What Are The Types Of Hepatitis B
There are two types of hepatitis B infection: acute and chronic.
Acute
An acute infection happens at the beginning, when you first get infected with hepatitis B. Many people are able to clear it from their bodies and recover. In fact, this is true of about 4 in 5 adults who are infected.
Chronic
If you are not able to clear the infection within six months or longer, you have chronic hepatitis B. It is chronic hepatitis B that leads to inflammation and the serious, and possibly fatal, illnesses of cirrhosis of the liver and liver cancer. Treatment can slow disease progress, reduce the chance of liver cancer and increase your chances of surviving.
How Long Does It Last
Hepatitis A can last from a few weeks to several months.
Hepatitis B can range from a mild illness, lasting a few weeks, to a serious, life-long condition. More than 90% of unimmunized infants who get infected develop a chronic infection, but 6%10% of older children and adults who get infected develop chronic hepatitis B.
Hepatitis C can range from a mild illness, lasting a few weeks, to a serious, life-long infection. Most people who get infected with the hepatitis C virus develop chronic hepatitis C.
Where Is The Hepatitis B Virus Found And How Is It Transmitted
Blood is the major source of the hepatitis B virus in the workplace. It can also be found in other tissues and body fluids, but in much lower concentrations. The risk of transmission varies according to the specific source. The virus can survive outside the body for at least 7 days and still be able to cause infection.
Also Check: Lactulose Dosing For Hepatic Encephalopathy
Why Are The Trial Results Significant
The trial offers the first evidence that mRNA technology may be effective against melanoma.
Modernas COVID-19 shot also uses mRNA technology, which allows for faster development of vaccines.
The company can make one of its melanoma vaccines within about eight weeks, a Moderna spokesperson said in an email.
The technology is very exciting, said Patrick Hwu, president and chief executive officer of Moffitt Cancer Center in Tampa.
Researchers can test to see if its successful against other forms of cancer, said Hwu, a tumor immunologist.
A Note About Sex And Gender
Sex and gender exist on spectrums. This article will use the terms male, female, or both to refer to sex assigned at birth. .
It is important that infants who are born to females with hepatitis B receive accurate doses of the hepatitis B vaccine. They may also be required to receive hepatitis B immunoglobulin if it is available.
The WHO also recommends using antiviral prophylaxis to help prevent hepatitis B transmission.
The table below outlines the two recommended hepatitis B vaccine schedules for infants born to those who have hepatitis B:
| Vaccine series |
|---|
You May Like: How Long Can Someone Live With Hepatitis B
What Other Problems Can Hepatitis B Cause
In rare cases, acute hepatitis B can cause liver failure.
Chronic hepatitis B can develop into a serious disease that causes long-term health problems such as cirrhosis , liver cancer, and liver failure.
If you have ever had hepatitis B, the virus may become active again, or reactivated, later in life. This could start to damage the liver and cause symptoms.
What Causes Hepatitis B
- being born to a mother with hepatitis B
- having unprotected sex with an infected person
- sharing drug needles or other drug materials with an infected person
- getting an accidental stick with a needle that was used on an infected person
- being tattooed or pierced with tools that were used on an infected person and werent properly sterilized, or cleaned in a way that destroys all viruses and other microbes
- having contact with the blood or open sores of an infected person
- using an infected persons razor, toothbrush, or nail clippers
You cant get hepatitis B from
- being coughed on or sneezed on by an infected person
- drinking unclean water or untreated water that has not been boiled
- eating food that is unclean or has not been properly cooked
- hugging an infected person
- shaking hands or holding hands with an infected person
- sharing spoons, forks, and other eating utensils
- sitting next to an infected person
Mothers who have hepatitis B can safely breastfeed their babies. If a baby receives hepatitis B immune globulin and starts receiving the hepatitis B vaccine to prevent hepatitis B infection shortly after birth, hepatitis B is unlikely to spread from mother to child through breastfeeding.15
Read Also: How Do You Find Out If You Have Hepatitis
What Does Hepatitis B Carrier Mean
Hepatitis B carrier is someone who has been exposed to HepB vaccine but does not have symptoms of the virus.
This means that the blood test for hepatitis B may show no sign of the virus, even though the person may have been exposed to it and developed symptoms. This can happen if the person had a previous exposure to hepatitis B as an infant or child, or any other reason for not being able to develop antibodies in response.
We hope this explains the Hepatitis B carrier meaning. For more information dont hesitate to take a look at what our experts say in other articles!
How Long Can You Live With Hepatitis B
Most people who contract hepatitis B during adulthood fully recover within 1 to 3 months.
People with chronic hepatitis B may have a higher risk of developing long-term liver problems, like cirrhosis or liver cancer, which require treatment and may be life threatening.
Keep in mind that the risk of developing chronic hepatitis B is higher for babies and children, especially if they have not been vaccinated against the virus.
Also Check: Cvs Hepatitis B Vaccine Appointment
Approaches By Virus Life Cycle Stage
consist of a and sometimes a few stored in a capsule made of , and sometimes covered with a layer . Viruses cannot reproduce on their own and instead propagate by subjugating a host cell to produce copies of themselves, thus producing the next generation.
Researchers working on such “” strategies for developing antivirals have tried to attack viruses at every stage of their life cycles. Some species of mushrooms have been found to contain multiple antiviral chemicals with similar synergistic effects.Compounds isolated from fruiting bodies and filtrates of various mushrooms have broad-spectrum antiviral activities, but successful production and availability of such compounds as frontline antiviral is a long way away. Viral life cycles vary in their precise details depending on the type of virus, but they all share a general pattern:
Before cell entry
This stage of viral replication can be inhibited in two ways:
Uncoating inhibitor
Inhibitors of uncoating have also been investigated.
During viral synthesis
Reverse transcription
Integrase
Transcription
Hepatitis B And Pregnancy
If youâre pregnant, you might pass the virus to your baby at birth.
If your baby gets the virus and isnât treated, they could have long-term liver problems. All newborns with infected mothers should get hepatitis B immune globulin and the vaccine for hepatitis at birth and during their first year of life.
You May Like: How To Convert Hepatitis B Positive To Negative
History Of Hepatitis B Virus
In 1965, the âAustralian Antigenâ was then discovered and identified as the Hepatitis B virus surface antigen HBsAg. This was one of the first breakthroughs in the effort to understand the pathology of viral hepatitis that instigated jaundice in those infected with HBV. It allowed industrialized countries to reliably diagnose asymptomatic carries of Hepatitis B virus and the discovery provided healthcare professionals a way to screen blood for Hep B before administering blood transfusions.
Today, Hepatitis B Virus infection is easily avoided by receiving one of the Hepatitis B vaccines. The plasma-derived HepB vaccine was licensed in 1981 and was subsequently replaced in 1986 with the recombinant HepB vaccine. Engerix B was approved in 1989 and Heplisav-B was approved in 2017. All of which provide protection against HBV.
Hepatitis B Vaccination In Pregnancy
Hepatitis B infection in pregnant women may result in severe disease for the mother and chronic infection for the baby.
This is why the hepatitis B vaccine is recommended for pregnant women who are in a high-risk category.
Theres no evidence of any risk from vaccinating pregnant or breastfeeding women against hepatitis B.
And, as its an inactivated vaccine, the risk to the unborn baby is likely to be negligible .
You May Like: Hepatitis C How Is It Spread
Recommended Reading: Where Can I Get My Hepatitis B Vaccine
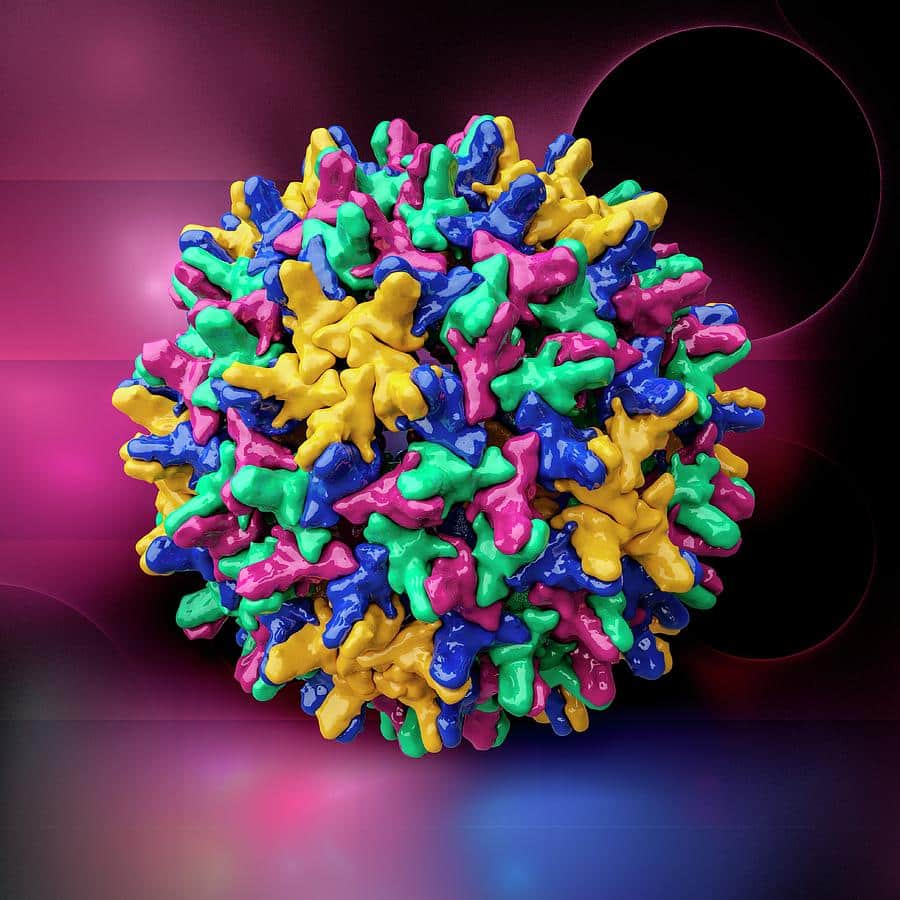
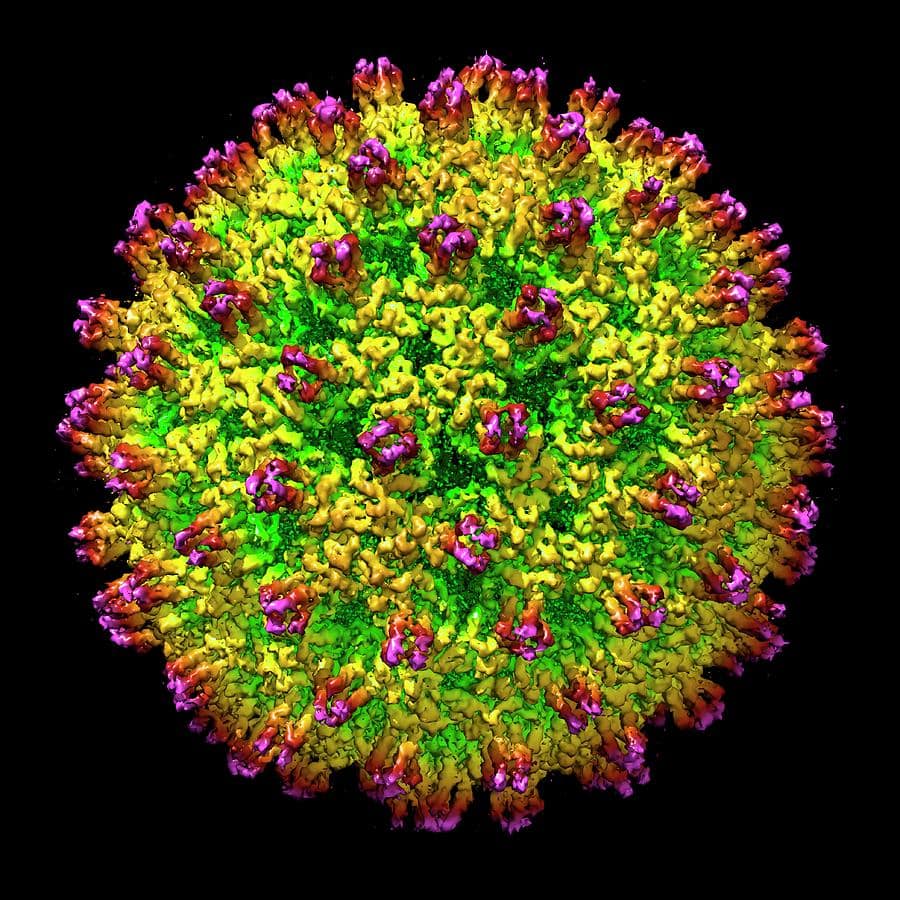
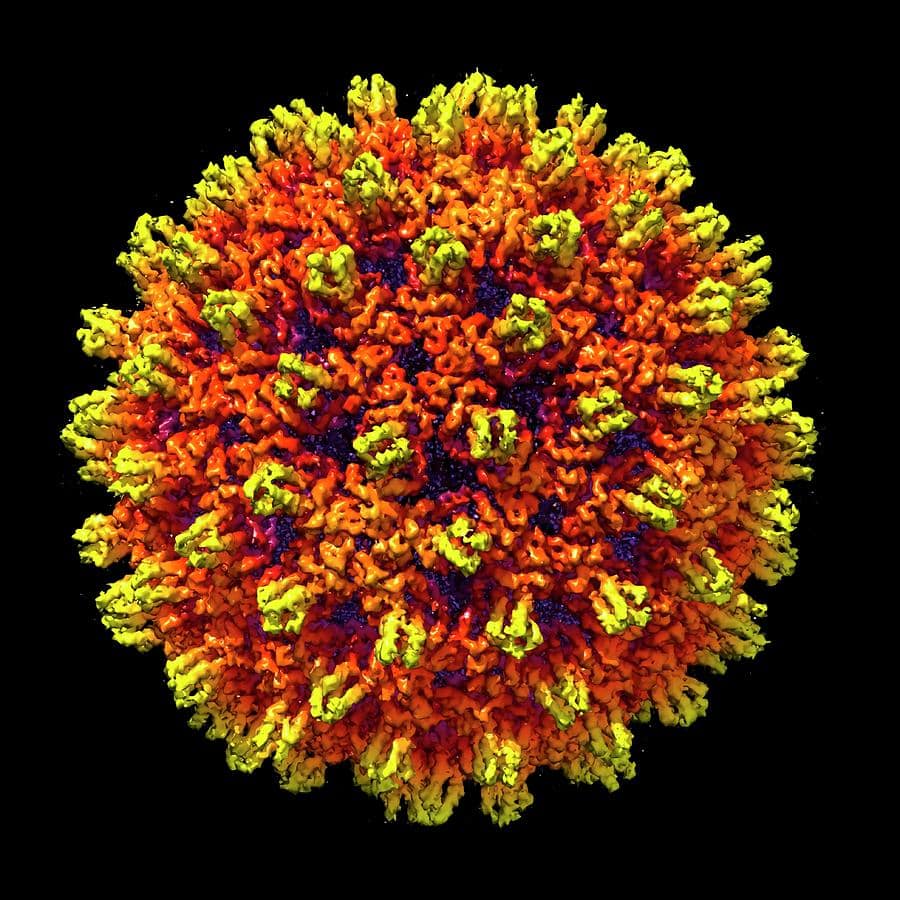
About The Hepatitis B Virus
The hepatitis B virus is a small DNA virus that belongs to the Hepadnaviridae family. Related viruses in this family are also found in woodchucks, ground squirrels, tree squirrels, Peking ducks, and herons.
Structure of the Hepatitis B Virus The hepatitis B virus contains an outer envelope and an inner core.
- The outer envelope of the virus is composed of a surface protein called the hepatitis B surface antigen or “HBsAg”. The HBsAg can be detected by a simple blood test and a positive test result indicates a person is infected with the hepatitis B virus.
- The inner core of the virus is a protein shell referred to as the hepatitis B core antigen or “HBcAg,” which contains the hepatitis B virus DNA and enzymes used in viral replication.
Life Cycle of the Hepatitis B Virus
The hepatitis B virus has a complex life cycle. The virus enters the host liver cell and is transported into the nucleus of the liver cell. Once inside the nucleus, the viral DNA is transformed into a covalently closed circular DNA , which serves as a template for viral replication . New HBV virus is packaged and leaves the liver cell, with the stable viral cccDNA remaining in the nucleus where it can integrate into the DNA of the host liver cell, as well as continue to create new hepatitis B virus. Although the life cycle is not completely understood, parts of this replicative process are error prone, which accounts for different genotypes or genetic codes of the hepatitis B virus.
Treatment Options For Antiviral Resistant Pathogens
If a virus is not fully wiped out during a regimen of antivirals, treatment creates a bottleneck in the viral population that selects for resistance, and there is a chance that a resistant strain may repopulate the host. Viral treatment mechanisms must therefore account for the selection of resistant viruses.
The most commonly used method for treating resistant viruses is combination therapy, which uses multiple antivirals in one treatment regimen. This is thought to decrease the likelihood that one mutation could cause antiviral resistance, as the antivirals in the cocktail target different stages of the viral life cycle. This is frequently used in retroviruses like HIV, but a number of studies have demonstrated its effectiveness against influenza A, as well. Viruses can also be screened for resistance to drugs before treatment is started. This minimizes exposure to unnecessary antivirals and ensures that an effective medication is being used. This may improve patient outcomes and could help detect new resistance mutations during routine scanning for known mutants. However, this has not been consistently implemented in treatment facilities at this time.
Also Check: What’s The Signs Of Hepatitis C
Hepatitis B And Your Liver
The liver is such an important organ that we can survive only one or two days if it completely shuts down – if the liver fails, your body will fail, too. Fortunately, the liver can function even when up to 80% of it is diseased or removed. This is because it has the amazing ability to regenerate – or create – itself from healthy liver cells that still exist.
If your body were an automobile, your liver would be considered the engine. It does hundreds of vital things to make sure everything runs smoothly:
- Stores vitamins, sugar and iron to help give your body energy
- Controls the production and removal of cholesterol
- Clears your blood of waste products, drugs and other poisonous substances
- Makes clotting factors to stop excessive bleeding after cuts or injuries
- Produces immune factors and removes bacteria from the bloodstream to combat infection
- Releases a substance called “bile” to help digest food and absorb important nutrients
The word hepatitis actually means inflammation of the liver. Thus, hepatitis B refers to inflammation of the liver caused by the hepatitis B virus. With early detection and appropriate follow-up medical care, people living with a chronic hepatitis B infection can expect to enjoy a long and healthy life.
Acute Hepatitis B Symptoms
There are three phases of acute hepatitis B infection, and symptoms may differ depending on the stage. Early in the disease, called the prodromal phase, symptoms may include:
- Dark urine and light stool color
During the icteric phase:
- Jaundice develops
- Anorexia, nausea and vomiting may worsen
- Irritated skin lesions may develop
- Other symptoms may subside
Read Also: What Is Chronic Hepatitis B
How Common Is It
In 2006, the Public Health Agency of Canada reported the incidence of HBV as 2.0 cases for every 100,000 or about 650 cases reported annually in Canada. In the year 2013, the incident rate was 0.5 per 100,000 . Incidence of the disease varies from region to region but has been declining due to increasing use of the vaccine and universal immunization programs.
An Ounce Of Prevention
As a liver transplant specialist, Dr. Choi notes that the most common reasons for a liver transplant in the U.S. are alcohol-related liver disease and metabolic-associated fatty liver disease also known as fatty liver.
Alcohol use and metabolic syndromeobesity plus diabetes, high cholesterol and high blood pressurehave been on the rise in our country, and we are seeing their impact in the liver world, he says, concluding that adopting a healthier lifestyle can prevent both diseases.
As well, the HBV vaccine should be offered to all infants and children, and to adults who are not immune to the virus.
Dr. Choi also points to several diseases that are not always preventable, such as autoimmune liver disease. Fortunately, he says, most of these diseases can be treated or controlled so that you wont develop cirrhosis or liver cancer. Thats why screening to diagnose liver disease early is so crucial.
While a liver transplant can save your life, not needing one in the first place is the best outcome, he adds.
Also Check: How I Cured Myself Of Hepatitis B
Enhancing Healthcare Team Outcomes
The interprofessional health care team faces many challenges when vaccinating patients for hepatitis B. While few medical interventions have as significant an impact on health as vaccinations, and the hepatitis B vaccination is generally safe, lack of knowledge about the vaccine by healthcare team members and patient concern about adverse events can decrease coverage. Challenges on knowledge of the vaccine for healthcare team members include staying current on evolving recommendations for whom the vaccine is indicated. All team members can increase the vaccination rate of their patients by encouraging all staff to become trained in the assessment of vaccination histories and any pertinent staff in the administration of the vaccine. Protecting the time available for the team to do this is an essential component of this strategy. All patients should receive education on the benefits of vaccination, including its herd immunity effect, the generally safe side effect profile, and the relatively few contraindications. A presumption of acceptance may be effective with most patients. The hesitant parent and patient who does not respond to this can pose a challenge in vaccination. Motivational interviewing techniques have shown to be effective with these hesitant patients.
What Is Involved In A Liver Transplant
A liver transplant is considered necessary when the liver is damaged and cannot function or in some cases of liver cancer. Your liver is very important. It is responsible for many functions related to making sure that your body stays healthy and is able to digest foods.
You may be eligible for a transplant if you have chronic hepatitis B infection or some of the diseases that may result from it, including liver cancer and cirrhosis. You will have to complete testing and be evaluated before being approved for a transplant. It is likely that you will be placed on a waiting list while an appropriate organ is found.
Donated livers come from two types of donors: living and deceased. Because the liver can regenerate, it is possible to use part of a liver for transplant. The remaining sections in both the donor and the receiver will grow into livers of adequate size.
People who get liver transplants must take anti-rejection drugs for the rest of their lives. These drugs make you more susceptible to infection. However, liver transplants have become more successful over time and continue to improve.
Don’t Miss: Can You Live With Hepatitis C
What Is The Outlook
Most people with hepatitis A recover without any complications. Once youve had hepatitis A, you cant get it again. Antibodies to the virus will protect you for life.
Some people may be at an increased risk for serious illness from hepatitis A. These include:
acute hepatitis B infections in the United States in 2018.
Immunosuppressive Or Anticancer Therapy
Hepatitis B virus reactivation is common in patients receiving immunosuppressive or anticancer therapy. In patients with HCC, hepatitis after systemic chemotherapy occurs in up to 60% of cases, most of which is attributed to HBV reactivation.48 In patients receiving hematopoietic stem cell transplantation, HBV reactivation also occurs in up to 50% of HBV-infected patients.49 HBV reactivation may result in liver decompensation and death. In addition, cessation of anticancer therapy is often necessary during HBV reactivation and it may interfere with successful cancer treatment.
HBV reactivation during immunosuppressive or anticancer therapy is characterized by a rise in HBV DNA, followed by ALT flares. ALT flares commonly occur after the withdrawal of immunosuppressive or anticancer therapy because of the combined effect of rising viral load and immune restitution. When icteric hepatitis occurs, the mortality rate is between 5% and 40%.48
Young patients, male sex, high pretreatment ALT, and HBV DNA are risk factors of HBV reactivation.50 Although HBeAg is associated with high HBV DNA in general, HBeAg-negative patients with precore and/or basal core promoter mutants are also at risk of reactivation.51 The risk of reactivation is also associated with the intensity of immunosuppression. Systemic corticosteroids and anthracyclines are most commonly associated with HBV reactivation.48 Recent studies also reported a high risk of HBV reactivation with the use of rituximab.
You May Like: What Are The Signs And Symptoms Of Hepatitis B