Deterrence And Patient Education
Patient education remains one of the most important components in preventative measures regarding HBV infection.
Education should be provided to expecting parents about the importance of vaccination and to clarify erroneous beliefs about vaccinations.Patient education should also include counseling about the avoidance of risky behaviors that predispose an individual to be infected, including promiscuous sexual activity or intravenous drug abuse. They should also be advised not to share items such as shaving razors, toothbrushes, or hair combs due to possible transmission via mucosal contact or through microtrauma to protective barriers.
Public Health Significance And Occurrence Of Hepatitis D
Hepatitis D occurs worldwide. It is most prevalent in countries and communities that have a high risk of hepatitis B, including Africa, South America, Romania and parts of Russia among haemophiliacs, people who inject drugs and others who come in frequent contact with blood in institutions for the developmentally disabled and, to a lesser extent, among men who have sex with men.
Outbreaks have been reported in tropical South America , in the Central African Republic, and among people who inject drugs in the United States.
In recent years, as the prevalence of chronic hepatitis B surface antigen carriers has decreased, there has been a decline in both acute and chronic HDV in the Mediterranean area and in many other parts of the world. Better sanitation and social standards may have also contributed to the decline.
New areas of high HDV prevalence continue to appear and include Albania, areas of China, northern India and Japan .
Despite high rates of hepatitis B in Asian countries, the incidence of hepatitis D is lower. Hepatitis D is uncommon in Australia. An average of 13 cases has been reported per year in Victoria since 2010.
Information To Collect For Chronic Hepatitis B Infection
The following information is epidemiologically important to collect in a case investigation for chronic hepatitis B infection. Additional information may also be collected at the direction/jurisdiction of the state health department.
- Demographic information
- Laboratory results
- Risk behaviors/exposures
- Pregnancy status. All HBsAg-positive pregnant women should be reported to the Perinatal Hepatitis B Prevention Program manager so that they can be tracked and their infants can receive appropriate case management
The recommended elements of case investigation and follow-up of persons with chronic hepatitis B virus infection are detailed elsewhere. The following should be included:
- Contact investigation and prophylaxis: Provision of hepatitis B vaccination for sexual, household, and other contacts of persons with hepatitis B, and counseling to prevent transmission to others
- Counseling and referral for medical management, including
- assessing for biochemical evidence of chronic liver disease, and
- evaluating eligibility for antiviral treatment
Also Check: Hepatitis A Vaccine Side Effects
Also Check: How Many Genotypes Of Hepatitis C Are There
Epidemiology And Risk Factors
The seroprevalence of HDV among HBsAg-positive carriers has substantial variations worldwide. These are depicted in Table 1. Interestingly, more recent data have shown that 8% of the general Mongolian population is estimated to be positive for HDV . Notably, in the USA, the prevalence of HDV among HBV carriers has been reported to range from 2% to 50%, depending on the patient population . A large study of the US Veterans Affairs medical system more recently reported an HDV seroprevalence of 3.4% among patients with chronic HBV who are tested for HDV . A study using the National Health and Nutrition Examination Survey reported a HDV seroprevalence of 42% among HBV carriers . Finally, the highest estimation of HDV seroprevalence came from a study of HBV-positive intravenous drug users , which showed that the seroprevalence of HDV increased from 29% in 19881989 to 50% in 20052006 . However, a general lack of HDV RNA validation in these studies prevents estimation of true HDV prevalence.
When To Contact A Doctor
Anyone who suspects that they have come into contact with HBV should consult a doctor as soon as possible.
A doctor can provide postexposure prophylaxis through the vaccines and a drug called hepatitis B immune globulin. PEP can prevent infection and liver damage.
A person should also contact a doctor if they notice any of the symptoms of hepatitis B or if they know they have hepatitis B, and their symptoms worsen.
Hepatitis B is a viral infection that impacts the liver.
Recommended Reading: How Do You Contract Hepatitis B
Important Questions And Needs For Future Research
How To Prevent Hepatitis C
Without treatment, HCV can lead to cirrhosis of the liver and even liver failure. But its a preventable illness. Here are three ways to prevent getting hepatitis C:
- If you have a history of illicit drug use, get help in trying to quit. Avoiding contact with needles used by others is the biggest single step you can take to prevent infection or reinfection.
- If youre a healthcare worker, always practice universal precautions when handling used needles, syringes, and blades.
- Avoid getting a tattoo or piecing in an unregulated setting, as any infected needle can transmit the virus.
Recommended Reading: How Soon Do Hepatitis C Symptoms Appear
Viral Structure And Life Cycle
Hepatitis D virus viral life cycle and sites of drug target. 1. Hepatitis D virus virion attaches to the hepatocyte via interaction between hepatitis B surface antigen proteins and the sodium taurocholate cotransporting polypeptide , a multiple transmembrane transporter. 2. HDV ribonucleoprotein is translocated to nucleus mediated by the hepatitis D antigen . 3. HDV genome replication occurs via a rolling-circle mechanism. 4. HDV antigenome is transported out of the nucleus to the endoplasmic reticulum . 5. HDV antigenome is translated in the ER into small HDAg and large HDAg . 6. L-HDAg undergoes prenylation prior to assembly. 7. S-HDAg is transported back to the nucleus where it supports HDV replication. 8. New HDAg molecules are associated with new transcripts of genomic RNA to form new RNPs that are exported to the cytoplasm. 9. New HDV RNP associates with hepatitis B virus envelop proteins and assembled into HDV virions. 10. Completed HDV virions are released from the hepatocyte via the trans-Golgi network.
Finally, once the RNP interacts with the envelop protein of HBV and the HDV is assembled, the HDV virion is now ready for release. The HDV virion is released via the trans-Golgi network, where it can go on to infect other hepatocytes. However, the exact mechanism of HDV-virion release remains unknown .
How Can Hepatitis D Be Prevented
The only known way to prevent hepatitis D is to avoid infection with hepatitis B. You can take the following preventive measures to reduce your risk for hepatitis B:
- Get vaccinated. Theres a vaccine for hepatitis B that all children should receive. Adults who are at high risk for infection, such as those who use intravenous drugs, should also be vaccinated. The vaccination is usually given in a series of three injections over a period of six months.
- Use protection. Always practice safe sex by using a condom with all of your sexual partners. You should never engage in unprotected sex unless youre certain your partner isnt infected with hepatitis or any other sexually transmitted infection.
- Avoid or stop using recreational drugs that can be injected, such as heroin or cocaine. If youre unable to stop using drugs, make sure to use a sterile needle each time you inject them. Never share needles with other people.
- Be cautious about tattoos and piercings. Go to a trustworthy shop whenever you get a piercing or tattoo. Ask how the equipment is cleaned and make sure the employees use sterile needles.
Last medically reviewed on May 17, 2018
Also Check: Hepatitis How Is It Transmitted
Signs And Symptoms Of Chronic Hbv
People with CHB often do not have symptoms, so those with the disease may have no way of knowing that they are infected. However, some complain of fatigue, aches and pains, fever, loss of appetite, nausea and abdominal pain.
The majority of acute HBV infections are also asymptomatic but around 30% of adults will present with jaundice, fatigue, poor appetite, weight loss, nausea and vomiting, abdominal pain, pyrexia, dark urine and light stools .
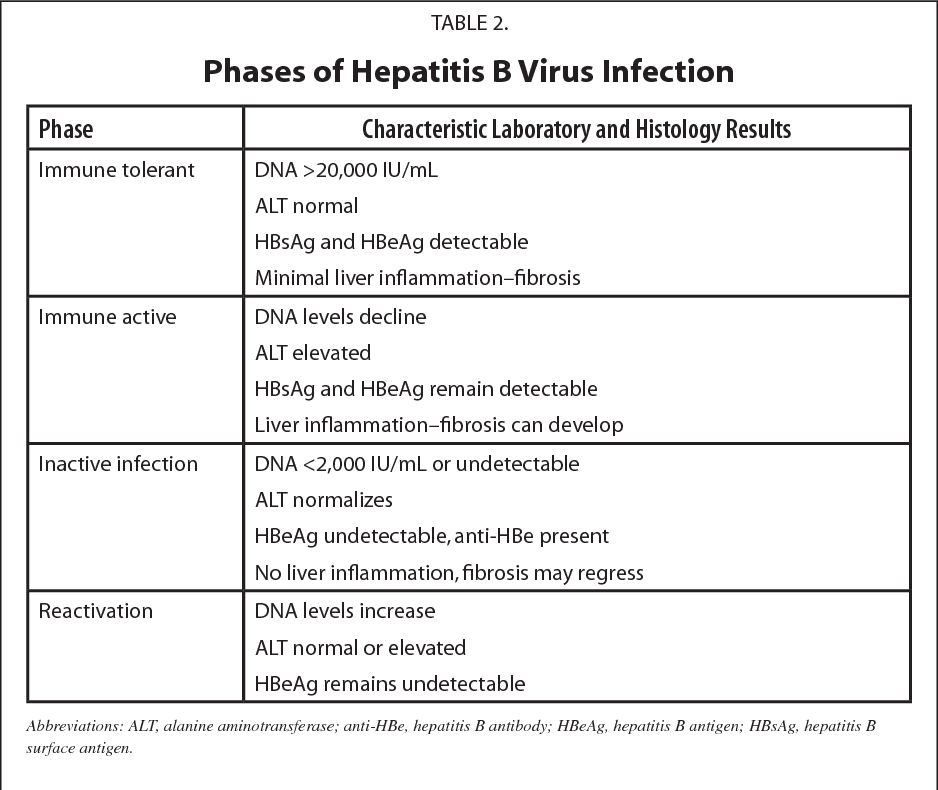
Diagnosis
HBV is diagnosed with a blood test to detect hepatitis B surface antigen . The different HBV serological markers may be used collectively to determine a persons HBV status. These are shown in Table 4.
HBV testing
Since 2000, all pregnant women have been tested for HBV. The National Institute for Health and Care Excellence has published a new guideline to promote HBV and hepatitis C virus testing. The guideline recommends that the at-risk groups listed in Box 1 are tested for HBV, and given counselling before and afterwards.
Box 1. Who to screen
The following at-risk groups should be tested for HBV:
All those who test positive for HBV surface antigen should be referred to a specialist centre within six weeks. Pregnant women should be assessed by a specialist within six weeks of receiving the screening test result so treatment can be offered in the third trimester if necessary .
Hepatitis D Incubation Period
The incubation period of hepatitis D virus is 2 to 8 weeks. Anyhow, If we count in days they become 14 to 56 days. This is a period in which the tiny hepatitis D virus affects the liver. When hepatitis D virus enters a patient with chronic hepatitis D, it takes 14 to 56 days to cause the disease hepatitis D and show the symptoms. Moreover, When D virus enters the liver, the readily present Hepatitis D virus Shares the envelope of glycoprotein to the HDV. This is an ideal situation for the D virus to live and to infect the patient.
Read Also: How Can You Get Hepatitis A And B
Modes Of Transmission And Epidemiology
HDV is transmitted mainly by blood or other body fluids . It shares the transmission modes of HBV: percutaneous and sexual transmission .
Five to 20 million people are chronic carriers of HDV worldwide, and it is estimated that approximately 5 to 10% of chronic HBV carriers have anti-HDV antibodies. The prevalence of HDV among HBV carriers, however, varies considerably from region to region. France is a region of low prevalence.
Where Is The Hepatitis B Virus Found And How Is It Transmitted
Blood is the major source of the hepatitis B virus in the workplace. It can also be found in other tissues and body fluids, but in much lower concentrations. The risk of transmission varies according to the specific source. The virus can survive outside the body for at least 7 days and still be able to cause infection.
Read Also: Diagnostic Test For Hepatitis B
Hepatitis B Vaccine Schedules For Infants By Maternal Hbsag Status
| Maternal HBsAg Status | |
|---|---|
| 4 | 6 mos¶ |
* Mothers should have blood drawn and tested for HBsAg as soon as possible after admission for delivery if the mother is found to be HBsAg positive, the infant should receive HBIG as soon as possible but no later than age 7 days. Pediarix and Vaxelis should not be administered before age 6 weeks.§ HBIG should be administered at a separate anatomical site from vaccine.¶ The final dose in the vaccine series should not be administered before age 24 weeks .
Also Check: What Is Hepatitis C And How Do You Catch It
Is Hepatitis B Curable
Theres currently no known cure for hepatitis B, but there are many ways you can prevent infection and avoid transmitting the virus to others.
The most effective and safe way to prevent hepatitis B is to get vaccinated. You can also use barrier methods, like condoms, when having sex and avoid sharing needles.
Donât Miss: Hepatitis B Antiviral Drugs Cost
Recommended Reading: Hepatitis B And C Test Price
How Long Can You Live With Hepatitis B
Most people who contract hepatitis B during adulthood fully recover within 1 to 3 months.
People with chronic hepatitis B may have a higher risk of developing long-term liver problems, like cirrhosis or liver cancer, which require treatment and may be life threatening.
Keep in mind that the risk of developing chronic hepatitis B is higher for babies and children, especially if they have not been vaccinated against the virus.
Screening And Risk Factors
Screening of all pregnant women for HBsAg to identify infants requiring postexposure prophylaxis has been recommended since 1988. Universal infant hepatitis B immunization has been recommended since 1991, and universal adolescent hepatitis B immunization since 1995. In the United States, approximately 21,000 HBsAg-positive women give birth annually. Without postexposure prophylaxis to prevent perinatal HBV infection, it is estimated that HBV transmission would occur in 36% of infants born to HBsAg-positive women. Furthermore, before the implementation of universal infant hepatitis B immunization, an additional 16,000 children younger than 10 years old were infected annually in the United States through exposure to HBsAg-positive household members or community contacts. Populations with the highest rates of these early childhood infections included Alaska Natives, children of Pacific Islander parents, and children of first-generation immigrants from countries where HBV is of intermediate or high endemicity.
Among persons who reported risk behaviors/exposures in 2016, the most frequently reported risk behavior/exposure for acute, symptomatic hepatitis B was injection drug use , followed by sex with multiple partners . More than half of persons with newly acquired hepatitis B were previously seen in medical settings where hepatitis B vaccine is routinely recommended, such as sexually transmitted disease treatment clinics or drug treatment centers.
Also Check: Hepatitis B Blood Test Results
Pathogenesis Of Hepatitis D
HDV only replicates in the liver, and therefore pathologic changes are limited to this organ. Liver damage in HDV infection is thought to be mostly immune mediated, although initial data from experimentally infected chimpanzees had suggested a direct cytopathic effect of HDV on hepatocytes, particularly during the primary infection . It was observed that in acute hepatitis D, infected hepatocytes were undergoing degenerative changes characterized by shrunken eosinophilic cytoplasm and pyknotic nuclei, with minimal inflammatory cells in the liver parenchyma, consistent with a cytopathic hepatocellular damage. These findings were reported both in vitro and in human studies . The small isoform of HDAg expressed was suggested to be responsible for this direct cytopathic effect of HDV . However, other results and in vivo observations, such as the presence of inflammatory cells surrounding the infected hepatocytes and the presence of various autoantibodies in the serum of patients, argue for a mostly immune-mediated liver damage. On the other hand, because HBV replication is usually suppressed by HDV, liver damage is believed to be induced mostly by HDV rather than by HBV.
Acute Hepatitis B Infection
An acute hepatitis B infection may last up to six months and infected persons are able to pass the virus to others during this time. A simple blood test can let a person know if the hepatitis B virus is in their blood or if they have successfully gotten rid of the virus. The doctor should periodically test your blood over the six-month period to monitor the health of your liver and check progress towards recovery. In a person who has recovered from an acute hepatitis B infection, a taken six-months after initial diagnosis will show that there is no more hepatitis B virus in your blood.
Being diagnosed with acute hepatitis B can be difficult. As you move through the initial six-month period, there are tips and strategies to help.
Until your health care provider confirms that the blood test shows that there is no more hepatitis B virus in your blood, it is important to protect others from a possible infection.
It is also important to have your sexual partner and family members get tested for hepatitis B. If they have not been infected and have not received the hepatitis B vaccine then they should also start the hepatitis B vaccine series.
Be sure to follow-up with your health care provider for any additional blood tests that are needed to confirm your recovery from an acute infection.
Also Check: How Did Naomi Judd Get Hepatitis C
You May Like: How Often Should You Be Tested For Hepatitis C
Perinatal Hepatitis B Virus Infection
Clinical description
Perinatal hepatitis B in a child 24 months of age may range from asymptomatic to fulminant hepatitis.
Laboratory criteria for diagnosis consists of one or more of the following
- Positive HBsAg test OR
- Positive HBV DNA
Case classification
Confirmed: Child born in the United States or a United States territory to a HBV-infected mother and positive for HBsAg at 1 month of age and 24 months of age OR positive for HBeAg or HBV DNA at 9 months of age and 24 months of age.
Probable: Child born in the United States or a United States territory and positive for HBsAg at 1 month of age and 24 months of age OR positive for HBeAg or HBV DNA at 9 months of age and 24 months of age, but whose mothers hepatitis B status is unknown.
Infants born to HBsAg-positive mothers should receive the first dose of hepatitis B vaccine and HBIG within 12 hours of birth, followed by the second and third doses of vaccine at 1 and 6 months of age, respectively, if receiving the single-antigen vaccine. Scheduling will be different if the infant received a combination vaccine or if the infant weighed < 2,000 grams at birth. Postvaccination serologic testing for HBsAg and anti-HBs is recommended at age 912 months . If the initial dose of the hepatitis B vaccine and HBIG are delayed for more than 1 month after birth, testing for HBsAg may determine if the infant is already infected.
Read Also: Is Milk Thistle Good For Hepatitis C