Pathophysiology Of Neurovisceral Pain In Acute Porphyria
The metabolic changes underlying acute porphyria have been well-delineated for more than 40 years, yet for most of that time their role in the pathogenesis of neurovisceral attacks has been unclear. Research has focused on two hypotheses that are not mutually exclusive. The first is heme deficiency, which could directly affect neuronal function in that these cells, like hepatocytes, require heme for synthesis of essential heme proteins. One such protein is tryptophan pyrrolase, which has a relatively low affinity for heme but requires it for enzymatic activity. When heme is scarce, the activity drops, potentially shifting tryptophan metabolism from the kynurenine pathway to 5-hydroxytryptamine , a neurotransmitter. Although certain aspects of acute porphyria suggest a serotonergic state, human data to confirm this postulate are lacking.
Biochemical Diagnosis Of Acute Porphyria
In all three autosomal dominant acute porphyrias, attacks are accompanied by a clear increase in PBG , which, for convenience, is generally assessed in urine rather than blood. In active AIP, the type most commonly associated with acute attacks, the PBG is at least 10-fold the upper limit of normal, more typically 20- to 100-fold. A urine PBG of > 50 mg/g creatinine in a patient with pain symptoms of unknown cause is highly specific for the diagnosis occasional genetic carriers have PBG levels in this range even when feeling well and thus represent false-positive cases. While this is unusual, it highlights the importance of having baseline information from urine samples that are collected when the patient is feeling well. ALA should be evaluated at the same time to identify cases of lead poisoning, which can mimic acute porphyria. It would also identify the rare individual with ALA dehydratase deficiency.
Treatment Of Acute Attacks
Consensus guidelines for the treatment of the acute attacks of the acute hepatic porphyrias are available. Briefly, during acute attacks, narcotic analgesics are usually required for abdominal pain, and phenothiazines are effective for nausea, vomiting, anxiety, and restlessness. Insomnia and restlessness are treated with chloral hydrate or low doses of certain short-acting benzodiazepines. Carbohydrate loading, usually with intravenous glucose , may be effective in milder acute attacks . Because intravenous hemin is more effective and the response slower if treatment is delayed, it is recommended that hemin therapy be started initially for moderate to severe attacks, and for mild attacks that do not respond to carbohydrate loading within 1-2 days. The standard regimen is 3-4 mg of heme in the form of lyophilized hematin , heme albumin , or heme arginate , infused daily for 4 days. That increased carbohydrates may ameliorate attacks is supported by the recent finding that hepatic ALAS1 is modulated by the peroxisome proliferator-activated receptor- coactivator 1, providing an important link between nutritional status and the acute attacks.
Recommended Reading: How Do They Test For Hepatitis
Treatment Of Recurrent Attacks:
In recurrent attacks that appear linked to the menstrual cycle, ovulatory suppression with gonadotropin-releasing hormone agonists may be helpful . GnRH agonists are peptides that have no demonstrable porphyria-inducing activity . The main adverse effect is menopausal symptoms, which are not tolerated by some patients. Supplemental low-dose estrogen may be helpful for those whose porphyria symptoms are improving on treatment.
Patients who experience more than 34 attacks per year should consider prophylactic hematin therapy . Monitoring of ALA and PBG between attacks is helpful for optimizing the timing of prophylactic hematin therapy. Regular, long-term administration of hematin typically requires the placement of an indwelling venous catheter for access. Patients should be monitored for complications related to chronic hematin administration such as iron overload.
Outcome Measures And Safety Assessments
Efficacy assessments including AAR of composite porphyria attacks , annualized days of hemin use, and urinary levels of ALA and PBG were collected throughout the study. Patient-reported outcomes included daily worst pain, fatigue, and nausea ,, opioid use, changes from baseline in the 12-Item Short Form Health Survey Version 2 scores, EuroQOL-5 Dimension , Patient Global Impression of Change , and Porphyria Patient Experience Questionnaire . Data for daily worst pain, fatigue, nausea, opioid use, and PGIC were collected through Month 12. Safety assessments included monitoring of AEs, clinical laboratory measures, vital signs, 12-lead electrocardiography, and physical examination and were done throughout the study. Adverse events were coded according to the Medical Dictionary for Regulatory Activities Version 23.0.
Don’t Miss: My Husband Has Hepatitis A Can I Get It
Genetic Basis Of Acute Hepatic Porphyria
Acute hepatic porphyria represents a classical group of inherited metabolic disease with incomplete penetrance and large intrafamilial expressivity . Phenotypic expression results in AHP from a complex interaction between an individual monogenic basis and epigenetic and environmental factors , as previously discussed. A summary of the main pathogenic and likely pathogenic variants reported to date in the four genes associated with AHP is provided . Most pathogenic variants related to AHP are classified as missense, small deletions, and small insertions or duplications . AIP, VP, and most cases of HCP are associated with autosomal dominant pattern of inheritance and occurs due to heterozygous pathogenic variants, respectively, in HMBS, PPOX, and CPOX genes. Biallelic variants have been also described rarely in HCP and its extremely rare variant presentation called harderoporphyria. Homozygous and compound heterozygous variants in ALAD gene are also identified in the rare context of autosomal recessive Doss porphyria . Compound heterozygous variants have also been identified in rare presentations of childhood-onset autosomal recessive AIP .
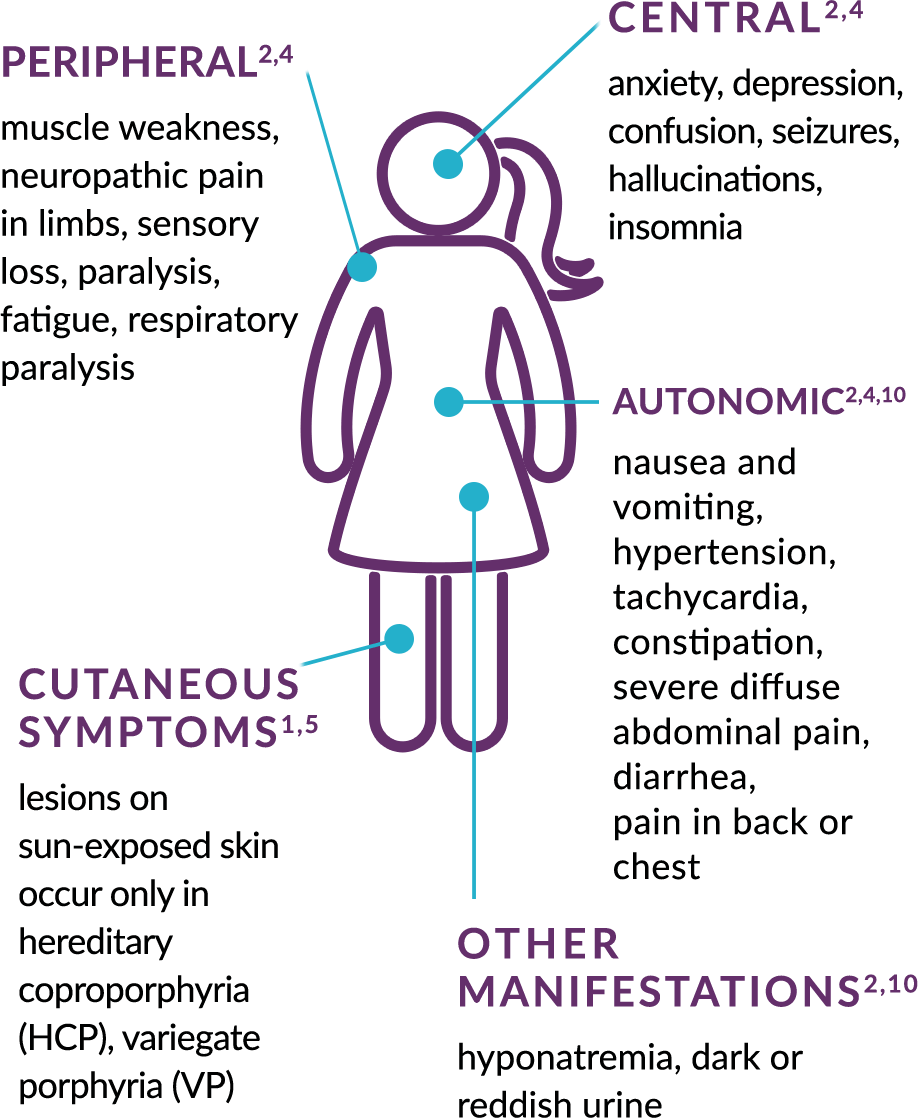
Clinical Overview Of Acute Hepatic Porphyrias
Nowadays, the AHP are considered a chronic condition with a negative impact on physical and emotional health, leading to low quality of life and complicated by acute attacks, which typically present with multiple dysfunctions of autonomic, peripheral, and central nervous system, requiring hospitalization and not rarely with fatal outcomes . In addition, long-term complications including liver disease , systemic arterial hypertension, and chronic kidney disease are part of the natural history of AHP .
Typically, most patients with AHP are women between second and fifth decades of life with recurrent episodes of severe abdominal pain accompanied by malaise, fatigue, psychiatric disturbances , nausea and vomiting, loss of appetite and constipation, and tachycardia . Even subtle neurological symptoms lasting hours to days often require visits to emergency department and opioid prescriptions to pain relief . The dark-colored urine, the clinical feature that derives the term porphyrus, may be unremarkable because ALA and PBG are colorless and is most observed after exposure of the voided urine to light, leading to the oxidative reaction of porphobilinogen to uroporphyrin and porphobilin .
You May Like: Medication For Hepatitis C Cure
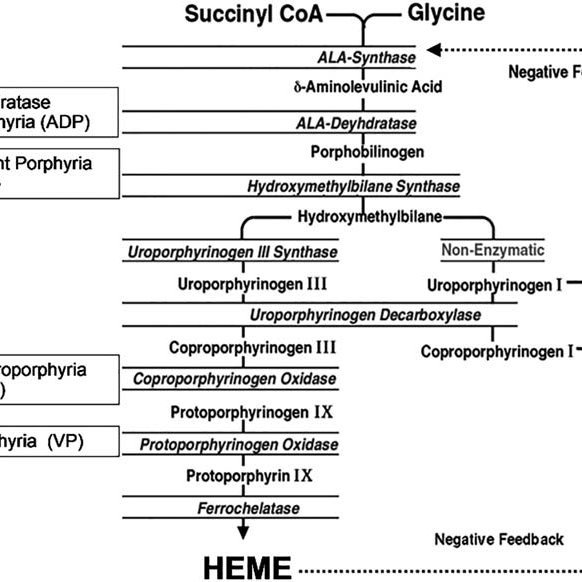
Heme Biosynthesis And Regulation
Heme is required for a variety of hemoproteins, including hemoglobin, myoglobin, respiratory cytochromes, and the cytochrome P450 enzymes. Hemoglobin synthesis in erythroid precursor cells accounts for 85% of daily heme synthesis in humans. Hepatocytes account for most of the rest, primarily for synthesis of cytochrome P450 enzymes, which are especially abundant in the liver endoplasmic reticulum, and turn over more rapidly than many other hemoproteins, such as the mitochondrial respiratory cytochromes.
Treatment Of The Acute Attack
CONTENTS
TREATMENT OF THE ACUTE ATTACK
The diagnosis of an acute attack of porphyria should be confirmed with a quantitative urine porphobilinogen concentration before starting specific treatment . This is essential in patients without a previous diagnosis of acute porphyria. For patients who have had an unequivocally diagnosed porphyria attack in the past, it may be necessary to start specific treatment before the results of the laboratory investigation are available. Withdraw any drugs which are not safe in porphyria. Treat any infection.
Read Also: Can You Get Hepatitis C Through Saliva
Pathogenesis Of The Acute Attacks
For years, the pathogenesis of these attacks was intensely debated., Did they result from: elevated levels of ALA and PBG, one or both being neurotoxic, heme deficiency in the nervous system, or both? Clearly, induction of the acute attacks is related to environmental or hormonal factors, such as drugs, diet, and steroid hormones that induce ALAS1 resulting in the overproduction of ALA and PBG.
Recently, new insight into the etiology of the acute attacks came from several patients with AIP and VP who had chronic attacks that ceased after liver transplantation., Of note, domino transplantation of the porphyric livers into recipients with liver failure who did not qualify for transplantations, corrected their liver function, but made them susceptible to acute attacks. Thus, the debate was resolved. The acute attacks result from the hepatic production of a neurotoxic substance, presumably ALA and/or PBG that may interact with -aminobutyric acid or glutamate receptors.
Classification Of The Porphyrias
Traditionally, the porphyrias have been classified as either hepatic or erythropoietic depending on the primary site of overproduction and accumulation of porphyrin precursors or porphyrins, although some porphyrias have overlapping features., The hepatic porphyrias are characterized by overproduction and initial accumulation of the porphyrin precursors, ALA and PBG, and/or porphyrins primarily in the liver, whereas in the erythropoietic porphyrias, overproduction and initial accumulation of the pathway intermediates occur primarily in bone marrow erythroid cells. Here, for simplicity, we have classified the 8 major porphyrias into 3 groups: the 4 acute hepatic porphyrias, the single hepatic cutaneous porphyria PCT, and the 3 erythropoietic cutaneous porphyrias . It should be appreciated that there is some overlap, as patients with the acute hepatic porphyrias, hereditary coproporphyria , and variegate porphyria may have cutaneous lesions, and the rare homozygous dominant forms of acute intermittent porphyria , HCP, and VP, as well as the rare homozygous recessive form of PCT, hepatoerythropoietic porphyria, have erythropoietic manifestations.
Also Check: Long Term Effects Of Hepatitis C
Heme Precursor Patterns In Acute Porphyria And Genetic Diagnosis
shows the profile of heme precursors in urine or feces for the four hepatic porphyrias. The pattern is distinctive for each type, reflecting the step that is genetically altered. The route of precursor excretion reflects the relative lipophilicity of the individual precursors, as noted above. Before the advent of genetic analysis, the enzymatic defect for each of the porphyrias was predicted from these patterns and confirmed by assays of enzyme activity. In AIP, the altered gene product, HMBS , exists in two forms, which arise by alternative splicing of the primary transcript the erythroid HMBS gene transcript lacks exon 2 of the hepatic transcript. Because the enzyme is cytosolic, it persists in erythrocytes. A commercial blood test was developed, which is used together with urine tests to diagnose AIP. Its main shortcoming is partial overlap of the normal and deficient ranges. Also, it yields a false-negative result when the HMBS mutation is in exon 2, which the erythroid-specific transcript lacks. Finally, sample handling problems may allow decay of the activity and a false-positive result. Overall, the HMBS assay identifies about 80% of AIP carriers. Enzyme tests for HCP and VP , respectively, are not available commercially. An assay for CPOX in whole blood was offered in the 1990s but resulted in many false-positive results and ultimately was discontinued.
Missed Diagnosis And Misdiagnosis
In the urgent care setting, porphyria is often overlooked as a diagnostic possibility, because the symptoms are those of far more common conditions. When the initial screening tests for the common conditions are negative, patients usually are discharged with a diagnosis of viral gastroenteritis, irritable bowel syndrome, addiction withdrawal, or psychosomatic pain. A recent study of U.S. patients with genetically confirmed acute porphyria found that the diagnosis was delayed by an average of 15 years from the onset of symptoms . The case presented above is unusual, in that a perceptive resident physician thought of the diagnosis and ordered the correct test, a urine PBG.
The number of people who have been misdiagnosed and believe, erroneously, that they have acute porphyria far exceeds those with a confirmed diagnosis. When they come to an ED, very few will have documentation of their diagnosis. In this situation, a rapid PBG would be definitive but, as discussed above, is not available. Although neurological complications are not a concern in this group, a test that excludes acute porphyria would redirect attention to other possible causes of the patient’s complaints and potentially avoid an expensive and unproductive hospitalization.
Also Check: How Can A Person Get Hepatitis B
Pathophysiology Of Acute Hepatic Porphyrias
Porphyrin precursors, in particular ALA, are likely neurotoxins , whereas porphyrins are light absorbing chemicals that act as photosensitizers, resulting in skin damage. In VP and HCP, both porphyrin precursors and porphyrins accumulate, and patients with these types can present with both neurovisceral attacks and cutaneous symptoms.
In AHP, the severity of the overproduction of intermediates is dependent on the demand for heme. When the need for heme production is low, ALAS1 typically remains the rate-limiting step in the pathway even with the presence of a partially defective enzyme downstream, and there is minimal accumulation of heme intermediates. Under inducing conditions that increase demand for heme synthesis, ALAS1 expression increases, and the defective enzymatic step becomes the rate-limiting step. With persistence of the demand for heme, ALAS1 expression remains elevated, resulting in abnormal accumulation of ALA and PBG. In HCP and VP, the accumulation of coproporphyrinogen III and protoporphyrinogen IX, respectively, inhibits the function of hepatic hydroxymethylbilane synthase . This is the metabolic setting for an acute attack of AHP.
While several hypotheses have been proposed regarding the pathogenesis of episodic acute attacks in AHP patients, including relative heme deficiency in nerve tissue, recent data has pointed to excess circulating ALA as the etiology.
Disclosures Of Conflicts Of Interest
In accordance with ACCME guidelines, PER® has identified and resolved all conflicts of interest for faculty, staff, and planners prior to the start of this activity by using a multistep process.
Herbert L. Bonkovsky, MD
- Grant/Research Support : Alnylam Pharmaceuticals Gilead Sciences Mitsubishi-Tanabe, NA Recordati Rare Diseases
- Consultant: Alnylam Pharmaceuticals Disc Medicine Mitsubishi-Tanabe NA Recordati
Vera Bril, MD
- No relevant financial relationships with commercial interests
Rachel Waldron, MD
- No relevant financial relationships with commercial interests
Bruce Wang, MD
- Grant/Research Support : Alnylam Pharmaceuticals
- Consultant: Alnylam Pharmaceuticals Recordati Rare Diseases
The staff of Physicians Education Resource®, LLC , have no relevant financial relationships with commercial interests to disclose.
Don’t Miss: Hepatitis A And B Symptoms
Prevalence Of Acute Hepatic Porphyria
The prevalence of AIP has been estimated at 510 cases per 100,000. However, this is based largely on people with symptoms, who represent only a small fraction of those who carry a relevant mutation and are at risk of an attack. In one study of mutation prevalence from France, 3,350 healthy blood donors were screened for HMBS deficiency. The test was positive in four, and a known AIP mutation was documented in two. Thus, the prevalence of mutations in this group was at least 1:1,675 far larger than is generally assumed. Another study from northwestern Russia and Finland screened patients who were admitted to a neurology ward with acute polyneuropathy or encephalopathy and abdominal pain. Out of 108 patients, 11% proved to have previously undiagnosed acute porphyria. While these studies are small, they suggest that people coming to an Emergency Department with recent onset abdominal pain may have a mutation for AIP more often than is generally assumed.
Deterrence And Patient Education
During an acute attack, potentially harmful medications should be discontinued whenever possible. It is strongly advised for clinicians to consult the websites of the American Porphyria Foundation and the European Porphyria Network , which list many medications, including those that are not classified with certainty provide evidence for these classifications, and are regularly updated. Also, these websites should be consulted to avoid prescribing harmful medications in treating concurrent illnesses or symptoms.
Potentially harmful lifestyle factors include smoking and alcohol use. Patients should be counseled to avoid or discontinue smoking, including the use of marijuana, and to avoid alcohol intake. Smoking and alcohol use can both exacerbate acute hepatic porphyrias via induction of hepatic cytochrome P450 enzymes , which, in turn, can diminish the pool of hepatic heme and directly induce enzymes in the porphyrin pathway, leading to increased synthesis of toxic heme precursors.
Acute attacks are also associated with sex hormones , decreased caloric or carbohydrate intake , and metabolic stress due to infections or other illnesses.
Don’t Miss: Hepatic Wet Food For Cats
Treatment Of Acute Porphyria
Initial management is focused on eliminating factors that may be contributing to an attack, including inducer medications, caloric deprivation, and dehydration . Medications considered risky for genetic carriers of acute porphyria and all nonessential medications are discontinued. The American Porphyria Foundation and the European Porphyria Network maintain lists of drugs that are considered safe or hazardous. If possible, calories and rehydration are administered orally to reverse the fasting state otherwise, 10% dextrose in 0.45% normal saline is administered IV. Although this therapy has not been tested in controlled trials, it does stop the attack for some patients. Hyponatremia may be severe, requiring urgent saline administration. A protocol that minimizes the risk of brainstem damage should be followed. Pain relief generally requires opiates, often in large doses, while waiting for porphyria-specific therapy to take effect .
The Erythropoietic Cutaneous Porphyrias
The erythropoietic cutaneous porphyrias, congenital erythropoietic porphyria and EPP, and its recently recognized X-linked form, XLP, are characterized by elevations of porphyrins in bone marrow and erythrocytes and usually present with cutaneous photosensitivity in infancy or early childhood,, or in the case of CEP, even in utero as nonimmune hydrops fetalis.
Also Check: How Can Hepatitis B Be Transmitted
Acute Hepatic Porphyria: Pathophysiological Basis Of Neuromuscular Manifestations
- Division of Neuromuscular Diseases, Department of Neurology and Neurosurgery, Federal University of São Paulo , São Paulo, Brazil
Acute hepatic porphyria represents a rare, underdiagnosed group of inherited metabolic disorders due to hereditary defects of heme group biosynthesis pathway. Most patients have their definite diagnosis after several years of complex and disabling clinical manifestations and commonly after life-threatening acute neurovisceral episodes or severe motor handicap. Many key studies in the last two decades have been performed and led to the discovery of novel possible diagnostic and prognostic biomarkers and to the development of new therapeutic purposes, including small interfering RNA-based therapy, specifically driven to inhibit selectively delta-aminolevulinic acid synthase production and decrease the recurrence number of severe acute presentation for most patients. Several distinct mechanisms have been identified to contribute to the several neuromuscular signs and symptoms. This review article aims to present the current knowledge regarding the main pathophysiological mechanisms involved with the acute and chronic presentation of acute hepatic porphyria and to highlight the relevance of such content for clinical practice and in decision making about therapeutic options.