How Can A Person Get Hepatitis C
Hepatitis C transmits from person to person, most often through shared needles, so its particularly prevalent among intravenous substance users. Even absent needle sharing, it can also be transferred through all equipment used to prepare or cook intravenous drug solutions, putting all those in contact with these instruments at high risk.
How Alcohol And Hepatitis C Affect The Liver
Alcohol is toxic to the liver. This is true for all people, even those who don’t have hepatitis C. But, if you do have the virus, the damage from alcohol is even greater. Learning what your liver does can help you understand why.
Your liver has many jobs. First, it works as a metabolic factory. The liver takes certain substances in your bloodstream, like sugars and proteins, and turns them into other things your body needs. The liver stores essential nutrients and releases them when your body needs them.
The liver also acts like a filter. Blood passes through the liver. As this happens, it breaks down alcohol and other harmful chemicals and cleans your blood.
However, if you have hepatitis C, your liver can’t do these jobs as well. The virus makes it hard for the liver to break down alcohol. This means the toxins in alcohol are not completely removed from your body.
Normally, the liver can repair itself if it’s damaged by infection or injury. But if it’s constantly under attack from a virus, drugs or alcohol, scar tissue can develop, replacing healthy liver tissue. This damage is more difficult to repair. Over time, this can lead to severe permanent scarring of the liver. That’s a serious health condition called .
The bottom line: Both hepatitis C and alcohol damage the liver. If you have this and you drink alcohol, your chances of developing cirrhosis are much greater.
What Are The Other Health Challenges For People With Hepatitis Who Inject Drugs
People with hepatitis who inject drugs often have several other health conditions at the same time, including mental illness and HIV/AIDS, thus requiring care from multiple health care providers. This is sometimes referred to as co-occurring disorders. Substance use disorder treatment is critical for PWID, as it can reduce risky behaviors that increase the chance of transmitting hepatitis. Research has shown that patients with hepatitis receiving medication-assisted treatment for their opioid addiction can be safely treated with antiviral medications.5
To enhance HCV care, NIDA is examining coordinated care models that utilize case managers to integrate HCV specialty care with primary care, substance use disorder treatment, and mental health services so that these patients get treatment regimens that address all of their health care needs. The Health Resources and Services Administrations Ryan White HIV/AIDS Program developed a free, online curriculum about HIV/hepatitis C for healthcare providers and healthcare staff to increase knowledge about co-infection among people of color in the United States.
Also Check: Side Effects Of Hepatitis C Medication
Role Of Ros In Hcv And Ald
The generation of ROS seems to be a hallmark of both ALD and HCV .3). While location and mechanisms of their generation differ markedly between ALD and HCV, downstream events of oxidative damage are similar due to the high but rather unspecific reactivity of species such as hydroxyl radicals or lipid peroxidation products. Hepatocyte mitochondria are structurally altered in more than 50% of HCV patients and these conditions are accompanied by a significant depletion of hepatocellular and lymphocyte glutathione , an increase of oxidized GSH and the lipid peroxidation marker malondialdehyde. ROS are either induced directly by the virus or indirectly through activation of inflammatory cells. HCV core and NS5A have been implicated in generating ROS via mitochondrial damage and calcium release.
Potential molecular mechanisms that explain the synergistic effect of alcohol and HCV on the progression of liver disease. Reactive oxygen species and iron accumulation seem to be key features of both diseases.
Charles S Lieber Md Macp
Charles S. Lieber, M.D., M.A.C.P., is chief of the Section of Liver Disease & Nutrition, Alcohol Research Center, Bronx, NY Medical Center and professor of medicine and pathology at Mt. Sinai School of Medicine, New York, New York. The preparation of this article was supported in part by National Institute on Alcohol Abuse and Alcoholism grants AA11115 and AA12867, by the Department of Veterans Affairs, and by the Kingsbridge Research Foundation.
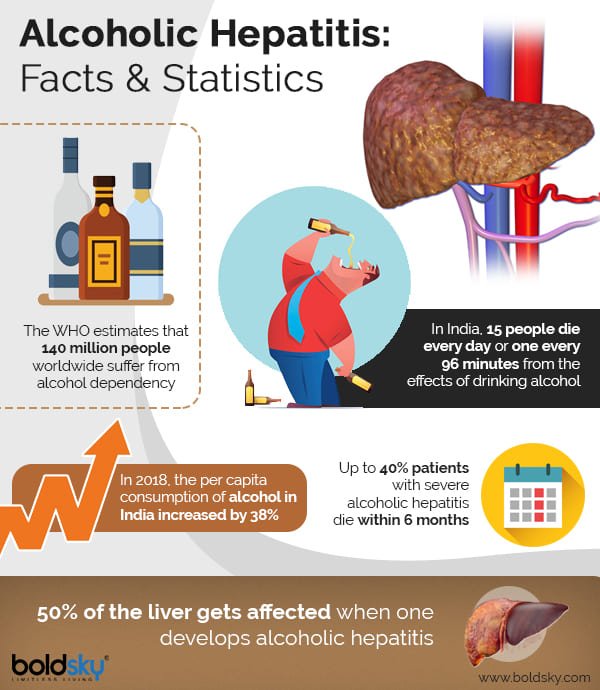
Hepatitis is an inflammation of the liver that is characterized by jaundice, liver enlargement, abdominal and gastric discomfort, abnormal liver function, and other symptoms. Although in many patients the diseased liver is able to regenerate its tissue and retain its function, severe hepatitis may progress to scarring of the liver tissue , cirrhosis, liver cancer , and chronic liver dysfunction. Hepatitis can have numerous causes, such as excessive alcohol consumption or infection by certain bacteria or viruses. One common cause of hepatitis is infection with one of several types of viruses . With the development of new diagnostic tools, infections with the hepatitis C virus have received increasing attention in recent years. In the United States, the number of deaths caused by HCV is increasing and may approach or even surpass the number of deaths from AIDS in the next few years .
EPIDEMIOLOGY AND NATURAL HISTORY OF HCV INFECTION
EFFECT OF ALCOHOLISM ON HCV INFECTION
Effects of Alcoholism on HCV Acquisition and Persistence
You May Like: Chronic Hepatitis C Without Hepatic Coma
What Is The Relationship Between Drug Use And Viral Hepatitis
Drug and alcohol use places people at particular risk for contracting viral hepatitis. Engaging in risky sexual behavior that often accompanies drug use increases the risk of contracting HBV and, less frequently, HCV. People who inject drugs are at high risk for contracting HBV and HCV from shared needles and other drug preparation equipment, which exposes them to bodily fluids from other infected people. Because drug use often impairs judgement, PWID repeatedly engage in these unsafe behaviors, which can increase their risk of contracting viral hepatitis. One study reported that each person who injects drugs infected with HCV is likely to infect about 20 others, and that this rapid transmission of the disease occurs within the first 3 years of initial infection.4 Drug and alcohol use can also directly damage the liver, increasing risk for chronic liver disease and cancer among those infected with hepatitis. This underscores that early detection and treatment of hepatitis infections in PWID and other people who use drugs is paramount to protecting both the health of the person and that of the community.
Maintaining A Healthy Weight
You may not think that your weight has anything to do with the health of your liver, but being overweight is linked to a buildup of fat in the liver. This is called nonalcoholic fatty liver disease .
Having a fatty liver when you already have hepatitis C may increase your risk of getting cirrhosis. Certain medications used to treat hepatitis C may also not be as effective if youre overweight.
If youre overweight, following a healthy eating plan and exercising regularly can help you lose weight. The recommends that adults should do some moderate-intensity physical activity for at least 30 minutes at least five days of the week.
Some examples of moderate-intensity activities include:
- walking briskly
There are no specific diet and nutrition rules for people with hepatitis C. But eating a good, well-balanced diet can help you reach and maintain a healthy weight and reduce your risk of hepatitis C complications.
Here are some general guidelines for eating well with hepatitis C:
- Choose whole-grain cereals, breads, and grains.
- Eat plenty of fruits and vegetables in a variety of colors.
- Avoid processed foods containing trans fats.
- Go easy on fatty, sugary, or salty foods.
- Resist fad diets, and opt for a food plan that you can live with and follow for the long term.
- Stop eating when youre about 80 percent full. You may actually be fuller than you think you are.
- Boost your energy by eating small meals or snacks every three to four hours.
Read Also: Hepatitis B And C Can Be Spread By
Risk Of Hcc And Other Clinical Manifestations Of Liver Disease Complicated By Hcv Infection And Alcohol Consumption
Among 120 recruited patients, HCCs were detected in 55 patients by analysis of follow-up images: five in Group A, 10 in Group B, 26 in Group C, and 14 in Group D . The occurrence of HCC was found to be significantly higher in the HCV plus alcohol intake groups compared to HCV infection only . HCV-infected patients who consumed alcohol moderately to heavily had a 1.52.5-fold greater risk of HCC in contrast to alcohol-free HCV-infected patients. The higher prevalence of HCC in Group C than in Group D may be due to the non-homogeneous distribution of patients in these two groups. Similar non-homogeneous distribution of patients in Group B and Group A resulted in a higher occurrence rate of HCC in Group B, compared to Group A .
When the clinical manifestations of gastro-oesophageal varices, ascites and encephalopathy were analysed and compared in the alcohol and alcohol-free groups, we found a significantly higher occurrence of these clinical manifestations in Groups C and D, compared to Groups B and A . HCV-infected patients showed a higher risk of these clinically apparent liver diseases, in contrast to patients with alcoholic liver disease . The gastro-oesophageal variceal bleeding episodes were higher in Groups A, C and D compared to Group B . When endoscopic formation of varices graded from F1 to F3 was compared among all groups of patients, we found that the frequency of severe varices was much higher in the alcohol-intake groups than alcohol-free HCV-infected patients.
How Much Alcohol Is Safe
So far it is unclear how long a patient has to abstain from alcohol before the negative effects of alcohol abuse are reversed. It is for this reason that alcohol cessation should be explored as part of a treatment plan for people with chronic HCV infection, particularly those with diagnosed with compensated or decompensated cirrhosis.
Furthermore, patients who require peginterferon are recommended to abstain for at least six months before starting treatment and should be advised to abstain from further alcohol consumption for at least six months following completion of therapy.
Read Also: How Do You Know If You Have Hepatitis A
Role Of Alcohol And Hcv On Development Of Hcc
Various studies have shown that there is an increased risk of HCC in patients with HCV and alcohol abuse compared to either HCV or ALD alone. Since these studies vary considerably in their definition of alcohol abuse, Table is restricted to comparable studies that tried to identify the independent contribution of HCV and ALD to HCC development. It can be concluded from these data, that a daily uptake of > 80 g alcohol alone increases HCC risk 5-fold while the presence of HCV alone increases HCC 20-fold. A combination of both risk factors increases the risk for HCC development over 100-fold. Thus, HCV and alcohol act truly synergistic on HCC development.
Preventing Complications From Hepatitis C
Liver damage is a major concern for people with hepatitis C. Hepatitis C can cause inflammation or swelling of the liver.
- This inflammation can eventually lead to liver damage called cirrhosis. Cirrhosis is a condition where scar tissue replaces healthy liver tissue. A liver with too much scar tissue wont work properly.
Here are some things you can do to keep your liver healthy:
- Dont drink alcohol and avoid using recreational drugs.
- Reach and maintain a healthy weight.
- Exercise most days.
- Eat a low-fat, high-fiber diet full of fruit, vegetables, and whole grains. Limit trans fats and saturated fats.
- Talk with your doctor before taking vitamins or other supplements.
Also Check: How Can You Contact Hepatitis C
Effect Of Graded Doses Of Alcohol
Only four studies divided drinking subjects into moderate drinking and heavy drinking groups. The results are shown on table 3. The cut off for moderate and heavy drinking varied in the four studies. In one study, alcohol intake was divided into three categories: < 40 g/day, 4180 g/day, and > 80 g/day. HCV RNA levels were comparable for the two lower categories which were combined. In another study, moderate and heavy drinking were defined as < 50 g/day and > 50 g/day, respectively. In the third study, the categories were < 46 g/day and > 46 g/day, respectively. The fourth study divided the drinking groups into < 80 g/day and > 80 g/day. Within each study and for the combined analysis we performed pairwise comparisons of effects between the non-drinking subjects and the two drinking groups. In two studies, there was an increasing effect on viral titres with higher doses of alcohol. The third study showed the same effect for non-drinkers and moderate drinkers with a decreasing effect for heavy drinkers. The fourth study gave the same decreased effect for moderate and heavy drinkers. Basing our choice of model on the test for heterogeneity, there was no significant difference between non-drinkers and moderate drinkers , between non-drinkers and heavy drinkers , or between moderate drinkers and heavy drinkers . For this analysis the requisite data for study by Loguercio and colleagues was estimated from a graph as the actual values were not provided.
Table 3
How Much Alcohol Is Too Much
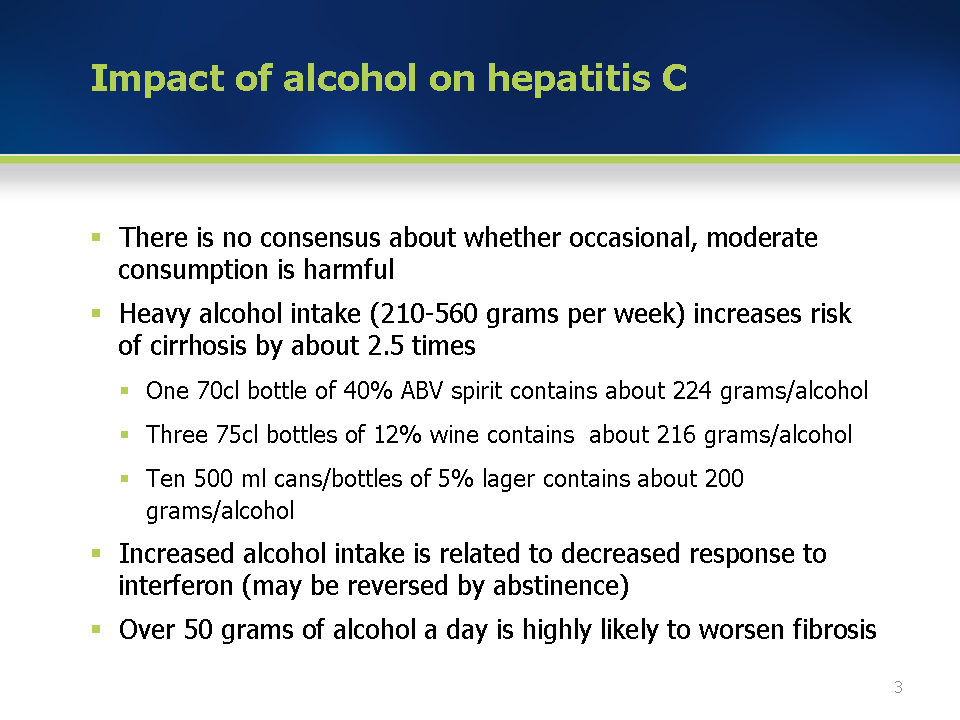
The more you drink, the worse the damage gets and the faster it happens. There’s no “safe” level of alcohol for people with C. The best thing you can do is avoid alcohol entirely.
People with hepatitis C who do not drink are much less likely to develop severe . This is true even up to 40 years after being infected with the virus. On the flip side, after 40 years of hepatitis C infection, most heavy drinkers have cirrhosis.
If you do drink, limit how much you have. If you have more than two alcoholic drinks daily or drink on most days of the week, take steps to cut back.
Don’t Miss: What Are The Symptoms Of Hepatitis A And B
Hcv Treatment Outcomes Among Persons With Alcohol Use
Most of the studies that have addressed whether alcohol use impacts treatment outcomes were performed in the pre-DAA treatment era and results from these studies were mixed.
DAA Treatment Era
- In the DAA treatment era, a large observational study out of the Veterans Affairs healthcare system evaluated the impact of alcohol use on HCV DAA-based treatment outcomes. Of the 15,151 persons who initiated DAA therapy and had a documented AUDIT-C score, 68.5% were categorized as abstinent, 22.6% as low-level drinking, and 8.9% as unhealthy drinking. Overall SVR12 rates were high among all persons in the study, regardless of alcohol use, with no statistical difference between HCV genotype or by cirrhosis status . These findings support current recommendations to not exclude persons from HCV treatment based on their alcohol use.
Interferon and Peginterferon Treatment Era
How Much Alcohol Can I Drink
Even modest alcohol consumption has been associated with increased oxidative stress and increased progression of fibrosis. A standard drink contains 12 grams of alcohol, which is equivalent to 1.5 ounces of whiskey or other 80 proof distilled spirits, a 12-ounce beer, or 5 ounces of wine. Since moderate alcohol consumption or about 2 standard drinks per day increases risk for progression of liver disease, you should try to avoid drinking altogether if you have HCV. This is especially true for the period before starting treatment with an interferon-based drug regimen.1
Recommended Reading: What Is Hepatitis B And C
Potential Reinfection With Hcv Among Persons Who Inject Drugs
Multiple studies have shown significant risk of HCV reinfection in persons cured with HCV therapy. Thus, it is essential that persons with past or active injection-drug use be counseled that they can become reinfected with HCV after achieving an SVR. This risk is significant in persons who inject drugs, but reinfection can also occur through sexual contact, particularly among men who have sex with men. In one study that clearly evaluated reinfection among treated PWID, the reinfection rate for those reporting ongoing injection after SVR was 5.3/100 person-years. Similarly, in a recent systematic review of 36 studies of HCV reinfection following successful HCV treatment in persons who inject drugs, the overall rate of HCV reinfection was 6.2 per 100 person-years among those who reported recent injection-drug use. In a pilot study among 31 persons with active injection-drug use treated with ledipasvir-sofosbuvir, the reinfection rate was 16.3/100 person-years . Thus, it is important that programs for HCV treatment provide access to counseling for safe injection practices and opioid agonist therapy. Although unstudied, detailed guidance on safer injection techniques may mitigate the risk for HCV infection .
Effect Of Alcohol On The Prevalence Of Hcv Infection
Chronic alcoholics have an increased prevalence of HCV infection, increasing with the severity of the ALD. Takase et al showed that HCV prevalence demonstrated by anti-HCV positivity increases with the severity of ALD, having a prevalence of approximately 5% in alcoholic fibrosis, almost 40% in alcoholic cirrhosis and almost in 80% in HCC due to alcohol. This could be due to the lifestyle of chronic alcoholics, since many of them are also intravenous drug abusers, which is a high risk for HCV infection. It could also be due to the immunosuppressive effect of alcohol decreasing the HCV-clearance rate after infection since it has been shown that alcohol suppresses the function of various immune components including natural killer cells, neutrophils, monocytes and others.
Don’t Miss: Chronic Hep C Without Hepatic Coma Icd 10
What Happens If Hepatitis C Virus Isnt Treated
When HCV care is not available, the condition can worsen into cirrhosis of the liver. This is a progressive, chronic hepatitis form that can ultimately render the liver unable to remove toxins from the bloodstream. It can also develop into a form of cancer called hepatocellular carcinoma. The CDC reports that one million people will die over the next 40 to 50 years due to chronic, untreated HCV infections.