Ii Diagnostic Confirmation: Are You Sure Your Patient Has Hepatitis C
Most people are asymptomatic or have only nonspecific symptoms in the acute phase after initial infection. Diagnosis of acute hepatitis C is therefore rarely made. Chronic hepatitis C may be identified at the time of workup for causes of aminotransferase elevations however, the majority of people with chronic HCV infection remain asymptomatic until the disease progresses to advanced stages of fibrosis or cirrhosis.
Presence of anti-HCV antibodies confirms prior infection with HCV. To determine if a patient has current HCV infection, HCV RNA is measured. A patient with detectable serum HCV RNA has chronic HCV infection. A patient with a positive HCV Ab but undetectable HCV RNA was previously exposed to HCV but either spontaneously cleared the infection or was cured by prior treatment . During the early phases of an acute infection, patients may not have developed HCV antibodies therefore, if acute HCV infection is suspected, HCV RNA should be checked despite a negative HCV Ab result. Additionally, patients who are immunocompromised may have negative antibody testing but active infection as indicated by a positive HCV RNA test. In such patients with aminotransferase elevations that remain unexplained after typical causes are excluded, HCV infection should be fully excluded by RNA testing.
Liver Cancer And Hepatitis C
- Reactions 0 reactions
Liver cancer is a risk for the more than 3 million people in the United States who have chronic hepatitis C. Research shows the impact of liver cancer on Americans is growing, along with the cases of hepatitis C.1
The rate of liver cancer in the United States rose by 20 percent between 2008 and 2017. Some states saw increases of more than 50 percent, with North Dakota topping the list at 107 percent. The rate of liver cancer dropped in only 3 states in the nation.2
The number of deaths from liver cancer in the United States also grew by 18 percent between 2008 and 2017. The American Cancer Society expects deaths from liver cancer to exceed 30,000 by the end of 2020. The deaths are not far behind the count of new liver cancer diagnoses, which will likely total almost 43,000 in 2020.2,3
The Centers for Disease Control and Prevention points to 2 likely causes of the increase in liver cancer cases:4,5
- A surge in new HCV infections, which exceeded an estimated 50,000 in 2018
- Improved methods for reporting cases of hepatitis C virus infections
Hepatitis C Virus Transgenic Mice
The transgenic mouse system has widely been used to study HCV proteins and carcinogenesis . Hepatitis C virus gene products have been expressed either alone or in combination in the liver of transgenic mice by using different liver-specific promoters. As already mentioned, three different HCV core transgenic lines develop liver steatosis and HCCs but other animals show only steatosis or different phenotypes , depending on the promoter used, the context of expression and the mouse strain background. NS5A transgenic mice, in spite of the pleiotropic functions of the protein in vitro, do not have any significant phenotype . The transgenic mice reported so far in HCV transgenes have always been expressed from constitutive promoters. Besides from not being amenable to any postnatal regulation, constitutive expression of HCV proteins in utero may easily induce adaptive or compensatory epigenetic that can profoundly affect the animal phenotype.
Table 1 Transgenic mice expressing HCV gene products
You May Like: How Hepatitis C Affects The Body
Who Is Most At Risk Of Contracting Hepatitis C
You have a high risk of contracting hepatitis C if you:
- use or have used injection drugs even if it was just once or many years ago
- have received blood or blood products or an organ transplant before July 1990 in Canada
- have been in jail or
- have been injected or scratched during vaccination, surgery, blood transfusion or a religious/ceremonial ritual in regions where hepatitis C is common.
You have a high moderate risk of contracting hepatitis C if you:
- have tattoos or body piercing
- have multiple sexual partners
- have a sexually transmitted infection , including HIV or lymphogranuloma venereum
- have experienced traumatic sex or rough sex or have used sex toys or fisting that can tear body tissue
- have vaginal sex during menstruation
- have received a kidney treatment
- have received an accidental injury from a needle or syringe
- have another infectious disease
- were born to a hepatitis C infected mother or
- have a sexual partner infected with hepatitis C.
Hepatitis C is NOT passed from person to person by:
- coughing, sneezing
- breastfeeding unless your nipples are cracked and bleeding or
- oral sex, unless blood is present.
Treatment Options For Hep C And Nhl
HCV treatment involves antiviral medication and focuses on reducing liver inflammation and preventing complications. The length of treatment varies depending on the extent of liver damage.
The goal is to clear the virus from the body before liver damage occurs. HCV becomes chronic if left untreated for more than about 6 months.
Chronic hep C can be a lifelong infection, if left untreated. In the case of severe chronic hepatitis C, which has led to liver damage, known as cirrhosis, a liver transplant may be required.
You May Like: What Is Included In A Hepatitis Panel
V Patient Safety And Quality Measures
In addition to traditional risk groups, the latest guidelines from CDC recommend one-time testing for all persons born during 1945-1965 without prior ascertainment of HCV risk. Studies have shown that point of care testing in urban hospital emergency departments can also identify a substantial number of new cases. All newly detected HCV cases should be referred to a specialist for further evaluation and consideration for antiviral treatment.
All patients with chronic hepatitis C should be tested for hepatitis A and hepatitis B and if found negative, should be vaccinated against hepatitis A and B as per the standard protocol.
All patients with chronic hepatitis C should be counselled on the risk of transmission to minimize transmission to others:
-
Patients should be informed about the low but present risk for transmission with sex partners.
-
Sharing personal items that might have blood on them, such as toothbrushes or razors, can pose a risk to others.
-
Cuts and sores on the skin should be covered to keep from spreading infectious blood or secretions.
-
Donating blood, organs, tissue, or semen can spread HCV to others.
-
HCV is not spread by sneezing, hugging, holding hands, coughing, sharing eating utensils or drinking glasses, or through food or water.
-
Patients may benefit from a joining support group.
Are People With Liver Cancer Considered For Liver Transplantation
Most cancers of the liver begin elsewhere in the body and are spread to the liver. These cancers are not curable through liver transplantation. Tumours that start in the liver are usually detected in an advanced stage. They are also rarely cured by a liver transplant. If the primary liver cancer is small and confined to the liver, a liver transplant may be considered.
Are their treatments for secondary liver cancers?
The liver is involved in approximately one-third of all cancers and often those that begin in the gastrointestinal tract, colon, pancreas, breast and lung. The risk factors involved in this type of liver cancer are numerous given that the cancers start elsewhere. The prognosis for people with secondary liver tumours depends on the primary site of malignancy. In general, people do not live longer than one year from the diagnosis of cancer spreading to the liver . Treatments for secondary liver cancers remain unsatisfactory but include surgery, chemotherapy, immunotherapy, and embolization.
Read Also: Royal Canin Hepatic Dry Dog Food
Diagnosis Of Hepatitis B
Blood tests are available to determine if you are or have been infected with hepatitis B. It may take 6 months from the time of infection before a blood test can detect antibodies to hepatitis B, so follow-up testing may be required. During this 6-month period, until you know whether you are infected or not, take action to prevent potential infection of other people.
There are also tests that can assess liver damage from hepatitis B. The interpretation of these tests can be complicated and specialist advice is needed, so talk to your doctor.
All pregnant women are tested for hepatitis B. If you are found to have chronic hepatitis B, your doctor can help reduce the risk of transferring the infection to your newborn child.
How Can I Reduce My Risk Of Hiv
The best way to avoid HIV-linked cancers is to avoid HIV infection. But if you do have an HIV infection, anti-retroviral therapy can reduce both the effects of the infection and the risk of HIV-linked cancer. Since ART became available, cases of cancers linked to HIV have gone down.
Whether you are on ART or not, its really important to listen to your body and speak to a health professional if somethings not quite right. Spotting cancer at an early stage can make a real difference.
And remember, around 4 in 10 cancers in the UK could be prevented. Things like stopping smoking, cutting down on alcohol and staying safe in the sun can have a big impact on your cancer risk.
Also Check: How Can You Get Hepatitis B
Effect Of Hcv Cure On Hcc Development
Fig. 1
Natural history of HCV-related HCC development and modulation by anti-HCV therapies. Progressive liver fibrosis along with aging gradually increases the risk of hepatocarcinogenesis, which could be further accelerated by several host and viral risk factors. Annual incidences of HCC development and recurrence after DAA-based SVR were estimated from retrospective and prospective studies summarized in Table . SVR induced by interferon- or DAA-based anti-HCV therapies may result in distinct post-SVR HCC risk. AFP alpha-fetoprotein, DAA direct-acting antiviral, HCV hepatitis C virus, HCC hepatocellular carcinoma, SVR sustained virologic response
E Common Pitfalls And Side
With the development of DAAs that do not require use of interferon, all patients with confirmed chronic HCV and no other life-threatening comorbidities should be referred to a liver specialist for treatment. Most patients experience little to no side effects during treatment. Those who achieve SVR have significantly decreased risk of progression to cirrhosis or worsening of liver function if already cirrhotic at the time of treatment. The risk for hepatocellular carcinoma likely also declines when HCV is cured.
No effective vaccine is available for prevention of HCV infection.
You May Like: What Vitamins Are Good For Hepatitis B
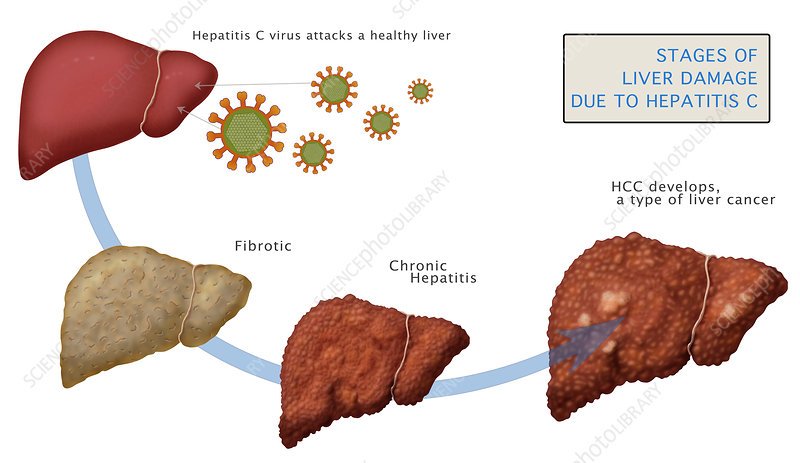
Does Hepatitis C Cause Liver Cancer
Long-term hepatitis C virus and hepatitis B virus infections are known to be the leading causes of liver cancer. This holds true around the world. In the United States, HCV causes more cases of liver cancer than HBV. In March 2016, the CDC reported that HCV accounts for 50 percent of all cases of liver cancer in the United States.5-7
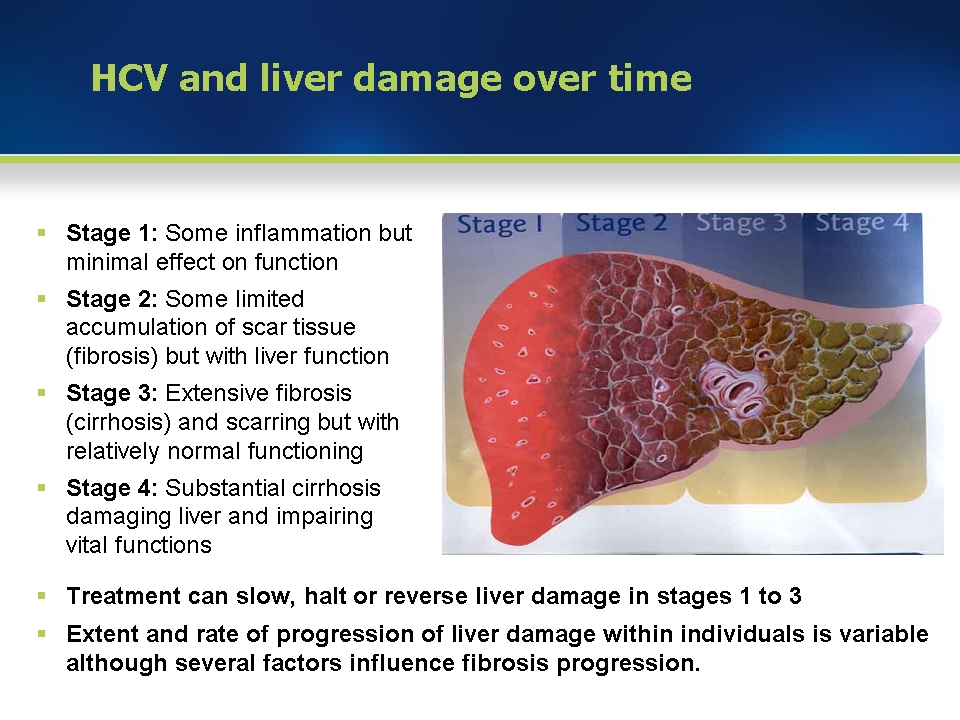
Liver cancer usually follows cirrhosis of the liver. Cirrhosis can occur in people with long-term hepatitis C. The infection destroys healthy liver cells and causes scar tissue to form in their place.2,5,7
What Are The Risk Factors For Getting Hepatitis B

Due to the way that hepatitis B spreads, people most at risk for getting infected include:
- Children whose mothers have been infected with hepatitis B.
- Children who have been adopted from countries with high rates of hepatitis B infection.
- People who have unprotected sex and/or have been diagnosed with a sexually transmitted infection.
- People who live with or work in an institutional setting, such as prisons or group homes.
- Healthcare providers and first responders.
- People who share needles or syringes.
- People who live in close quarters with a person with chronic hepatitis B infection.
- People who are on dialysis.
Donât Miss: What Is Included In A Hepatitis Panel
You May Like: Hepatitis B How Long Does It Last
Multidisciplinary Care For Patients
The Simmons Comprehensive Cancer Center and the Liver Transplant Program receive many referrals for the prevention and management of liver cancer treatment both incident and recurrent cases. Our cancer center is one of just 32 U.S. cancer research centers named by the National Cancer Institute as a National Clinical Trials Network Lead Academic Participating Site.
Only centers that meet rigorous standards for advanced cancer research can become NCI-designated. UT Southwestern is also home to one of the largest and most robust liver transplantation programs. Together, we care for patients awaiting liver transplants as well as those who have complex concurrent conditions such as decompensated cirrhosis from hepatitis C, alcohol-related liver disease, or non-alcoholic steatohepatitis.
As a multidisciplinary team, we approach patient care holistically with the goal of improving overall patient health along with their emergent liver condition. UT Southwestern continually pushes the boundaries of research in prevention and ongoing care. We anticipate that the profound findings from our research will usher in a new era in the care of patients with liver disease.
When Hep C Becomes Chronic
If youre one of the millions of people with ongoing hepatitis C infections, youre in a sort of no mans land, where your immune system keeps beating away at the virus and trying to kill infected liver cells, but it can never quite clear the infection. Over time, that constant assault on your liver causes inflammation, triggered by your bodys immune response. This, combined with the direct action of the virus, damages the organ. You have this smoldering fire in the liver, explains Houghton.
Don’t Miss: How Do You Get Hepatitis A B C
How Is Hepatitis C Spread
Hepatitis C spreads through contact with the blood of someone who has HCV. This contact may be through
- Sharing drug needles or other drug materials with someone who has HCV. In the United States, this is the most common way that people get hepatitis C.
- Getting an accidental stick with a needle that was used on someone who has HCV. This can happen in health care settings.
- Being tattooed or pierced with tools or inks that were not sterilized after being used on someone who has HCV
- Having contact with the blood or open sores of someone who has HCV
- Sharing personal care items that may have come in contact with another person’s blood, such as razors or toothbrushes
- Being born to a mother with HCV
- Having unprotected sex with someone who has HCV
Before 1992, hepatitis C was also commonly spread through blood transfusions and organ transplants. Since then, there has been routine testing of the U.S. blood supply for HCV. It is now very rare for someone to get HCV this way.
Other Hep C And Liver Cancer Causes
There are three additional reasons why hep C might lead to liver cancer. First, an infection creates a high turnover of liver cells, as both the virus and your immune system kill cells and your body works to replace them. Due to chronic inflammation, these new liver cells may contain damaged DNA, which increases the chance of developing cancer. Meanwhile, an inflamed liver may signal to your immune system to produce toxic chemicalsand these, too, might trigger cancerous mutations. Finally, the immune system may alter certain gene activity, encouraging tumor growth.
Don’t Miss: Causes And Symptoms Of Hepatitis
Genetic Risk Factors In Hepatocellular Carcinoma Development
Besides the well-known patient-specific risk factors for HCC development in CHB described above, evidence exists for a genetic predisposition due to single-nucleotide polymorphisms . Several SNPs associated with HCC have been reported and expression profiles generated . These polymorphisms alter biological pathways, including inflammation, oxidative stress, DNA repair, cell cycle and growth factors . The association between aflatoxin B1 and CHB is well established, and a concomitant SNP of GTSM1 and GSTT1 is associated with a dramatic increase in HCC risk . This indicates that the HCC risk attributable to specific polymorphisms depends on underlying risk factors and specific SNPs are associated with increased HCC risk in CHB. Such polymorphisms include SNPs of MDM2 and p53 XRCC3 HLA -DQ CTL-4 GLB1 and TGF-1 but no other proinflammatory cytokines or interleukin-10 . Nonetheless, these SNPs were mostly detected in collectives of CHB patients from the Far East or Asia and confirmatory studies in other patient populations are required.
How Do People Get Hepatitis C
HCV spreads by direct contact with an infected person’s blood and other body fluids. This can happen through:
- sharing drug needles and intranasal drug devices
- getting a tattoo or body piercing with unsterilized tools
- sexual contact
- passing of the infection from a pregnant woman to her unborn child
Children who have HCV most often acquired it as newborns from their mothers.
Thanks to blood screening and other health care precautions adopted in the early 1990s, the spread of HCV from hemodialysis, blood transfusions, or organ transplants is now rare.
It’s also rare, but possible, for someone to get HCV by sharing household items that might contain an infected person’s blood, such as razors, toothbrushes, or scissors.
Recommended Reading: What Are The Symptoms To Hepatitis C
What Are The Signs & Symptoms Of Hcv Infection
Most people with HCV have no symptoms. But even without symptoms, they can develop health problems decades later and can still pass the disease to others.
If symptoms do happen, it’s usually when the disease is very advanced. Symptoms can be similar to those of hepatitis A and hepatitis B and include:
- jaundice
- fever
- darker than usual urine or gray-colored stools
Hepatocellular Carcinoma Epidemiology Risk Factors And Treatment Options
Worldwide, liver cancer is the second leading cause of cancer-related death in men, with 745 000 deaths per year, and the sixth most common cancer, with rising incidence . HCC represents approximately 90% of all primary liver cancer cases, shows a clear gender disparity towards males and is a major cancer in less developed regions, with a correlation to HBV surface antigen prevalence. Chronic HBV and HCV infections represent the leading cause for HCC , with a total incidence of 16/100 000 globally. In most of Africa and Asia, HBV is the single leading risk factor for HCC, whereas in Japan, northern Europe and the USA HCV is the major risk factor . The risk of developing HCC is 10- to 25-fold higher in CHB compared with non-infected controls, and up to 17-fold increased in HCV-associated liver cirrhosis . While HCC in HCV infection rarely occurs without liver cirrhosis, CHB without any obvious liver inflammation per se confers a risk for HCC development. The highest risk for HCC development is associated with co-infection of HBV with HDV, HCV or HIV.
Recommended Reading: The Effects Of Hepatitis C