Fibrosis Progression In Nash
Progression of fibrosis in NASH has been histologically demonstrated in 32%-37% of the patients. Estimated rates of cirrhosis development over 10 years of 5%-20% have been reported by 3 independent studies . NASH patients with advanced fibrosis are at risk of developing liver complications. Obesity, diabetes, IR and the initial severity of the fibrosis are the factors most conspicuously associated with fibrotic progression.
The mechanisms by which IR promotes fibrosis progression include: steatosis, hyperleptinemia, increased TNF production, impaired expression of PPAR- receptors. Hepatic injury in NASH induces oxidative stress, ROS and peroxidation products which lead to cytotoxic events, release of proinflammatory cytokines that activate hepatic stellate cells and deposition of collagen.
HCC has been detected in several NASH patients, most often at the time of diagnosis, and rarely, during follow up. In the larger Olmsted County Community Study, 2 of 420 NAFLD patients developed HCC during a 7-year follow-up period. The estimated rate of liver-related deaths over 10 years was 12% for NASH patients.
What Is A Degenerative Disease Of The Liver Characterized By Scarring
Serosis is a chronic degenerative liver condition marked by scarring. The scars may be visible on the surface of the liver or may only be detectable under the skin, in other words, subclinical. They can’t be cured but they can be treated.
The most common cause of serous liver disease is alcohol consumption. Other causes include taking certain medications, such as phenacetin , acetaminophen , chloramphenicol , and methotrexate having autoimmune disorders such as primary biliary cirrhosis or primary sclerosing cholangitis and genetic conditions such as Hereditary Hemorrhagic Telangiectasia . HHT is a rare genetic disorder that affects the blood vessels, causing them to develop an abnormal number of holes. This disease can lead to liver cancer if not treated.
Liver disease is a major concern for people who drink alcohol regularly because alcohol affects both healthy and diseased livers in similar ways. It can cause severe damage to healthy liver tissue, leading to cirrhosis.
About Article Author
Ashley Shields
Ashley Shields has been in the health industry for over 10 years. She has worked as an intern for both hospitals and medical schools, gaining experience in every aspect of medicine and health. She loves to share her knowledge of health with others through blogging or speaking at conferences, where she can share what she’s learned during her time in the field.
Disclaimer
Fatty Liver Disease Has A Genetic Component
The likelihood of developing fatty liver disease is influenced in part by genetics. But the heritability of fatty liver is not so simple to determine. Research has shown that there is not just one gene that determines the risk of developing fatty liver disease, but rather an interaction of many genes in your DNA.
Research published in Clinical and Molecular Hepatology describes three genes PNPLA2, GCKR, and TM6SF2 that may influence the likelihood of fat accumulation in the liver. Specific variants of each gene are associated with increased risk of conditions associated with fatty liver disease, such as insulin resistance and type 2 diabetes. Of the three genes, PNPLA3 is the most well-studied gene and directly plays a role in liver metabolic processes. Moreover, a certain variant of the PNPLA3 gene is associated with a higher risk of fatty liver disease progression to NASH, fibrosis, and cirrhosis.
You May Like: Where To Get Tested For Hepatitis B
What Is The Medical Term For Liver Disease
Alcoholism and liver disease A catch-all phrase describing a variety of clinical disorders induced by prolonged excessive alcohol intake, such as hepatitis, fatty liver, and cirrhosis. Alcoholic hepatitis is a type of severe acute alcoholic intoxication that can lead to death. Alcoholic hepatitis differs fromsimple alcoholic poisoning in that it involves inflammation of the liver, usually caused by excess consumption of alcohol.
Liver disease A condition in which the ability of the liver to function properly is impaired. Liver disease can be caused by many different factors including viral infection, alcoholism, autoimmune diseases, and diabetes. The most common form of liver disease is chronic hepatitis which does not cause immediate damage to the liver but over time may lead to scarring of the liver and reduce its capacity to function. There are several types of chronic hepatitis including viral, alcoholic, autoimmune, and congenital. Other forms of liver disease include cirrhosis and cancer.
The two main types of liver cancer are hepatocellular carcinoma , which accounts for more than 90% of all cases of liver cancer, and cholangiocarciousne . HCC is generally associated with chronic liver disease due to Hepatitis B or C infection, heavy alcohol use, or cirrhosis.
What Is A Progressive Degenerative Disease Of The Liver
Cirrhosis is a chronic liver condition that worsens with time. The two main types of cirrhosis are caused by alcohol abuse or infection with the bacteria Hepatitis C or B. Other factors such as autoimmune diseases, medications, and toxins can also lead to cirrhosis.
Alcoholism is a common cause of cirrhosis in people aged 30 to 60. Alcohol causes scarring of the liver, which prevents it from working properly. With time, this repeated injury leads to more severe scarring and eventually cancer.
Hepatitis is an inflammation of the liver caused by certain viruses or bacteria. There are several types of hepatitis, but most can be divided into two categories: acute and chronic. Acute hepatitis usually goes away on its own after causing the body to produce antibodies against the virus or bacteria that caused it. Chronic hepatitis does not go away over time instead, it results in permanent damage to the liver. This can lead to cirrhosis, cancer, or need for a transplant.
Cirrhosis can be diagnosed based on the results of a physical examination and laboratory tests. Diagnostic tools include blood tests, imaging scans, and endoscopy.
Also Check: How Do I Know I Have Hepatitis B
Where Do You Feel Liver Pain
Most people feel it as a dull, throbbing sensation in the upper right abdomen. Liver pain can also feel like a stabbing sensation that takes your breath away. Sometimes this pain is accompanied by swelling, and occasionally people feel radiating liver pain in their back or in their right shoulder blade.
Biological Role Of Insulin
Insulin, after binding its receptor, induces the phosphorylation of receptor substrates in the liver and muscles, and triggers several steps toward the transactivation of glucose transporter-4 .This increases glucose uptake by cells and its storage as glycogen, and inhibits the net production of glucose by the liver, thus blocking glycogenolysis and neoglycogenesis. Moreover, insulin promotes lipid storage by inhibiting lipolysis. When insulin is unable to induce glucose uptake, pancreatic -cells increase insulin production and the hyperinsulinemic state prevents hyperglycemia. Thus, IR depends on insulin secretion and insulin sensitivity.
Read Also: Best Treatment For Hepatitis C
Steatosis In Chronic Hepatitis C
In chronic hepatitis C patients, the prevalence of steatosis ranges from 40% to 86% . The majority of patients with steatosis have mild steatosis affecting less than 30% of hepatocytes. Thus, steatosis occurs more frequently in patients with chronic hepatitis C than in the general population of adults in the Western world. Macrovesicular steatosis is found in the periportal region of the liver-different from the centrilobular distribution characteristic of NASH patients. Mild steatosis had been reported in nearly 40% of patients with HCV genotype 4.
Moderate or severe steatosis is significantly less frequent in genotype 4 than 3 chronic hepatitis C patients and similar between genotype 4 and 1. In non-diabetic, overweight patients, moderate or severe steatosis is present in only 10%-15% of genotype 4 or 1 compared with 40% of genotype 3 patients. Thus, hepatic steatosis in genotype 4 is mostly associated with metabolic factors, similar to those in genotype 1.
Influence Your Genes With Diet And Lifestyle
Even if you have a gene that predisposes you to fatty liver disease, you are not destined for liver problems. Diet and lifestyle can influence your genes for better or for worse. If you have the fatty liver disease gene, your diet and lifestyle can prevent the expression of these genes.
Conversely, you dont have to have the fatty liver disease gene to develop fatty liver disease. If you dont have the fatty liver gene, certain diet and lifestyle factors cause the development of fatty liver disease. Generally, a sedentary lifestyle and diet high in added sugars and saturated fat can induce epigenetic changes that accompany fatty liver disease.
A study conducted by researchers at the Department of General and Thoracic Surgery at the University Hospital Schleswig-Holstein in Kiel, Germany, assessed the DNA of patients with fatty liver disease before and after bariatric surgical treatment for weight loss. The analysis showed that genetic changes associated with fatty liver disease were reversed post-treatment, revealing the livers ability to respond positively to environmental changes.
You May Like: How Do Catch Hepatitis C
Delivery Of Fatty Acids From Peripheral Stores To The Liver
Triglycerides are stored in adipose tissue and released as FFAs into the circulation through the actions of lipoprotein lipase. FFAs released from peripheral stores are hydrophobic and are strongly bound to circulating albumin. FFAs are transported by albumin to the liver where they can then be used as a substitute for -oxidation, stored as TAG, or exported as VLDL.
Excess glucose is converted to the liver, the backbone of most amino acids, can be converted to pyruvate and then to acetyl-coenzyme A , which feeds directly into cytosolic fatty acid synthesis.
Processes that can lead to excessive FFAs delivery or impaired -oxidation or secretion can lead to hepatic steatosis, increased mitochondrial reactive oxygen species and lipid peroxidation products.
When To Visit A Doctor
If you have a family history of renal disease or are developing symptoms that you believe might be associated with renal parenchymal disease, schedule a visit with your doctor as soon as possible to go over your symptoms and medical history and decide whether further testing might be necessary or appropriate.
The earlier you get a diagnosis of your condition, the better it will be for your future health, and it will also mean potentially earlier treatment.
Read Also: How Can You Spread Hepatitis C
What Is Parenchymal Liver Disease
In the clinical setting, chronic liver disease is a disease process of the liver that involves the gradual destruction and regeneration of the liver parenchyma, leading to fibrosis and cirrhosis. The term “chronic liver disease” refers to a liver ailment that lasts for at least six months. There are several different types of chronic liver diseases, including viral hepatitis, alcoholic liver disease, and fatty liver disease.
Chronic liver disease can be asymptomatic or it may cause abdominal pain, diarrhea, nausea, vomiting, jaundice , muscle weakness, weight loss, and fatigue. If left untreated, chronic liver disease can lead to serious complications such as liver failure, ascites , encephalopathy , bleeding from esophageal varices , and portal hypertension .
The two main forms of chronic liver disease are viral hepatitis and alcoholic liver disease. Both forms can occur independently or together. Hepatitis B and C are viruses that can damage the liver, causing inflammation. Alcoholism affects how the body processes alcohol it can also cause other health problems that can lead to liver disease, such as high levels of cholesterol or triglycerides. Other factors such as medications or autoimmune disorders can also lead to chronic liver disease.
Expression Of The Fatty Liver Disease Gene Depends On Environment
Your DNA an abbreviation short for deoxyribonucleic acid is a code that makes you human and determines your individual traits. Some traits, such as eye color, are influenced by just two genes and based on your inherited genes, will remain set in stone for your lifetime.
Other traits, such as personality, are much more complex and described as polygenic traits since they are influenced by a large number of different genes. An individuals personality like introversion or open-mindedness is highly influenced by both genes and the environment. For example, a naturally introverted child may become more extroverted over time in response to positive experiences with family and peers.
The expression of the genes contributing to fatty liver disease is comparable to more complex traits, like personality. Inheriting certain forms of the gene may predispose you to fatty liver disease under certain environmental conditions.
You May Like: How Can Someone Get Hepatitis B
Vascular And Biliary Architecture
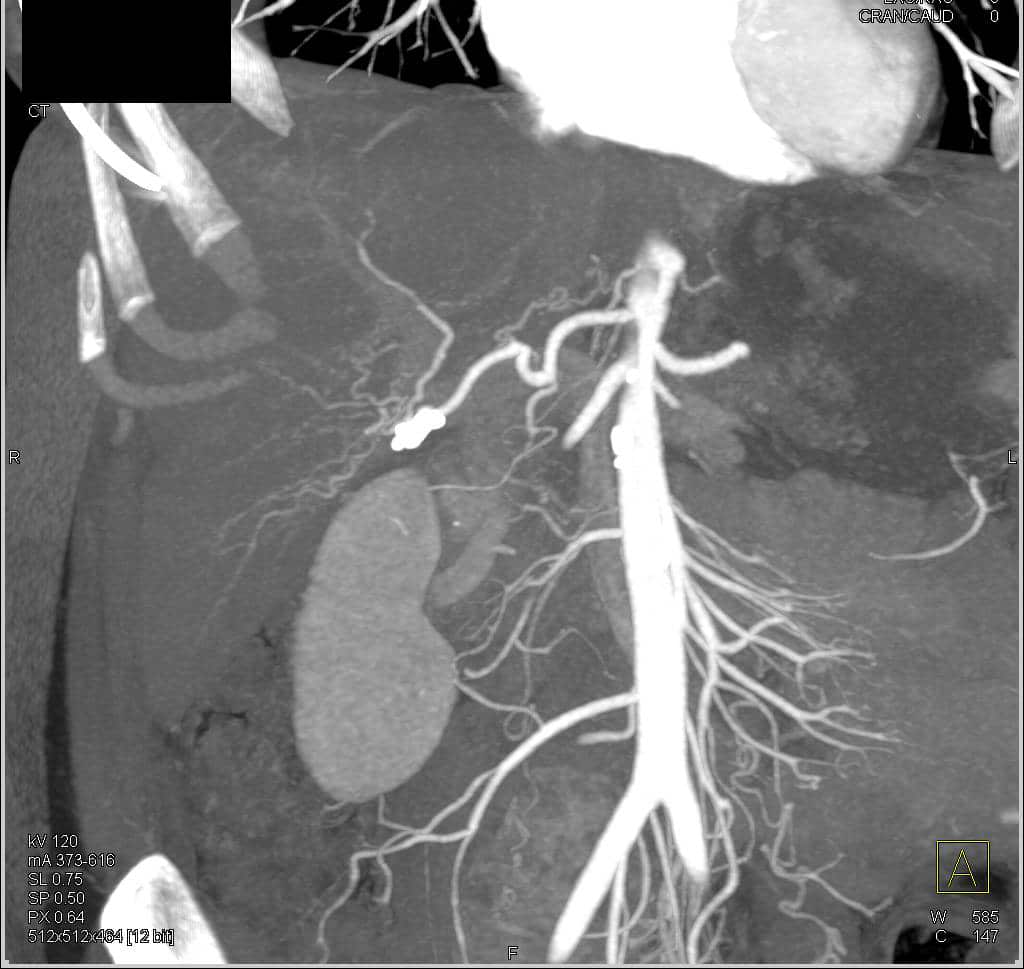
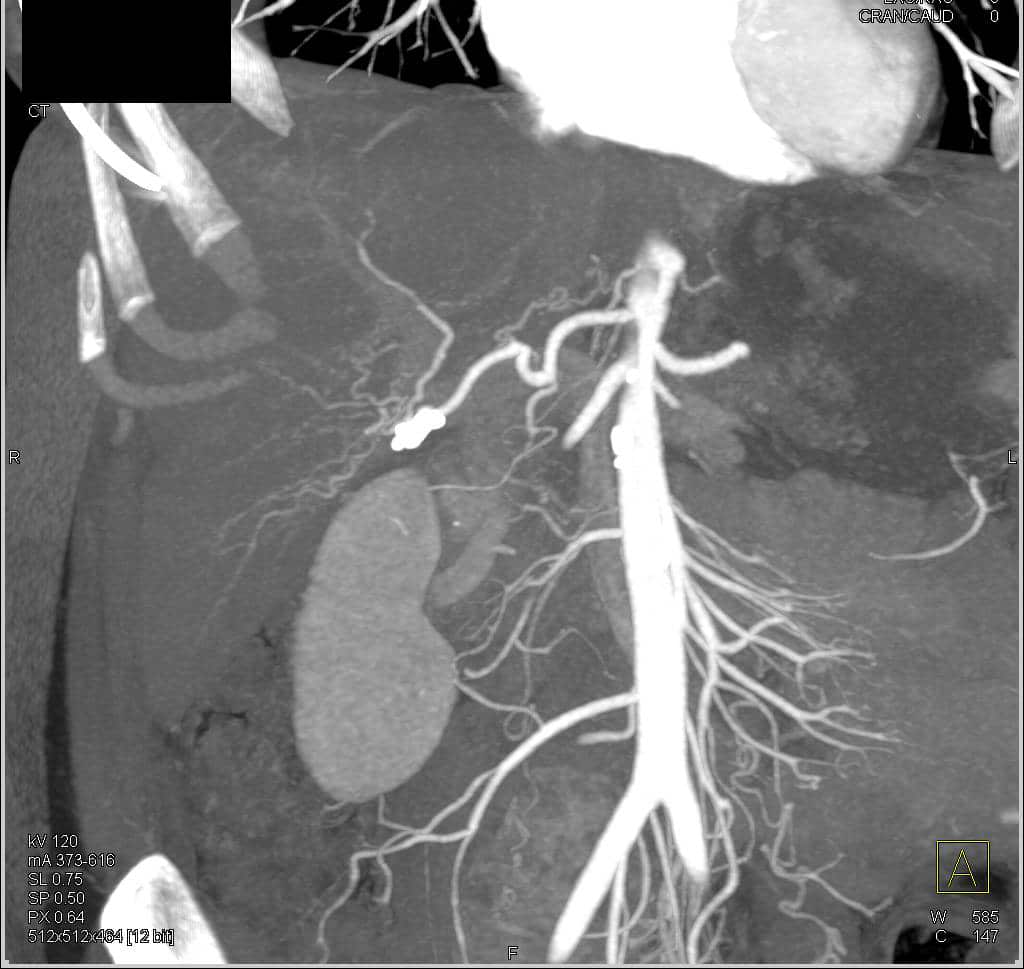
The generally smooth liver parenchyma is traversed by several vascular structures: the portal veins, hepatic veins, hepatic arteries and the bile ducts. The liver is unique in receiving two blood supplies: the hepatic artery provides approximately 25% of the inflow at rest, in the form of oxygenated blood direct from the systemic arterial system the portal vein provides partially deoxygenated blood via the bowel, spleen and other viscera. Both pass through the porta hepatis, along with the bile duct. Venous drainage occurs via the hepatic veins, directly into the upper inferior vena cava to the right atrium of the heart .
The common hepatic artery is normally a branch of the coeliac axis, and divides into left and right branches at or somewhere before the porta hepatis. In around 50% of people variations in its origin occur,3 including separate left and right supplies from the coeliac axis and superior mesenteric artery , or common supply from the SMA alone. Identification of these vessels is important in preoperative assessment of liver transplant recipients. The diameter of the normal common hepatic artery is 5 mm or less. On ultrasound images, the artery is roughly parallel with the portal vein at the porta, but is more tortuous, and is seen coming in and out of the scan plane.
C.J. YOON, J.W. CHUNG, in, 2007
Complications Of Renal Parenchymal Disease
The renal parenchymal disease can exact a heavy toll on your kidney functions and overall health. There is a wide range of complications and issues that can arise as you try to manage the disease and maintain your quality of life. One of the most notable complications of the renal parenchymal disease is the high incidence of patients that develop secondary hypertension.
The development of secondary hypertension opens the door to other health problems and threats to your well-being. When secondary hypertension develops, your doctor must take an aggressive approach to manage that condition in combination with renal parenchymal disease so as not to cause more severe and rapid deterioration of your overall health.
Also Check: What Does It Mean To Have Hepatitis B
Which Fruit Is Best For Liver
Fill your fruit basket with apples, grapes and citrus fruits like oranges and lemons, which are proven to be liver-friendly fruits. Consume grapes as it is, in the form of a grape juice or supplement your diet with grape seed extracts to increase antioxidant levels in your body and protect your liver from toxins.
Fate Of Fatty Acids In The Liver
In the fasting state, adipocyte TAG is hydrolyzed to release FFAs, which are transported to the liver where they can serve as substrates for mitochondrial -oxidation. -oxidation of fatty acids is a major source of energy needed to maintain liver viability during fasting. It is also the source of the ketone bodies, acetoacetate and acetone. These are released into the blood and are essential fuel sources for peripheral tissues, when glucose is in short supply. Defects in hepatic -oxidation cause microvesicular steatosis of the liver, increase in oxidative stress due to extramitochondrial oxidative stress. ROS and peroxidation products lead to cytotoxic events, release of proinflammatory cytokines and activation of hepatic stellate cells and fibrosis.
Don’t Miss: Is Hepatitis C An Sti
Pathogenesis Of Steatosis In Chronic Hepatitis C
IR emerges as a very important host factor, mainly because it has been related to steatosis development, fibrosis progression and non-response to peg-interferon plus ribavirin. HCV directly associates with IR independent of the visceral fat area in non-obese and non-diabetic patients. HCV is directly associated with IR in a dose-dependent manner, independent of the visceral adipose tissue area.
Factors associated with steatosis in chronic hepatitis C are: viral factor host factors , and drug therapy . The mechanisms underlying the development of parenchymal steatosis in HCV infection are not exactly known.
The first mechanism supposes that HCV core protein may block assembly of Apo-A1-A2 with TAG. This will result in decreased export of TAG bound to apolipoprotein- as VLDL out of hepatocyte, which is corrected by antiviral therapy. Others propose that the core protein induces oxidative stress within the mitochondria that contributes to lipid accumulation. Though the exact mechanism remains elusive, it seems that HCV itself can directly induce steatosis in genotype 3 by the cytopathic effect of high titer of intracytoplasmic negative strand HCV RNA.
The main deleterious effect of IR in chronic hepatitis C is the ability to promote fibrosis progression. High serum glucose levels have been found associated with an increased rate of fibrosis progression, even greater than overweight.
Steatosis And Fibrosis Progression In Hcv
High levels of TNF- have also been observed in human chronic hepatitis C patients. TNF- has been shown to induce IR in experimental animals and cultured cells. Inhibition of tyrosine phosphorylation of IRS 1 and 2 may be one of the mechanisms by which a high level of TNF- causes IR. Administration of an anti-TNF- antibody restores insulin sensitivity. These results provide direct experimental evidence for the contribution of HCV in the development of IR. There are experimental arguments for a direct role of insulin in fibrosis progression in HCV infection.
Epidemiological studies indicating that the state of IR now associated with NASH is also associated with an increased risk of HCC. It is worth mentioning that diabetes increases the risk of chronic liver disease and HCC.
Read Also: Where Can I Get Tested For Hepatitis C
Presenting Conditions In Haemochromatosis
- Skin pigmentation
- Sexual dysfunction
Patients who are homozygous for the mutation should have regular venesection to prevent further tissue damage. Heterozygotes are asymptomatic and do not require treatment. Cardiac function is often improved by venesection but diabetes, arthritis, and hepatic fibrosis do not improve. This emphasises the need for early recognition and treatment.