Hepatic Steatosis Hepatitis B And Virologic Response To Treatment
The data on implication of hepatic steatosis on antiviral therapy for chronic hepatitis B has been conflicting.
Cindoruk et al. retrospectively analysed 142 Turkish patients who underwent pegylated interferon alfa-2a found no difference in sustained virologic response between individuals with or without hepatic steatosis. Ateet al. also found no statistically significant difference in virologic response for patients receiving Interferon. Although, it should be pointed out that their study observed a higher sustained virologic response in the non Hepatic Steatosis group. Another more recent study performed in Turkey by Ceylan et al. , they found that although serum HBV DNA levels were found to be lower in patients with hepatic steatosis, the presence of hepatic steatosis has no effect on virologic response to either tenofovir or entecavir at 6 or 12 months. Interestingly, they also found that the presence of steatohepatitis may predict a favourable response in the tenofovir arm at 6 months. But given that their study was not designed to investigate patients with steatohepatitis and that they had a limited number of patients with steatohepatitis, it is difficult to draw a convincing association from it.
The conclusion we could gather from the presence of the current data suggests that there is unlikely any significant difference in efficacy between oral medications or interferon in patients with Hepatic Steatosis.
Non Alcoholic Fatty Liver Disease
NAFLD is usually seen in people who are overweight or obese.
According to the WHO , obesity is defined as an excess of weight by increasing the fat mass of an individual.1
However, it has been found in people of a normal weight whose diets are very high in fat and/or sugar content. A healthy liver should contain little or no fat and for most people, carrying a small amount of fat in the liver causes no major problems. Having high levels of fat in your liver is also associated with an increased risk of problems such as diabetes, heart attacks and strokes.2
If fat has been in the liver for a prolonged amount of time, the liver cells can become inflamed and the term NASH is then used. NASH may progress, like many liver diseases, to cirrhosis and liver cancer. See the diagram below:
Do not hesitate to read our article about FATTY LIVER DISEASE
References:
Treatment For Fatty Liver Disease
There are no medications approved for NAFLD, though some are in clinical trials.
Usually the first line of treatment is to lose weight. It helps reduce fat, inflammation, and scarring in your liver. Losing just 3% to 5% of your body weight can cut down on how much fat is in your liver. Weight loss surgery is also an option if you have a lot to lose.
Youâll also need to quit drinking. Itâs the only way you can keep liver damage from getting worse. You may even be able to undo some of the liver damage thatâs already happened. Talk to your doctor about how you can get help. You may need a medically supervised detox program to safely quit drinking and manage withdrawal symptoms.
If you have complications due to NASH, such as cirrhosis or liver failure, you may need to have a liver transplant. In general, people with NASH who get a liver transplant do very well.
Don’t Miss: Natural Ways To Cure Hepatitis C
Nonalcoholic Fatty Liver Disease
There are two different types of nonalcoholic fatty liver disease:
Simple fatty liver: This means you have fat in your liver, but you may not have any inflammation in your liver or damage to your liver cells. It usually doesnât get worse or cause problems with your liver. Most people with NAFLD have simple fatty liver.
Nonalcoholic steatohepatitis : This is much more serious than a simple fatty liver. NASH means you have inflammation in your liver. The inflammation and liver cell damage that happen with NASH can cause serious problems such as fibrosis and cirrhosis, which are types of liver scarring, and liver cancer. About 20% of people with NAFLD have NASH.
The Typical Treatments Hepatic Steatosis Versus Hepatocellular Disease
The primary treatment for fatty liver disease is surgery. This involves removing or dissolving the fatty liver cell. Surgery can be used for treating both severe and moderate cases. But the downside to surgery is that it can leave you with scarring that could impede your progress in losing weight and even your ability to stand up.
A more common way to diagnose fatty liver disease is through the use of liver function tests called a CT scan and an MRI. These tests will show whether or not your liver is functioning to its fullest capacity. If it shows signs of inflammation then your doctor may want to prescribe medication that will reduce inflammation. If there is fluid buildup in your abdomen, then your doctor may use a procedure called a liposuction to remove some of the fluid and reduce the swelling in the abdominal area.
===> How To Cure A Fatty Liver In Just Days < < <
The diagnosis of fatty liver is a little more tricky. A biopsy of your liver from the abdominal area will reveal inflammation, but it might not be fatty liver. It could be something else like hepatitis B or C, or even HIV if it is contained in its early stages. If the biopsy indicates the presence of fatty liver, then your doctor will conduct a trial of anti viral medication to make sure that the hepatitis does not develop into cirrhosis of the liver which would be very serious.
You May Like: Acute Hepatic Porphyria Treatment Guidelines
Fibrosis Progression In Nash
Progression of fibrosis in NASH has been histologically demonstrated in 32%-37% of the patients. Estimated rates of cirrhosis development over 10 years of 5%-20% have been reported by 3 independent studies . NASH patients with advanced fibrosis are at risk of developing liver complications. Obesity, diabetes, IR and the initial severity of the fibrosis are the factors most conspicuously associated with fibrotic progression.
The mechanisms by which IR promotes fibrosis progression include: steatosis, hyperleptinemia, increased TNF production, impaired expression of PPAR- receptors. Hepatic injury in NASH induces oxidative stress, ROS and peroxidation products which lead to cytotoxic events, release of proinflammatory cytokines that activate hepatic stellate cells and deposition of collagen.
HCC has been detected in several NASH patients, most often at the time of diagnosis, and rarely, during follow up. In the larger Olmsted County Community Study, 2 of 420 NAFLD patients developed HCC during a 7-year follow-up period. The estimated rate of liver-related deaths over 10 years was 12% for NASH patients.
Hepatitis B Status And Hepatic Steatosis
Although the pathogenesis of hepatic steatosis caused by Hepatitis B infection can be explained on the molecular level, the association between Hepatitis B virus and hepatic steatosis is poor and remains controversial. The meta-analysis performed by Machado et al. on 21 studies comprising of 4100 HBV infected patients showed no positive associations of HBV infection and hepatic steatosis. Moreover, seven studies from the meta analysis found strong negative effect of viral load on hepatic steatosis. In a more recent study by Enomoto et al. , they found a low frequency histological hepatic steatosis in patients with a high HBV-DNA level and concluded that there is unlikely an association between HBV infection and hepatic steatosis. In another large scale study in Taiwan by Cheng et al. which recruited a total of 33,439 subjects, they showed an inverse relationship between prevalence of fatty liver and positive HBsAg status in subjects older than 50 years and no significant association between HBV infection and fatty liver in subjects younger than 50 years. Although fatty liver was diagnosed via ultrasound and no liver biopsy was performed, the overwhelming statistics on these recent study showed that association between HBV infection and hepatic steatosis is not as strong as what previously thought.
Also Check: How Is Hepatitis C Virus Transmitted
What Is Nonalcoholic Fatty Liver Disease
NAFLD is a type of fatty liver disease that is not related to heavy alcohol use. There are two kinds:
- Simple fatty liver, in which you have fat in your liver but little or no inflammation or liver cell damage. Simple fatty liver typically does not get bad enough to cause liver damage or complications.
- Nonalcoholic steatohepatitis , in which you have inflammation and liver cell damage, as well as fat in your liver. Inflammation and liver cell damage can cause fibrosis, or scarring, of the liver. NASH may lead to cirrhosis or liver cancer.
Acute Fatty Liver Of Pregnancy
Acute fatty liver of pregnancy is when excess fat builds up in the liver during pregnancy. Its a rare but serious pregnancy complication. The exact cause is unknown, although genetics may be a reason.
When AFLP develops, it usually appears in the third trimester of pregnancy. If left untreated, it poses serious health risks to the mother and baby.
If your doctor diagnoses AFLP, they will want to deliver your baby as soon as possible. You might need to receive follow-up care for several days after you give birth.
Your liver health will likely return to normal within a few weeks of giving birth.
Also Check: Hepatitis C Drugs In India
Nonalcoholic Fatty Liver Disease: Diagnosis And Management
THAD WILKINS, MD, Georgia Regents University, Augusta, Georgia
ALTAF TADKOD, MD, Barrow Regional Medical Center, Winder, Georgia
IRYNA HEPBURN, MD, Good Samaritan Digestive Health Specialists, Lebanon, Pennsylvania
ROBERT R. SCHADE, MD, University of Pittsburgh Medical Center Presbyterian, Pittsburgh, Pennsylvania
Am Fam Physician. 2013 Jul 1 88:35-42.
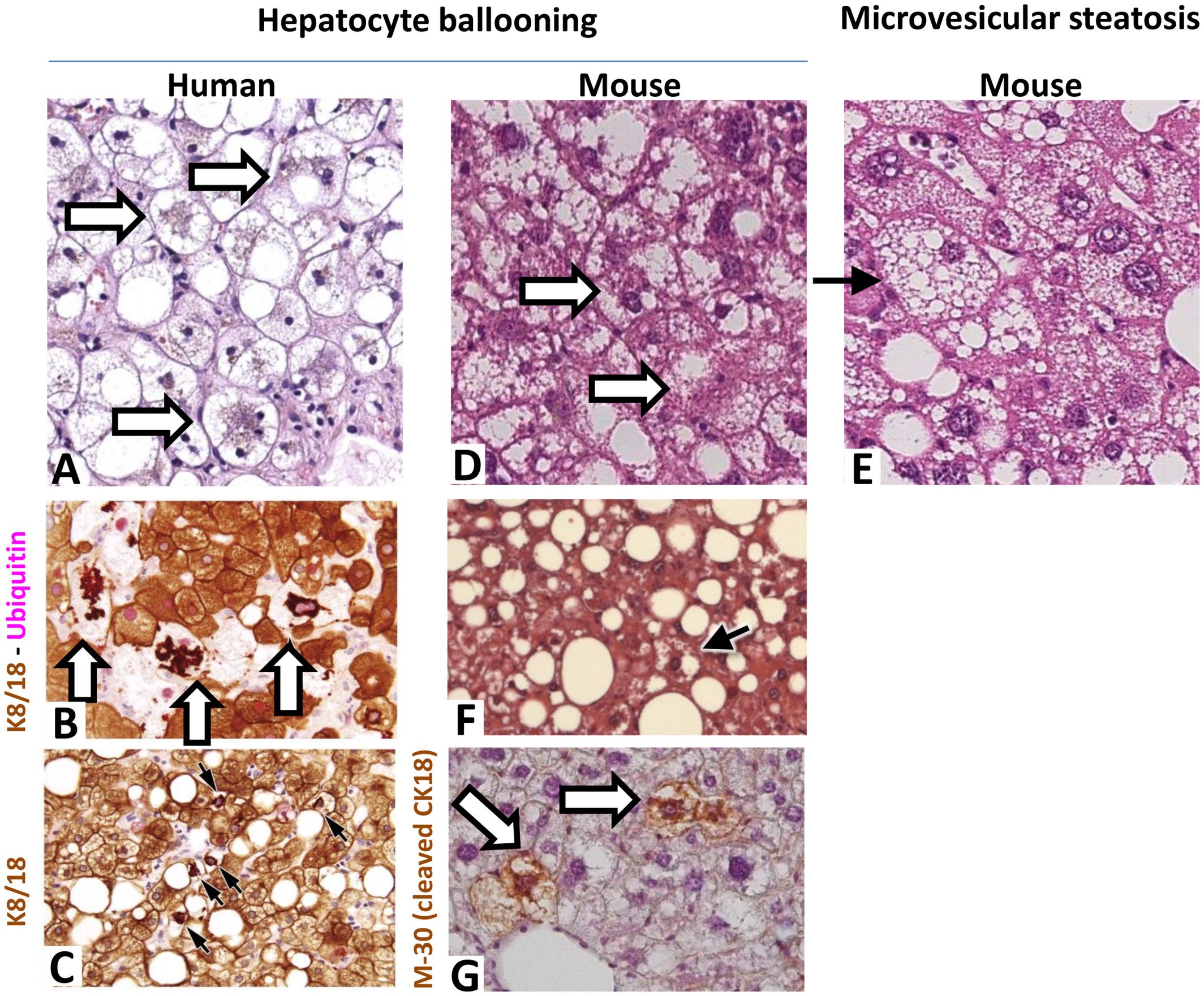
Nonalcoholic fatty liver disease is a fatty infiltration of the liver in the absence of other causes of steatosis, such as alcohol consumption. It is characterized by excessive fat accumulation in the liver . Nonalcoholic steatohepatitis is a subgroup of nonalcoholic fatty liver disease characterized by steatosis with additional findings of liver cell injury and inflammation. Hepatic steatosis and steatohepatitis can be distinguished only by liver biopsy and histology . It is unclear whether nonalcoholic fatty liver disease is a surrogate marker for disease, such as metabolic syndrome.
Ultrasonography Ct Scanning And Mri
Noninvasive studies such as ultrasonography , computed tomography scanning, and magnetic resonance imaging are useful in helping to establish a diagnosis of steatosis, as well as in finding evidence for portal hypertension these imaging tests are also helpful in ruling out biliary dilation in patients with a cholestatic pattern of liver test result abnormalities.
However, these imaging modalities can neither define the cause of steatosis nor reliably distinguish between benign steatosis and steatohepatitis. Benign steatosis may be focal or diffuse, whereas steatohepatitis is usually diffuse.
In patients with alcoholic steatosis, the liver appears diffusely echogenic on US. In patients with nonalcoholic fatty liver disease , the liver is hyperechogenic or bright. Steatosis is detected only when substantial fatty change is present. Studies in patients who are about to undergo gastric bypass surgery indicate that US has a 93% predictive value for NAFLD, with an accuracy of 76%. Patients with steatosis on US have a higher incidence of coronary artery disease and should undergo cardiac evaluation if suspicious symptoms are present.
The mean CT count is lower in the liver than in the spleen. CT scans may be used to monitor the course of the disease on successive scans. Focal fatty lesions may be identified by dual-energy CT scans that demonstrate increased attenuation with increasing energy.
Don’t Miss: Can You Get Rid Hepatitis C
Complications Of Fatty Liver Disease
The main complication for all these conditions is cirrhosis, or scarring of your liver. As your liver tries to stop the inflammation that comes with these conditions, it creates areas of scars. As inflammation spreads, so do the scars, and eventually, your liver canât do its job. That can result in:
- Fluid buildup in your abdomen
- Swollen veins in your esophagus that can burst and bleed
- Confusion and drowsiness
Viral Factors And Genotypes
It is well known that the presence of steatosis in the liver of CHC patients seems to be related to the presence of virus itself, with a distinctive genotype specificity. Six different HCV genotypes were identified according to Simmonds et al, characterized by different epidemiological and clinical peculiarities. In particular, the genotypes 1 and 3, the most prevalent in the western world, were found related to steatosis. HCV virus has, in fact, demonstrated a direct steatogenic effect in cell cultures and transgenic mice. This seems to be confirmed in human studies: there is considerable evidence that in HCV-infected subjects , the grade of hepatic steatosis seems to be related to viral load. Moreover, there has been evaluation of steatosis disappearing in response to antiviral therapy and its recurrence in the case of relapse with virus reappearance in the liver. However, non-3 genotypes also show a distinct association with steatosis, which has encouraged some authors to coin a new definition: virus-associated steatohepatitis .
You May Like: Hiv And Hepatitis B And C Are Incurable Bloodborne Pathogens
Types Of Fatty Liver Disease
Health care providers divide fatty liver disease into two types. If you just have fat but no damage to your liver, the disease is called nonalcoholic fatty liver disease . If you have fat in your liver plus signs of inflammation and liver cell damage, the disease is called nonalcoholic steatohepatitis .
About 10% to 20% of Americans have NAFLD. About 2% to 5% have NASH.
Stay Away From Refined Grains And Added Sugar
Refined grain and added sugar are significant contributory components to fatty liver disease and metabolic syndrome. Refined grain and added sugar are quickly broken down into glucose molecules in the digestive system. These glucose molecules then enter the bloodstream and spike blood sugar. Insulin is released and signals to body tissues to utilize the glucose as energy, but inevitably, there is leftover glucose that must be stored throughout the body, including the liver. Eating too many refined carbs and added sugar could, over time, contribute to fatty liver disease as well as metabolic conditions like insulin resistance and type 2 diabetes.
Steer clear of products that contain added sugar, such as candy, soda, pastries, cookies, cakes, and ice cream. Even products like granola bars, breakfast cereals, salad dressing, and condiments can contain more added sugars than you think.
To avoid refined grains, stay away from foods like white rice, white pasta, and white bread. Just like added sugar, refined grains are broken down into glucose.
Also Check: How Long Does Hepatitis B Vaccine Last
What Is Alcoholic Fatty Liver Disease
Alcoholic fatty liver disease is due to heavy alcohol use. Your liver breaks down most of the alcohol you drink, so it can be removed from your body. But the process of breaking it down can generate harmful substances. These substances can damage liver cells, promote inflammation, and weaken your body’s natural defenses. The more alcohol that you drink, the more you damage your liver. Alcoholic fatty liver disease is the earliest stage of alcohol-related liver disease. The next stages are alcoholic hepatitis and cirrhosis.
Biological Role Of Insulin
Insulin, after binding its receptor, induces the phosphorylation of receptor substrates in the liver and muscles, and triggers several steps toward the transactivation of glucose transporter-4 .This increases glucose uptake by cells and its storage as glycogen, and inhibits the net production of glucose by the liver, thus blocking glycogenolysis and neoglycogenesis. Moreover, insulin promotes lipid storage by inhibiting lipolysis. When insulin is unable to induce glucose uptake, pancreatic -cells increase insulin production and the hyperinsulinemic state prevents hyperglycemia. Thus, IR depends on insulin secretion and insulin sensitivity.
Recommended Reading: What Is Non Reactive Hepatitis C
What Does It Mean To Have Diffuse Hepatic Steatosis
If you have been told that you have diffuse hepatic steatosis, this indicates that you have fatty infiltration of the liver. The term diffuse describes the distribution pattern of fat within the liver. When fat particles are widely dispersed throughout the liver, this finding is called diffuse hepatic steatosis. Diffuse hepatic steatosis differs from focal fatty deposits, which occur in localized areas within the liver. Hepatic steatosis is the medical term that describes the accumulation of fat or lipids within liver cells, or hepatocytes.
Commonly, diffuse hepatic steatosis is indicative of fatty liver disease. Fatty liver disease means that you have excess fatty acids in your liver. Medically, your liver must be at least 5% fat to meet the criteria for a diagnosis of fatty liver disease. Fatty liver disease can be classified as either nonalcoholic or alcoholic.
Nonalcoholic fatty liver disease also called hepatic steatosis or hepatosteatosis- most often occurs due to diet and lifestyle factors, while alcoholic fatty liver disease is fueled primarily by alcohol intake. Nonalcoholic fatty liver disease is associated with conditions like metabolic syndrome, obesity, and hypertension. Genetic factors most likely contribute to the development of both nonalcoholic and alcoholic fatty liver disease as well. Fatty liver disease has a very high prevalence rate across the general population in the United States.
What You Need To Know About Fatty Liver Disease
If a fatty liver disease diagnosis is made, your doctor will perform a series of tests to identify the cause of the condition. These may include a CT scan, blood test, liver enzymes test, albumin level, serum creatinine, and urine test. Blood tests may also reveal symptoms such as high calcium, low albumin, or polydipsia. Once these symptoms are present, your doctor will evaluate them to determine if you do have fatty liver disease and what course of treatment is appropriate.
Some factors that are known to cause fatty liver disease include being overweight or obese, being a woman, and being over 50 years of age. People who smoke cigarettes or use other tobacco products are at increased risk of developing this condition. There are also other risk factors that are not well understood but include genetic tendencies toward obesity and polydipsia. Other risk factors that are associated with this disease include being older than 50 years of age and having an unhealthy body mass index. Obese people are at greater risk than thinner people for developing fatty liver disease because obese people have excess fat deposits around their bellies, hips, and thighs.
About one of every five Americans has a fatty liver, which is also called steatosis. In fact, up to 9 of every 10 diabetics and people with obesity have fatty liver.
Here are the details of each of these disorders:
Also Check: What Is Hepatic Cirrhosis Of The Liver