What Do I Ask The Doctor
When you visit the doctor, it helps to have questions written down ahead of time. You can also ask a family member or friend to go with you to take notes. Print this list of questions and take it to your next appointment.
- Do I need to get tested for hepatitis C?
- What puts me at risk for hepatitis C?
- How will you test me for hepatitis C?
- How long will it take to get my test results?
- How will I find out my test results?
- If I have hepatitis C, what will happen next?
- Can you give me some information about hepatitis C to take home with me?
Content last updated
How Common Is Hepatitis C
Some 4 million people in the U.S. have been infected with the hepatitis C virus, and these numbers are increasing. Hep C used to be thought of as a problem for baby boomers, but thats no longer the case. Were starting to see more infections in younger people, says Roger Chou, M.D, director of the Evidence Based Practice Center at Oregon Health & Science University in Portland and lead author of the medical review that informed the new screening guidelines.
Other Indications For Measuring Anti
In addition to screening, measuring anti-HCV can be useful in patients with symptoms of chronic liver disease patients who have other viral infections, including chronic fatigue, hepatitis B, HIV, intermittently abnormal ALT, or cirrhosis found on imaging tests or patients undergoing evaluation for organ transplantation.
Recommended Reading: Difference Between Fatty Liver And Hepatitis
Drawbacks To Screening For Hepatitis C
A patient’s worry or anxiety while waiting for test results, concerns about insurance coverage of evaluation and treatment, adverse effects of treatment, and complications associated with liver biopsy can limit screening for hepatitis C. However, the accuracy of HCV RNA testing, the availability of medication assistance programs for uninsured patients, and improved treatments with fewer side effects and shorter duration should allay some of the anxiety associated with the screening process.
Does The Referral For Follow

The law does not specify the clinician specialty but does specify that the referral must be for follow-up hepatitis C care. The patientâs medical record should reflect the name of the provider/facility to whom the referral appointment was made. The Departmentâs website includes contact information for providers of hepatitis C care and treatment.
You May Like: Is Hpv Vaccine Same As Hepatitis B
Who Should Be Tested For Hepatitis C
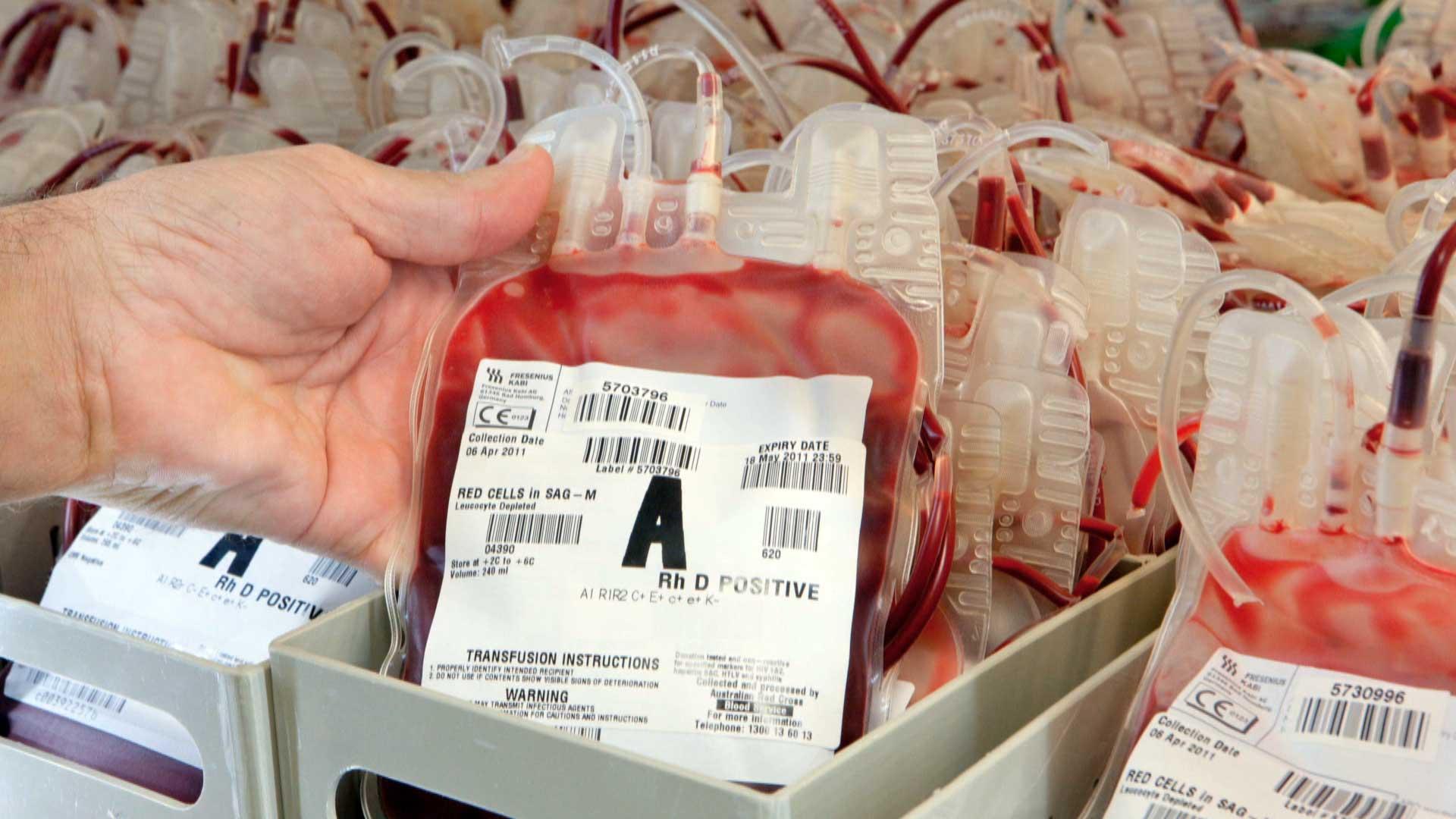
The CDC recommends that all baby boomers be tested once for hepatitis C even if no other risk factors are present. Additionally, the CDC recommends testing for anyone that is currently injecting drugs, has ever injected drugs, was the recipient of blood or organ transfers from an infected person, or has been in an environment which he or she was at in increased risk for exposure.
Why Did Screening Recommendations Change
A lot of it has to do with the treatment for hep C itself. Only a decade ago, treatment options for the disease werent that effective and caused significant side effects. Now, with the development of medications called direct-acting antiviral regimens, treatments for hep C destroy the virus in more than nine out of 10 people. These meds are also easier to tolerate and typically require only 8 to 12 weeks of therapy. Thats been a really remarkable change, Dr. Chou says.
Don’t Miss: What Is The Treatment For Hepatitis B Virus
Hepatitis C Testing Strategy
The goal of hepatitis C screening is to identify persons who are currently infected with HCV. Hepatitis C testing should be initiated with a U.S. Food and Drug Administration -approved anti-HCV test. Persons who test anti-HCV positive are either currently infected or had past infection that has resolved naturally or with treatment. Immunocompetent persons without hepatitis C risks who test anti-HCV negative are not infected and require no further testing. Persons testing anti-HCV positive should have follow-up testing with an FDA-approved nucleic acid test for detection of HCV RNA. NAT for HCV RNA detection determines viremia and current HCV infection. Persons who test anti-HCV positive but HCV RNA negative do not have current HCV infection. CDC encourages use of reflex HCV RNA testing, in which specimens testing anti-HCV positive undergo HCV RNA testing immediately and automatically in the laboratory, using the same sample from which the anti-HCV test was conducted. Hepatitis C testing should be provided on-site when feasible.
Hepatitis C Testing Types
Testing for hep C starts off with a hep C antibody test. This test looks for human antibodies something that your body produces to fight the virus. If your hep C antibody test result is positive, then it means you have been exposed to the hep C virus at some point.
If you get a positive antibody result, then your sample of blood is tested again using a PCR test. This test looks for parts of the actual hep C virus. If the PCR test result is positive it means that you have hep C. Have a look at our Hep C Testing chart for more info on hep C tests.
Recommended Reading: Can You Drink Alcohol With Hepatitis C
Under The New Law Do All Patients At
Under the new law, only those patients born between 1945 and 1965 are required to be offered a hepatitis C screening test. Although the new law requires the offer of a test only for those born between 1945 and 1965, CDC recommends hepatitis C testing be offered to all persons at risk for hepatitis C, such as injection drug users, those that received a blood transfusion or organ donation before 1992, persons living with HIV, anyone with abnormal liver tests, health and safety workers who have been exposed to blood on the job and persons on long term dialysis.
What Is The Benefit Of Testing Someone For Hepatitis C
There are several reasons why someone should be tested for hepatitis C. Knowing one’s hepatitis C status will help prevent hepatitis C transmission to others. Early clinical evaluation and ongoing disease monitoring can also improve health outcomes. Additional measures can be taken to protect the liver from further harm such as getting vaccinated for hepatitis A and B, decreasing or eliminating alcohol consumption and understanding the interactions among herbal supplements, over the counter medications, and prescription medications. Finally, hepatitis C is a curable disease for most. Better and more effective treatments are now available. The earlier in the disease process someone receives treatment, the greater chance they have to be cured.
Recommended Reading: Vaccine Available For Hepatitis B
Who Should Get Tested
You should consider getting tested for hepatitis C if you’re worried you could have been infected or you fall into one of the groups at an increased risk of being infected.
Hepatitis C often has no symptoms, so you may still be infected if you feel healthy.
Some groups of people are at an increased risk of hepatitis C, including:
- ex-drug users and current drug users, particularly users of injected drugs
- people who received blood transfusions before September 1991 or blood products before 1986 in the UK
- UK recipients of organ or tissue transplants before 1992
- people who have lived or had medical treatment in an area where hepatitis C is common high-risk areas include Africa, the Middle East and central Asia
- babies and children whose mothers have hepatitis C
- anyone accidentally exposed to the virus, such as health workers
- people who have received a tattoo or piercing where equipment may not have been properly sterilised
- sexual partners, family members and close contacts of people with hepatitis C
If you continue to engage in high-risk activities, such as injecting drugs frequently, regular testing may be recommended. Your doctor will be able to advise you about this.
How Do You Treat Hepatitis
Oral medications are taken to help treat the hepatitis C virus. They work in people with early and late stages of the disease. These medications also have few side effects.
“Prior to 2014, treatment for hepatitis C was intense and worked only half the time. Now, you can take one pill a day for eight to 12 weeks to get rid of the virus from your blood and eliminate the disease,” says Wolf. “Its literally a cure.”
If you are a baby boomer, ask your doctor about getting the one-time hepatitis C screening test. And, if you’re concerned about people in your life who are baby boomers, be sure to share this information with them, too. Spread the word on Facebook!
You May Like: What Hepatitis Is Not Curable
How Is Hcv Transmitted
All persons with HCV-RNA in their blood are considered infectious. The highest infection rates occur in persons with large or repeated, direct percutaneous exposure to blood or blood products, including:
- Less than 10 percent of cases are sexually transmitted.
- Perinatal transmission accounts for 5 percent of cases.
Summary Of The Literature
For the all-adult review, the initial literature search yielded 4,867 studies. Twenty-nine duplicates were identified. Of 4,838 unique studies, 4,170 were deemed irrelevant by title/abstract screening, resulting in 668 full texts for review. Among these, 368 studies had data available to extract.
For the pregnancy review, the initial literature search yielded 1,500 studies. Two duplicates were identified. Of 1,498 unique studies, 1,412 were deemed irrelevant by title/abstract screening, resulting in 86 full texts for review.
The supplementary review yielded an additional 1,038 and 195 studies among all adults and pregnant women, respectively. Of these, 912 and 168 , respectively, were deemed irrelevant by title/abstract screening, resulting in 126 and 27 , respectively, full texts for review. One study was added to the pregnant women review outside of the formal literature search .
Considering all 104 applicable studies, the median anti-HCV positivity prevalence among all adults was 6.6% . Median anti-HCV positivity prevalence was 1.7% for the general population , 7.5% for ED patients , 3.3% for birth cohort members , 9.3% for others/multiple risk factors , 54.2% for persons who use drugs , 5.2% for persons with HIV or sexual risk , and 4.7% for immigrants . Considering 26 applicable studies among pregnant women, median anti-HCV positivity prevalence was 1.2% .
Don’t Miss: What Is The Meaning Of Hepatitis
Appropriate Uses Of The Hcv Rna Test
There are 4 major reasons that HCV RNA tests are used:
More rarely, HCV RNA is used when either very acute HCV infection is suspected or a false HCV Ab is suspected.
It would not be appropriate to repeatedly order HCV RNA viral load screening for a patient who is not on or was recently on HCV treatment, or to use the HCV viral load to determine the severity of the patient’s infection or the patient’s risk of developing significant liver disease.
Virus Description And Transmission
HCV is a small, single-stranded, enveloped RNA virus in the flavivirus family with a high degree of genetic heterogeneity. Seven distinct HCV genotypes have been identified. Genotype 1 is the most prevalent genotype in the United States and worldwide, accounting for approximately 75% and 46% of cases, respectively . Geographic differences in global genotype distribution are important because some treatment options are genotype specific . High rates of mutation in the HCV RNA genome are believed to play a role in the pathogens ability to evade the immune system . Prior infection with HCV does not protect against subsequent infection with the same or different genotypes.
HCV is primarily transmitted through direct percutaneous exposure to blood. Mucous membrane exposures to blood also can result in transmission, although this route is less efficient. HCV can be detected in saliva, semen, breast milk, and other body fluids, although these body fluids are not believed to be efficient vehicles of transmission .
Also Check: How To Know If You Have Hepatitis B
Taking A Hepatitis C Test
Hepatitis C testing is conducted on a sample of blood. Blood samples can be collected by a doctor, nurse, technician, or other health care provider from an adult patients vein using a small needle or a skin prick on a childs heel.
For an at-home hepatitis C test, patients collect a blood sample according to the manufacturers directions. Instructions provided in the test kit detail the steps to obtain a small sample of blood and mail it for testing.
What Are The Key Provisions Of The Law
- A hepatitis C screening test must be offered to every individual born between 1945 and 1965 receiving health services as an inpatient or a hospital, or receiving primary care services in the outpatient department of hospital, or in a freestanding diagnostic and treatment center or from a physician, physician assistant, or nurse practitioner providing primary care.
- If an individual accepts the offer of the hepatitis C screening test and the screening test is reactive, the health care provider must offer the individual follow-up health care or refer the individual to a health care provider who can provide follow-up health care. The follow-up health care must include a hepatitis C diagnostic test.
- The offer of testing must be culturally and linguistically appropriate.
Also Check: Is Hiv The Cause Of Hepatitis B
Are There Other Reasons For The New Recs
Yes. A big reason for the re-think is that the number of hep C cases has risen dramatically in recent years, in part due to the opioid epidemic. Public health experts estimate that about one in three people who inject drugs under the age of 30 are infected with hep C, while the majority of older injection drug users are also likely to be infected. These factors convinced infectious disease experts that screening should be widespread and reach a broad age demographic.
If Using The General Medical Consent Does The Hepatitis C Screening Test Have To Be Specifically Listed In The Consent Language
No. The hepatitis C screening test does not specifically need to be identified in the consent language. However, we do recommend that the patient receives some type of education on hepatitis C, including the rationale for the screening test. The educational information can be provided in many different formats, including a fact sheet, brochure or a poster.
Read Also: Colloidal Silver And Hepatitis C
When Should I Get Hepatitis C Testing
When used for early detection in patients without symptoms of hepatitis C, screening is recommended at least once for all adults aged 18 years or older, except in locations with very low prevalence of HCV. Screening is also recommended during pregnancy and for patients of any age with risk factors for HCV infection. In patients with risk factors, periodic screening is recommended for as long as risk factors persist.
Risk factors for HCV include:
- Current or past injectable drug use
- Having a blood transfusion or organ transplant before July 1992
- Receiving kidney dialysis
- Pain in the abdomen or joints
- Nausea, vomiting, or loss of appetite
- Jaundice or yellowish skin and eyes
Hepatitis C testing may also be performed when liver tests are abnormal or when diagnosing the cause of existing liver damage.
Does The Requirement That Hepatitis C Testing Be Offered To All Persons Born Between 1945 And 1965 Apply In All Medical Settings
The requirement for the offering of testing applies to:
- Persons receiving inpatient services at hospitals
- Persons receiving primary care services through hospital outpatient clinics and diagnostic and treatment centers and
- Persons receiving primary care services from physicians, physician assistants, and nurse practitioners regardless of setting.
Emergency Departments are not required by the law to offer hepatitis C screening testing, but are encouraged to do so.
Don’t Miss: What Are The First Signs Of Hepatitis C
What Do We Do If A Patient Does Not Have Health Insurance And Accepts The Offer Of The Hepatitis C Screening Test
There are a number of free hepatitis C test sites throughout the state. For a complete list of those sites, go to:
- or
Free hepatitis C rapid test kits are also available for providers through the NYSDOH Hepatitis C Rapid Testing Program. Providers wishing to provide hepatitis C rapid testing may be eligible to enroll in this program. These tests kits are available for use with persons that do not have health insurance coverage. For more information on the NYS Hepatitis C Rapid Testing Program, go to: or call 518-486-6806.
What Are The Exceptions To The Mandatory Offer Of Hepatitis C Testing In The Hospital Diagnostic And Treatment Center And Primary Care Settings Noted In The Law
The law does not require an offer of testing to be made:
- When the individual is being treated for a life-threatening emergency.
- When the individual has previously been offered or has been the subject of a hepatitis C related test .
- When the individual lacks the capacity to consent* .
*The exception as stated in the law refers to the individual lacking the capacity to accept the offer. The reference to “capacity to consent” does not imply written, informed consent for the hepatitis C test, but rather capacity to understand the test offer.
You May Like: Can Chronic Hepatitis B Be Cured
Hepatitis C And Health
How can health-care personnel avoid exposure to HCV?
Avoiding occupational exposure to blood is the primary way to prevent transmission of bloodborne illnesses among health-care personnel. To promote blood safety in the workplace, health-care personnel should consult infectious-disease control guidance from the National Institute for Occupational Safety and Health and from CDC. Depending on the medical procedure involved, Standard Precautions may include the appropriate use of personal protective equipment .
What is the risk of acquiring hepatitis C after being accidentally exposed to HCV-contaminated blood or body fluids in the workplace?
Although sharps injuries have decreased in recent decades due to improved prevention measures, they continue to occur, placing health-care personnel at risk for several bloodborne pathogens like hepatitis C. A recent analysis of several studies revealed an overall 0.2% risk for infection among those exposed to HCV-antibody-positive blood through needlestick or sharps injuries . Updated guidelines for management and treatment of hepatitis Cexternal icon are available to provide guidance for health-care personnel who become infected via exposure to contaminated blood at the workplace.
Other than needlesticks, do other exposures place health-care personnel at risk for hepatitis C?
Should HCV-infected health-care personnel be restricted in their work?