When Can Hepatitis B Patients Stop Taking Antivirals Experts Finally Have Some Answers
With the help of antivirals, many patients today have undetectable viral load , a relatively healthy liver and cleared the hepatitis B e antigen . So when can they consider stopping their daily entecavir or tenofovir pill?
For years, experts have admitted the endgame of antiviral treatment has been ill-defined. While antivirals reduce viral load and the risk of liver damage, they rarely cure people. Recently, after years of observing patients and with the help of better diagnostic tools, experts are getting better at identifying when might be safe to stop.
Historically, in addition to reducing viral load to undetectable levels, the goals of antiviral treatment were:
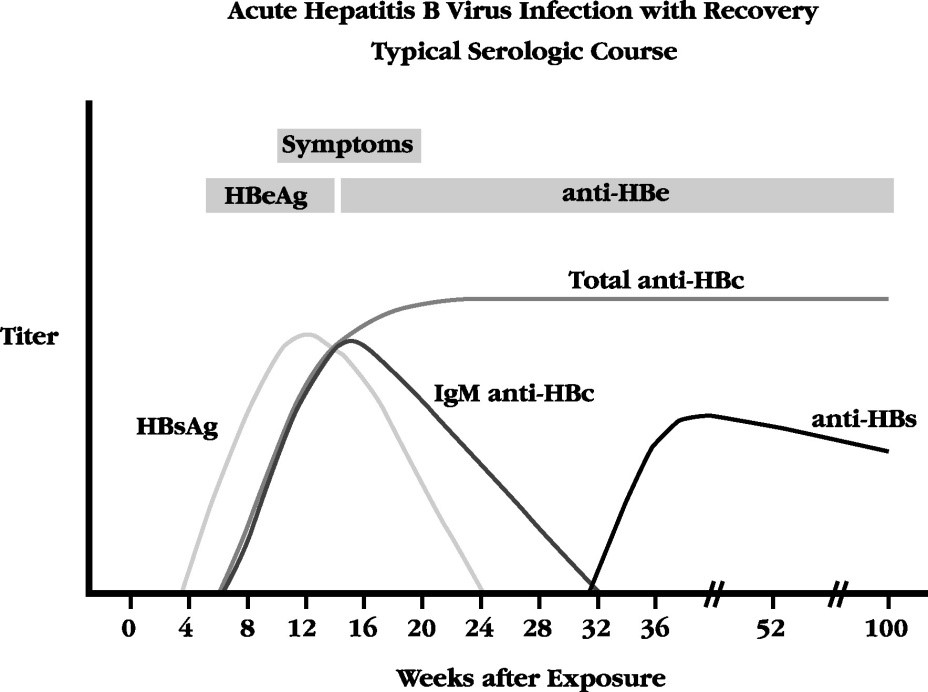
- Triggering HBeAg seroconversion: About 21 percent of HBeAg-positive patients with liver damage treated with either tenofovir or entecavir for 12 months are able to lose the hepatitis B e antigen and develop the e antibody . This HBeAg seroconversion indicates the immune system is fighting the infection and slowing viral replication.
- And reducing liver damage and even clearing the hepatitis B surface antigen : About 1-3 percent of patients treated with antivirals lose HBsAg after years of treatment. This is called a functional cure. Unfortunately, if you have HBeAg-negative hepatitis B, only 1-2 percent of you will lose HBsAg after five to eight years of antiviral treatment.*
What Are The Risk Factors For Getting Hepatitis B
Due to the way that hepatitis B spreads, people most at risk for getting infected include:
- Children whose mothers have been infected with hepatitis B.
- Children who have been adopted from countries with high rates of hepatitis B infection.
- People who have unprotected sex and/or have been diagnosed with a sexually transmitted infection.
- People who live with or work in an institutional setting, such as prisons or group homes.
- Healthcare providers and first responders.
- People who share needles or syringes.
- People who live in close quarters with a person with chronic hepatitis B infection.
- People who are on dialysis.
Current Therapy For Chronic Hbv
Current therapy for CHB includes interferon or PEGylated IFN-α , and/or nucleoside/nucleotide -based therapy, which includes lamivudine , adefovir, telbivudine, entecavir and tenofovir. The patients with CHB are at increased risk of progression to cirrhosis and hepatocellular carcinoma . CHB is responsible for approximately 600,000 deaths owing to its complications . The main goal for current HBV therapy is to alter the progression of liver fibrosis and reduce the occurrence of HCC.
Long-term follow-up studies have shown that treatment with PEG-IFN with or without 3TC results in a prolonged clinical remission with durable viral suppression in hepatitis B envelope antigen -positive CHB patients, increased rate of hepatitis B surface antigen seroconversion and improved liver histology . Response rate was also higher in genotypes A or B compared with C or D and with lower levels of HBV DNA at baseline and higher levels of ALT . Use of PEG-IFN therapy is limited by intolerance and adverse events.
The oral antiviral drugs, initially approved in USA were well tolerated but efficacy of these agents is limited by emergence of antiviral resistance. However, newer agents are more potent, well tolerated, and have a high barrier to antiviral resistance. Long-term follow-up studies on newer agents has shown sustained viral suppression along with improvement in biochemical and histologic evidence of disease .
You May Like: How Hepatitis C Affects The Body
Emergency Hepatitis B Treatment
See your GP as soon as possible if you think you may have been exposed to the hepatitis B virus.
To help stop you becoming infected, they can give you:
- a dose of the hepatitis B vaccine you’ll also need 2 further doses over the next few months to give you long-term protection
- hepatitis B immunoglobulin a preparation of antibodies that work against the hepatitis B virus and can offer immediate but short-term protection until the vaccine starts to take effect
These are most effective if given within 48 hours after possible exposure to hepatitis B, but you can still have them up to a week after exposure.
How Common Is Hepatitis B
Hepatitis B is fairly common in Africa and the western Pacific region. Throughout the world, there are about 292 million people who are infected with chronic hepatitis B. In the U.S., the figure exceeds 2 million people.
The number of infections had been falling in the U.S., but fewer vaccinations among adults combined with the onset of the opioid crisis and injected drug usage has resulted in the numbers rising again. Infected women can pass the infection on to their babies. Children who are infected before age 5 are more likely to have chronic infection than those infected later in life.
Read Also: Is There A Cure For Hepatitis B Virus
Strategies To Improve The Efficacy Of Ifn
Given the unique advantages of but relatively low response rates to IFN therapy, there is an urgent need to improve its efficacy .
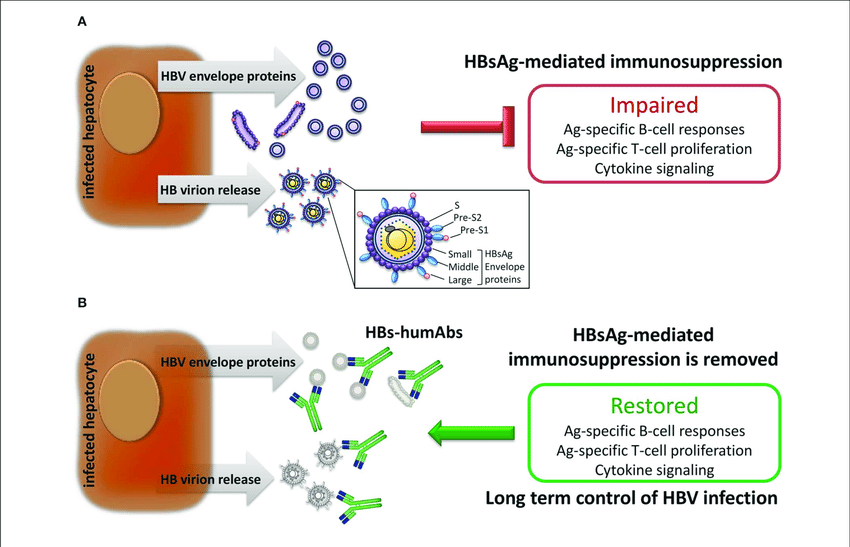
Figure 1 Predictors and strategies for improvement of the efficacy of IFN-based therapy for chronic hepatitis B.
In addition to type I IFN, type III IFNs, consisting of four IFN- subtypes , has been considered as an alternative in treatment of CHB . IFN-III signals through a heterodimeric receptor composed of IFN- receptor-1 and interleukin-10 receptor subunit beta . IFNLR1 is expressed primarily on epithelial cells, such as hepatocytes, and on select immune cells, including pDCs and some B-lymphocytes, which may indicate better cell-type specific activity . One of the most impactful findings about IFN- is the strong association of IFN- polymorphisms with chronic HCV clearance during the acute stage of infection and of achieving HCV cure with IFN-I-based therapy in chronic infection . Unfortunately, the similar association cannot be identified in HBV patients with high confidence and good reproducibility among various studies . Although IFN- can activate IFN signaling pathways and lower HBV viral load, pegylated IFN-1 was less efficient than PEG-IFN-2 24 weeks post-treatment because fewer patients achieved HBeAg seroconversion .
Value Of Biopsy: Fibrosis And Necro
Patients with moderate/severe inflammation or bridging fibrosis/cirrhosis must be treated. The degree of fibrosis or inflammation upon liver biopsy cannot be predicted for HBV-DNA levels > 10000 copies/mL. ALT is an imperfect marker for liver disease . Traditional and current guidelines recommend liver biopsy for patients who meet the criteria for chronic hepatitis . These patients must be treated if we follow the guidelines, and we believe that liver biopsy may be unnecessary.
Liver biopsy is more important for patients who do not meet the current criteria for treatment but have serum HBV-DNA levels of 104 to 105 copies/mL and/or ALT/AST levels that are normal or mildly elevated . The presence of significant inflammation or bridging fibrosis/cirrhosis is an indication for treatment. In a subgroup of these patients, hepatic elastography can avoid the need to carry out a liver biopsy for detection of significant fibrosis. This is a novel non-invasive method to assess hepatic fibrosis in patients with a chronic disease, by measuring liver stiffness. Its failure rate is about 5% of cases, mainly in obese patients. Elastography has a high positive predictive value for diagnosing significant fibrosis in Asian CHB patients. This method does not have a defined role in HBeAg-negative patients because histological inflammation during reactivation may affect the results.
Read Also: Medicine That Cures Hepatitis C
Why Wont Doctors Treat Young Adults With High Viral Load And No Signs Of Liver Damage
If antiviral medications almost always lower viral loads, why dont doctors treat young adults with high viral loads with this daily pill? After all, dont high viral loads lead to liver damage and even liver cancer?
This is one of the most common questions posed to the Hepatitis B Foundation, and at first glance the decision not to treat a high viral load with antivirals seems counter-intuitive or plain wrong. If antivirals reduce the number of hepatitis B virus in the body, wont that give the immune system an opportunity to clear out the remaining residual HBV?
Unfortunately, it doesnt work that way. Its complicated, as are many aspect of hepatitis B.
Its common for young adults who live with hepatitis B to be in the immune tolerant stage of infection with extremely high viral load but with no signs of liver damage.
When were born to mothers infected with hepatitis B, unless were immunized at birth 90 percent of us become infected from exposure to infectious blood and body fluids during delivery. And when infants are infected, their immature immune systems dont recognize the virus. The young immune system misses the red flag signature on this hepatitis B virus and tolerates the infection instead of attacking it.
Experts recently re-examined whether this hands-off approach was still valid and reviewed more than a dozen studies that examined whether antiviral treatment benefited immune-tolerant adults.
Lets explore their rationale:
Factors That Influence Ifn Response
HBV has been called a stealth virus since it does not induce a significant IFN response in the liver. Besides, sustained off-treatment response to exogenous IFN- therapy can be achieved only in a minority of CHB patients. Both host and viral factors influence the IFN response during HBV infection and IFN- therapy , some of which could be used as predictors to improve the cost-effectiveness of IFN- therapy.
Table 1 Viral and host factors that affect IFN response during HBV infection and IFN therapy.
Don’t Miss: Can You Get Hepatitis A After Vaccination
How Is Hepatitis B Prevented
Testing & Vaccination
- The hepatitis B vaccine offers excellent protection against HBV. The vaccine is safe and highly effective. Vaccination consists of 3 doses of vaccine over the course of 6 months. Protection lasts for 20 years to life.
- The American Academy of Pediatrics recommends that all children should receive hepatitis B vaccine starting at birth. .
- The CDC recommends hepatitis B vaccine for persons traveling to countries where HBV is common .
- If you have one or more risk factors for hepatitis B infection, you should get a simple HBV blood test. The blood test will determine whether you are:
- immune to hepatitis B or
- susceptible to hepatitis B and need vaccination or
- infected with hepatitis B and need further evaluation by a physician
Perinatal Hepatitis
- California law requires testing of all pregnant women for hepatitis B infection
- If the mother is HBV-infected, she will pass the infection to the baby during the birth process, unless the baby gets immunized within hours of birth
- Giving the infant HBIG and HBV vaccine right away will reliably prevent infection of the infant
- Other family members should best tested for hepatitis B too, and given vaccine if they are not already infected or immune
Healthy Habits
After Exposure to Hepatitis B
What Should You Know About Pregnancy And Hepatitis B
A pregnant woman who has hepatitis B can pass the infection to her baby at delivery. This is true for both vaginal and cesarean deliveries.
You should ask your healthcare provider to test you for hepatitis B when you find out you are pregnant. However, while it is important for you and your healthcare provider to know if you do have hepatitis B, the condition should not affect the way that your pregnancy progresses.
If you do test positive, your provider may suggest that you contact another healthcare provider, a liver doctor, who is skilled in managing people with hepatitis B infections. You may have a high viral load and may need treatment during the last 3 months of your pregnancy. A viral load is the term for how much of the infection you have inside of you.
You can prevent your infant from getting hepatitis B infection by making sure that your baby gets the hepatitis B vaccine in the hours after they are born along with the hepatitis B immunoglobulin. These two shots are given in two different locations on the baby. They are the first shots needed.
Depending on the type of vaccine used, two or three more doses must be given, usually when the baby is 1 month old and then 6 months old, with the last by the time the baby is 1 year old. It is critical that all newborns get the hepatitis B vaccination, but even more important if you have hepatitis B yourself.
Read Also: What’s The Difference Between Hepatitis B And Hepatitis C
Causes And Risk Factors
Hepatitis B is caused by a viral infection. The virus can survive outside of the body for at least seven days. During this time, it can infect a person if it enters his or her body. It can be detected within 30 to 60 days after infection. It can persist and develop into chronic hepatitis B, especially if someone is infected at a young age.
It can be transmitted or spread in several ways, including :
Anyone can get this virus. But some people are at a greater risk of exposure to the virus. This includes people who:
- Have multiple sexual partners
- Travel to countries with a high hepatitis B rate
Management Of Pregnant Hbv Carriers
Pregnant HBV carrier mothers present a unique opportunity to prevent transmission of HBV to their neonates. All infants born to HBsAg-positive mothers should receive hepatitis B immune globulin and a full course of HBV vaccination . Vaccine failure in the neonate is rare but does occur , and may be accounted for by transplacental transmission before birth. Follow-up testing of the neonate should be performed to confirm vaccination effectiveness. Testing should be performed for HBsAg to detect vaccine failures, anti-HBs to confirm a successful vaccine response and anti-HBc-Total to determine if the anti-HBs response was due to vaccination or resolution of natural infection. While testing for these markers is recommended one to two months after completion of the vaccine series, testing at approximately 18 months would ensure that the anti-HBc-Total test does not represent maternal antibody. This may be important because vaccination failures have occasionally been associated with HBV vaccine escape mutants that may only demonstrate a positive anti-HBc-Total as the sole marker of infection. These mutations occur in the open reading frame of the HBsAg, may not be recognized by antibodies induced by current HBV vaccine, and may not be detected by currently available HBsAg enzyme immunoassays . Clearly, surveillance systems need to be in place to ensure that HBV vaccines remain effective and vaccine escape mutants do not replace current HBV strains.
Don’t Miss: What Are The Symptoms Of Having Hepatitis C
What Treatments Are Available For Chronic Hepatitis B If Medications Dont Work
If you have advanced hepatitis B, you might also become a candidate for a liver transplant. This path does not always result in a cure because the virus continues in your bloodstream after a transplant. To prevent being infected again after your transplant, you may be prescribed hepatitis B immunoglobulin with an antiviral agent.
Vaccination And Other Prevention Measures
Vaccination is a safe and effective way of preventing the spread of hepatitis B. Since 1985, the hepatitis B vaccine has been part of the national immunisation schedule. In 1988, New Zealand was one of the first countries to introduce universal infant hepatitis B immunisation.The vaccine is given to babies at age six weeks, three months, and five months. Babies born to mothers with hepatitis B receive an extra dose of the vaccine at birth as well as a dose of hepatitis B-specific immune globulin.In children and adolescents who did not receive the hepatitis B vaccine in the first year of life, the full three-dose course is recommended.Hepatitis B immunisation is recommended and publicly funded for all infants and children up to their 18th birthday, household and sexual contacts of people with acute or chronic hepatitis B, and certain other high-risk populations. Measures that can help prevent the spread of the hepatitis B virus include:
- Teaching children not to touch the blood or wounds of others
- Covering cuts, scratches, and grazes
- Not sharing personal items such as razors and toothbrushes
- Never sharing needles or syringes if you use intravenous drugs
- Practising safe sex, including the use of condoms
- Seek assurance that body piercing and tattooing needles and equipment are sterile.
Recommended Reading: What Are The First Symptoms Of Hepatitis C
Who Should Be Vaccinated For Hepatitis B
All newborns should be vaccinated. Also, people who are under 18 who were not vaccinated at birth should also get the vaccine. Other groups who should be sure to be vaccinated are those in certain high-risk categories, such as:
- People who have more than one sexual partner.
- Men who have sex with men.
- Adults with diabetes.
- Sexual partners of infected people and people who share households with infected individuals.
- People who are exposed to blood and other bodily fluids, including healthcare and public safety professionals, and people who work in jails and other places taking care of people who cant take care of themselves.
Hepatitis B For Health Professionals
The Hepatitis Foundation runs a national monitoring programme for people living with chronic hepatitis B . Approximately 25,000 individuals are enrolled. People infected with chronic hepatitis B are at risk of liver failure and liver cancer. Long-term regular blood test monitoring has been shown to reduce morbidity and mortality from CHB.
GPs can refer patients to us via phone, by printing and completing a referral form and returning it to us via post, fax or email , or electronically via CareSelect, HealthLink , Best Practice or Medtech Outbox.
You May Like: What Does Hepatitis C Cause
Detection Of Antiviral Resistance
Lamivudine monotherapy has been reported to be associated with the rapid emergence of antiviral resistance in 15% to 60% of treated individuals . Resistant HBV genomes have mutations in codon 552 within the YMDD motif of the reverse transcriptase/polymerase where a valine or isoleucine replaces the methionine. Resistance is typically clinically manifested by significant elevations in ALT after an initial decline in response to treatment. Prolonged treatment after development of the YMDD mutant is controversial, although improvement in liver pathology with decreased fibrosis may occur with continuation of treatment. Concerns about disease flares after stopping lamivudine have been raised . The development of genotypic resistance can be documented by molecular sequencing or by the INNO-LiPA HBV DR assay , which involves hybridization of amplified HBV-DNA fragments onto specific nucleotide probes that have been immobilized on nitrocellulose strips .