis C treatment is initiated.
The objective of HCV antiviral treatment is to cure the HCV infection, reflected by a sustained virologic response. Although patients with HIV and HCV coinfection traditionally had lower response rates to HCV treatment with older regimen of ribavirin and peginterferon compared to individuals without HIV infection, patients with coinfection appear to have comparable sustained virologic response rates with all oral, direct-acting antiviral combination therapy.
Risk For Hepatocellular Carcinoma
Risk assessment: Hepatocellular carcinoma is a major cause of death in patients with chronic HBV infection, and all patients with HIV should be assessed for the risk of HCC. However, determining an individuals risk can be challenging. According to guidelines from the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver , the patient populations listed below are at high risk for HCC.
Patients at high risk for hepatocellular carcinoma, per AASLD and EASL guidelines :
- Asian men over 40 years and Asian women over 50 years of age
- Black patients over 20 years of age
- Patients over 40 years of age with persistent or intermittent serum ALT elevation and/or HBV DNA level > 2000 IU/mL
- Patients with cirrhosis including those awaiting transplantation
- Patients with a family history of HCC
- Patients with chronic HCV infection and advanced liver fibrosis
Nomograms have been published to assist in determining whether an individual patient should undergo surveillance for HCC . These nomograms can be used to predict an individuals risk for HCC based on known risk factors, including age, sex, alcohol intake, family history of HCC, elevated serum ALT level, presence of HBeAg, HBV DNA level, and HBV genotype.
| KEY POINT |
|
References
Recommended Reading: How To Get Hepatitis B
Immune Response To Hcv And Pathogenesis
Acute HCV mono-infection
Early after HCV infection, an innate immune response is evident in the liver and in the blood, featuring induction of antiviral proteins, notably the type 1 IFNs, IFNα and IFNβ. This leads to expression of many IFN-stimulated genes with antiviral properties . In addition to the ISG response, NK cells are activated in acute HCV infection and display markers of cytotoxicity .
In parallel with the innate response, viral antigens are processed by immature DCs to initiate adaptive immune responses, involving both CD4+ and CD8+ T cells . An association between HLA class II genotype and HCV clearance suggests that CD4+ T cells are critical . Consistent with this notion, early, vigorous, and sustained CD4+ T-cell proliferative responses against multiple HCV proteins have been shown to predict disease resolution . In addition, depletion of CD4+ T cells before re-infection of chimpanzees resulted in persistent, low-level viremia, despite functional intra-hepatic CD8+ T-cell responses . Similarly, in both human and chimpanzee studies, strong and broadly targeted HCV-specific CD8+ T-cell responses have been consistently associated with clearance of primary infection . These findings argue for a cooperative role for both CD4+ and CD8+ T cells in facilitating clearance .
Chronic HCV mono-infection
Hepatic fibrosis
Epidemiology And Global Burden Of Disease
The World Health Organization has estimated that approximately 14 million people worldwide have HIV and Mycobacterium tuberculosis co-infection and that TB is the most common opportunistic infection in individuals with HIV infection, accounting for about 26% of acquired immunodeficiency syndrome -related deaths. In 2010, the WHO estimated that 39% of new TB cases occurred in people with HIV co-infection .
Also Check: Is Hpv Vaccine Same As Hepatitis B
A Hiv Replication In The Liver
A number of studies have shown various cell types in the liver are permissive to HIV infection in vitro including HSC, Kupffer cells and hepatocytes . HIV infection of these cells has also been demonstrated in vivo in individuals naïve to ART and HIV sequences from the liver in individuals off ART have distinct compartmentalised sequences when compared to other tissue sites . There have been few studies to determine whether HIV persists in the liver on ART but studies of animal models, including SIV-infected macaques and HIV-infected humanized mouse models both suggest that HIV can persist in the liver on ART, primarily in Kupffer cells . Recently, infectious replication competent HIV was isolated from Kupffer cells obtained from liver at autopsy from three HIV-infected individuals who died on ART .
In the absence of virus replication on ART, HIV may also contribute to liver inflammation and fibrosis by binding of gp120 to CXCR4 which is expressed on hepatocytes and HSC . The effect of HIV infection and or HIV proteins in the liver has primarily been studied in the context of HIV-HCV co-infection in vitro but not in HIV-HBV co-infection. HIV infection alone, or in the presence of HCV, induced profibrotic processes in hepatocyte and HSC cell lines including increased chemokine production, HSC migration, hepatocyte apoptosis and expression of profibrotic genes .
What To Start Therapy With When Haart Is Initiated
As described above, if HIV therapy is initiated with tenofovir and emtricitabine as part of an anti-HIV regimen, then additional anti-HBV drugs are not needed because this combination is potent . This is also the best option in patients who may have or are known to have lamivudine-resistant hepatitis B. In a randomized controlled trial from Thailand, 36 HIV-HBV coinfected subjects were randomized to receive either lamivudine, tenofovir, or the combination of tenofovir and lamivudine. At the end of 48 weeks, the average decline in HBV DNA was similar in all three arms, ranging from 4.07-4.73 log10 copies/mL. However, suppression of HBV DNA levels to < 1000 copies/mL was more frequent in the two tenofovir-containing arms compared to the lamivudine arm . Drug resistance developed in only two patients, both of whom were in the lamivudine-only arm. In a cross-sectional study from a lamivudine-experienced HIV-HBV coinfected cohort from Australia and the United States, subjects who received a combination of tenofovir with emtricitabine or lamivudine were more likely to have HBV DNA < 100 IU/mL than those receiving either tenofovir or lamivudine monotherapy. The combination group was also significantly less likely to have HBV DNA > 200,000 IU/mL. The limitation of this study is that it was cross-sectional rather than prospective, but it provided some evidence that combination therapy was superior to monotherapy in HIV-HBV coinfected subjects with lamivudine-resistant HBV.
You May Like: Is There Medicine For Hepatitis B
Impact Of Cart Including Ird
The CD4+ T-cell dependence of anti-malaria antibodies suggests that restoration of CD4+ T-cell counts in HIV-infected individuals with cART will improve acquired immunity to malaria. However, recent research has suggested that cART does not improve innate immune responses to malaria . There are few studies on the efficacy of cART in preventing severe malaria in children or adults and non-specifically addressing this question in pregnant women. A prospective study of HIV-infected adults in Uganda receiving either co-trimoxazole prophylaxis alone or in combination with antiretroviral drugs and insecticide treated bed-nets, showed that the frequency of clinical malaria was decreased in individuals receiving cART plus co-trimoxazole compared to those receiving co-trimoxazole alone . While treatment was not randomized in this observational study, the analysis adjusted for CD4+ T-cell levels, age, and sex. There are no reported cases of malaria IRD possibly because protective immune responses are humoral rather than cellular.
Other Causes Of Liver Disease Top Of Page
It should be recognized that liver disease in patients with HBV-HIV coinfection can be from causes other than HBV, including other viral infections , alcohol, medications, HAART-related hepatotoxicity, and nonalcoholic fatty liver disease . Abnormal liver enzymes in HBV-HIV coinfected patients may be due to any of these factors, as well as the development of drug resistance or reactivation of HBV.
| Table 4. Differential Diagnosis of Liver Abnormalities in Patients with HBV-HIV Coinfection. |
| hbv |
Recommended Reading: Hepatitis C Flare Up Symptoms
Assessment For Inflammation And Fibrosis
As part of the initial evaluation of patients with HIV/HBV co-infection, liver biopsy is considered the gold standard to assess fibrosis and inflammation and to stage chronic disease. Ultrasound of the liver can sometimes detect cirrhosis and steatosis, and triple-phase computed tomography can be used during the initial assessment to detect HCC. However, because patients with HIV are at higher risk for fibrosis, liver biopsy may be prudent for patients with HIV/HBV co-infection with normal serum ALT or low HBV DNA levels who are considering deferral of anti-HBV therapy or who also have HCV.
Liver stiffness measurements and calculations of a fibrosis score from noninvasive tests, such as serum ALT level and platelet count, as well as the biomarker test known as FibroSure , can be used however, these have not yet been validated in patients with HIV/HBV co-infection. Another noninvasive method for calculating liver stiffness is the elastography technique known as FibroScan, which has demonstrated promising results and has been approved by the Food and Drug Administration for use in the United States.
References
Chu CJ, Keeffe EB, Han SH, et al. Hepatitis B virus genotypes in the United States: Results of a nationwide study. Gastroenterology 2003 125:444-451.
Fraquelli M, Branchi F. The role of transient elastography in patients with hepatitis B viral disease. Dig Liver Dis 2011 43:S25-S31.
Epidemiology Top Of Page
More than 350 million people are infected with HBV, with 75% of the worlds HBV carriers residing in Asia . Forty million people are infected with HIV worldwide. Due to shared modes of transmission, coinfection is common, and an estimated 4 million people worldwide are coinfected with HBV-HIV. The prevalence of HBV in HIV-infected individuals varies with the population studied. In the United States, up to 10% of all HIV-infected individuals have HBV coinfection . Several studies support an increased prevalence of HBV in HIV-infected populations of sub-Saharan Africa, with more than 80% of HIV-positive individuals in some of those countries carrying serum markers for HBV .
Figure 1.Geographic Distribution of Chronic HBV Infection.
HBsAg, hepatitis B surface antigen Source: Department of Health and Human Services Centers for Disease Control and Prevention. Viral Hepatitis Slidesets: Hepatitis B 101. Available here. Accessed January 15, 2007.
The prevalence of HBV surface antigen varies geographically, with high endemicity areas in Southeast Asia, sub-Saharan Africa, the Amazon Basin, parts of the Middle East, the central Asian republics, and parts of Eastern Europe. Areas of low endemicity include North America, Western and Northern Europe, Australia, and parts of South America .
Read Also: How Do You Get Hepatitis A And B
Occult Infection Top Of Page
Occult HBV infection is defined as the presence of HBV DNA in the absence of HBsAg . Often the only serum marker in occult HBV is anti-HBc . The prevalence of occult HBV in HIV-infected populations varies from 10% to 43% depending on the study , whereas the presence of anti-HBc alone is rarely associated with occult infection in HIV-uninfected patients. One study showed ongoing necroinflammatory liver disease with chronic ALT elevations in HIV-infected patients with occult HBV, illustrating that occult HBV represents chronic HBV with active viral replication and should be managed as such .
Immune Reconstitution Inflammatory Syndrome
Though current guidelines suggest treatment of HBV/HIV coinfected patients with dual antiviral regimen targeting HBV and HIV, immune reconstruction-related hepatic flare following the ART should be noted . IRIS is considered as a complication induced by the initiation of highly active antiretroviral therapy in HBV/HIV coinfected patients. It is an inflammatory disorder related to the worsening status of existing infection .
You May Like: Hepatitis C Treatment Guidelines 2017
Natural History Of Cryptococcus Infection
Like TB, cryptococcosis may be an acute infection but it is most often due to reactivation of latent infection. Reactivation most commonly occurs in the CNS presenting as either meningoencephalitis or cerebral cryptococcoma . Factors leading to reactivation â be it a distinct qualitative or quantitative change in immunity – are uncertain , but immunosuppression and particularly HIV infection is a major risk factor for reactivation and disease.
Immune Response To Cryptococcus And Pathogenesis
Host defense against cryptococcosis has largely been thought to be mediated by cell-mediated immunity , based on the preponderance of cryptococcosis in HIV/AIDS patients with impaired T-cell immunity, granuloma formation as characteristic of CMI, and studies of adoptive T-cell transfer in CMI-deficient Cryptococcus-susceptible animal models . Evidence also suggests a role for innate immunity and antibody-mediated humoral immunity. Protective CMI is based primarily on cryptococcal specific Th1-type CD4+ T cells, which produce IL-12, IL-2, IFN-γ, and TNF-α .
IFN-γ has been shown to play a critical role in the control of cryptococcosis in murine models and in human cryptococcosis. An increase in early IFN-γ secretion from lung-associated lymph nodes was observed in Cryptococcus-resistant mice compared to Cryptococcus-sensitive mice, and the administration of both an anti-IFN-γ and anti-IL-12 antibody resulted in reduced Cryptococcus clearance . In patients with CM, higher IFN-γ levels in CSF were associated with improved rates of CSF Cryptococcus clearance and overall survival . In HIV-CM co-infected patients, a higher proportion of IFN-γ+ CD4+ T cells was associated with a lower fungal burden and improved survival at two weeks after cART .
Read Also: How Is Hepatitis E Transmitted
The Impact Of Hiv On Malaria
Malaria parasitemia and disease
A meta-analysis of early studies largely comprising children or non-pregnant adults suggested that there was no effect of HIV infection on malaria . Several other studies also suggested that there was no association between HIV infection and malaria parasitemia in pregnant women . However, in two population based cohort studies in rural Uganda and Malawi , HIV infection was associated with an increased prevalence of clinical malaria episodes and the degree of parasitemia showed an inverse correlation with CD4+ T-cell counts in HIV-infected individuals. Although there was a relationship between malaria parasitemia and clinical disease and HIV infection, the association was not as strong as with other infections such as tuberculosis .
Humoral immunity and pregnancy-associated malaria
The decrease in opsonic activity in HIV-infected women was clinically significant, since lower levels of these antibodies were associated with anemia in these women and correlated with infant birth weight in other studies . Our data suggested that HIV infection blocks some antibody responses to malaria infection but not all, which is consistent with data showing that antibodies specific for VSAPAM and the merozoite antigen AMA-1 are decreased in HIV positive women but not antibodies specific for another merozoite surface antigen MSP-2 .
HIV-infected monocyte/macrophages and malaria