Early Evidence On Hcv Transmission
HCV was first identified in 1989 and although studies as far back as 1993 pointed to sexual transmission as a probable risk factor amongst gay men, the information did not translate into a public health message. This is likely because many more studies showed that the risk of sexual transmission was seen to be extremely low in the general population, and there may also have been an assumption that safer sex messages relating to HIV would also implicitly cover HCV transmission.
In these earlier studies, published between 1993-1996, data on three different cohorts of gay men without a history of IDU in the U.S. showed that between 3-5 percent were infected with HCV. Osmond found that HCV infection was marginally associated with more than 50 sex partners a year or more than 25 oral receptive partners or more than 25 anal receptive partners. Buchbinder found that sexual risk factors for HCV infection included receptive anal intercourse, fisting, having a sexual partner with a history of IDU, a self-reported history of genital herpes and being HIV-positive. Ndimbie found that whilst the number of sexual partners was not a significant risk factor, a history of syphilis, rectal gonorrhoea, insertive anal intercourse with ejaculation, and douche or enema use before anal receptive intercourse were statistically significant sexual risk factors.
No Identifiable Source Of Infection
According to the Centers for Disease Control and Prevention, injection drug use accounts for approximately 60% of all HCV infections in the United States, while other known exposures account for 20-30%. Approximately 10% of patients in most epidemiological studies, however, have no identifiable source of infection. HCV exposure in these patients may be from a number of uncommon modes of transmission, including vertical transmission, and parenteral transmission from medical or dental procedures prior to the availability of HCV testing. There are no conclusive data to show that persons with a history of exposures such as intranasal cocaine use, tattooing or body piercing are at an increased risk for HCV infection based on these exposures solely. It is believed, however, that these are potential modes of HCV acquisition in the absence of adequate sterilization techniques.
What Is The Treatment For Hepatitis C
Drugs are licensed for treatment of persons with chronic hepatitis C. Combination drug therapy, using pegylated interferon and ribavirin, can get rid of the virus in up to five out of ten of persons with genotype 1, the most common genotype in the U.S. and eight out of ten persons with genotype 2 or 3. It is important to know that not everyone will need treatment. The decision to treat hepatitis C is complex and is best made by a physician experienced in treating the disease.
Read Also: How Does A Person Contract Hepatitis
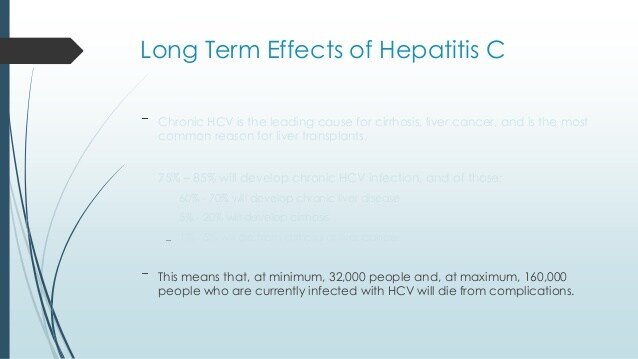
Effective Treatments Are Available For Hepatitis C
New medication to treat for HCV have been approved in recent years. These treatments are much better than the previously available treatment because they have few side effects and do not need to be injected. There are several direct-acting antiviral HCV treatments that cure more than 95% of people who take them in 8 to 12 weeks. HCV treatment dramatically reduces deaths among people with HCV infection, and people who are cured of HCV are much less likely to develop cirrhosis or liver cancer.
Take Action! CDCs National Prevention Information Network Service Locator helps consumers locate hepatitis B and hepatitis C prevention, care, and treatment services.
Who Is At Risk
While anyone who has not been vaccinated is, in theory, at risk of contracting hepatitis A, the World Health Organization cites the following groups at being of the highest risk:
Also Check: Hepatitis C Blood Test Results
Quebec Projects And Organizations
Footnote *Fighting against HIV and HCV in Quebec:
This project aims to improve the knowledge and skills of priority populations-gay and bisexual men, people who inject drugs, people living with HIV-and people who may interact with people living with HIV in the course of their work. To do this, the project will offer training workshops and information sessions on prevention to people from priority populations and people who may interact with people living with HIV in their work.
Mouve:
This project will promote the adoption of safer sexual behaviours and reduce stigma among at-risk youth from Montreal’s Caribbean and sub-Saharan African communities by increasing their knowledge about the transmission of sexually transmitted and blood-borne infections and building their capacity to manage their sexual health. To do this, the project will offer workshops that are culturally adapted to the realities and needs of young people. In addition, it will facilitate access to testing services for participants. Awareness-raising kiosks will be organized during festivals and neighbourhood festivals.
ETIAM:
This Community Alliance will offer workshops, organize symposia and disseminate reliable information to increase the knowledge and skills of community workers, professionals working in prisons and people from priority populations . A trans-inclusive approach will be adopted by alliance members and the participation of people with lived experience will be sought.
New Brunswick Projects And Organizations
New Brunswick STBBI Community Alliance:
This Community Alliance will work with community-based partner organizations, public health and healthcare professionals to identify and reduce barriers to accessing prevention, testing and treatment services for HIV, hepatitis C and sexually transmitted and blood-borne infections for people who use drugs. Activities will include implementing pilot projects to facilitate access to STBBI testing and integrating an expanded range of HIV prevention options into existing programs. In addition, healthcare providers and people who use drugs will receive training to overcome access barriers to HIV/HCV/STBBI prevention, testing and treatment services.
Education for Prevention & Support in Correctional settings:
This project will reach incarcerated men, women and youth through education sessions and the development of individualized pre-release plans. These activities will be supported by peer education mentors and will lead to increased knowledge of sexually transmitted and blood-borne infections , the adoption of safer sex and drug-using behaviours in correctional settings and on release, and greater access to STBBI and health services in community.
Don’t Miss: What Happens If You Have Hepatitis
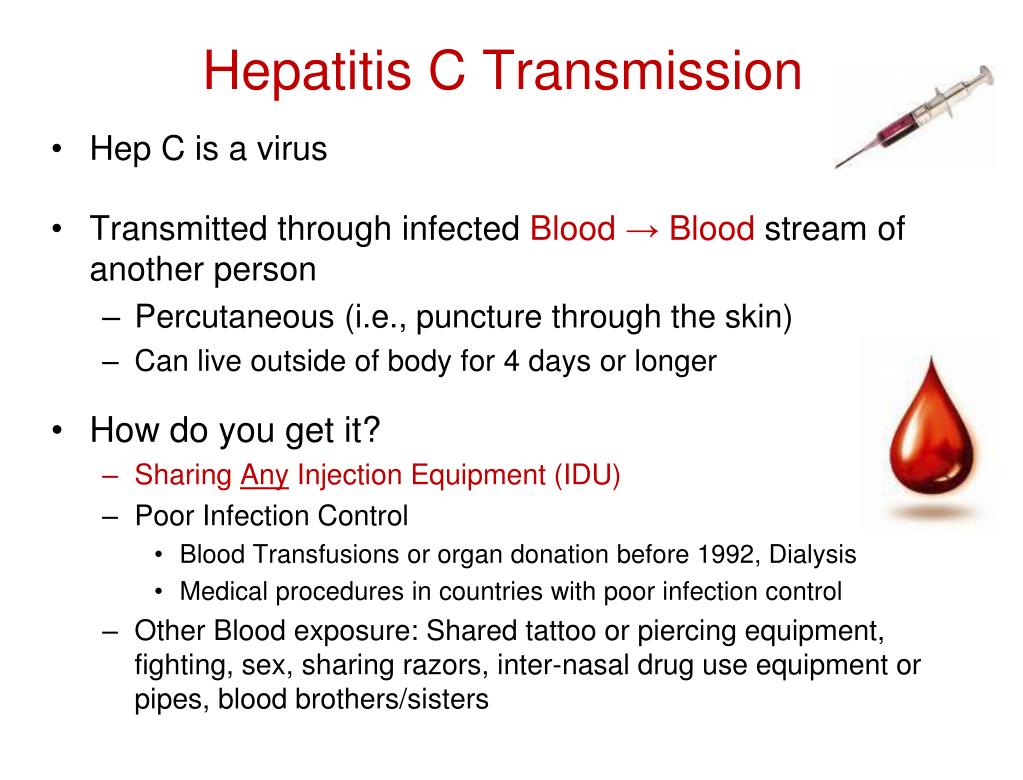
Contaminated Needles And Infected Blood
You can get hepatitis C from sharing contaminated needles, syringes and other injecting equipment during recreational drug use. Banknotes and straws used for snorting may also pass the virus on.
Being exposed to unsterilised tattoo and body piercing equipment can also pass hepatitis C on. Occasionally, you can get it from sharing a towel, razor blades or a toothbrush if there is infected blood on them.
Hepatitis C infection is also passed on in healthcare settings, from needle stick injuries or from medical and dental equipment that has not been properly sterilised. In countries where blood products are not routinely screened, you can also get hepatitis C by receiving a transfusion of unscreened blood and blood products.
You can prevent hepatitis C by:
- never sharing needles and syringes or other items that may be contaminated with infected blood
- only having tattoos, body piercings or acupuncture in a professional setting, where new, sterile needles are used
- following the standard infection control precautions, if youre working in a healthcare setting.
For Safer Sex Treat Hepatitis C
If you have chronic hepatitis C, of the best strategies for preventing transmission of the virus is to get medical treatment. More than 90 percent cases of hepatitis C can be cured within 8 to 12 weeks of treatment, according to the CDC. Newer hepatitis C treatments are not only effective but generally have fewer and much less severe side effects than previous drugs.
Just be aware that during treatment, transmission can still occur. And a cure doesnt grant you protection against the virus for life. If you continue to engage in high-risk behavior, you can get re-infected, warns Kenneth Sherman, MD, PhD, a professor of medicine and the director of the division of digestive diseases at UC Health in Cincinnati, Ohio.
Also Check: Side Effects Of Hepatitis C
Testing And When To Get Tested
Hepatitis C is tested through a blood test. At the HSHC, we offer non-nominal Hepatitis B, Hepatitis C and syphilis testing. You can do this at the same time as an anonymous HIV/AIDS test. With this test, your health card and personal information are required. These STBBIs are considered reportable to the Nova Scotia Health Authority, which means they track infection rates and follow up and will inform previous partners if they are at risk of infection. However, your blood is drawn and sent to the lab under a code which is known only by the nurse. When the test results are back from the lab, they are transferred to your electronic chart.
The difference between non-nominal and anonymous testing can be confusing! Please feel free to ask us any questions you may have about the testing process.
Why Is It Important
This measure reports on the sexually transmitted infections : chlamydia gonorrhoea non-congenital syphilis and also the blood-borne viruses: hepatitis B and C and human immunodeficiency virus . This measure no longer captures data on acquired immunodeficiency syndrome as it was removed from the National Notifiable Disease List in 2016.
If left untreated, STIs can have serious long-term health consequences, such as pelvic inflammatory disease, infertility, adverse pregnancy outcomes, miscarriage, and neonatal infections. Untreated syphilis can cause heart and brain damage . Chlamydia, gonorrhoea, and syphilis are treatable but cases are often asymptomatic for long periods . There is also evidence that these STIs can enhance transmission of HIV . Aboriginal and Torres Strait Islander people currently experience a relatively high number of notifications for bacterial STIs, relative to their representation in the total population. Although rates of HIV are not particularly high, Indigenous Australians are possibly more susceptible due to the high rates of STIs .
Recommended Reading: Chronic Hepatitis C Without Hepatic Coma
Nunavut Project And Organization
Culturally-Responsive Arts- and Social Media-Based Interventions to Promote Positive Sexual Health, Attitudes and Behaviours among Nunavut Youth:
This project aims to improve knowledge, attitudes and behaviours towards sexual health, sexuality and relationships, and to increase social media and internet safety among 12 to 25 year-old youth in Nunavut. This will be accomplished through Inuit knowledge-sharing and teaching techniques, including arts-based workshops for youth and a resource to support parent-adolescent conversations about sexual health and relationships. The initiative will also involve a youth-driven Photovoice project, which is an arts-based research method that allows the photographer to be the researcher.
For more information about the funding of these organizations please visit PHAC’s Proactive Disclosure page.
The Community Action Fund also provides support through Northern Wellness Agreements with:
- Government of Northwest Territories
Epidemiology Of Sexually Transmitted Hcv
2.1.1. Trends in HCV infections in HIVpositive and negative MSM
2.1.2. Molecular epidemiology
Molecular epidemiology is increasingly used to identify clusters and transmission pathways in rapidly evolving pathogens such as HIV and HCV. The main aim of these molecular approaches was to aid the public health response by identifying factors of the epidemic, such as hotspots or emerging clusters, otherwise missed.
2.1.3. Risk factors for acquiring sexually transmitted HCV
Finally, studies consistently show that biological factors might play a role: confection with STI, HIV1 infection in itself, a lower CD4 cell count and higher HIV RNA levels are associated with an increased risk of incident HCV infection , , , . These factors might affect the mucosal microenvironment and activate specific immune cells within mucosal tissues, which would allow HCV entry and retention.
You May Like: How Long Is Hepatitis C Treatment
British Columbia Projects And Organizations
Engage: Educate: Connect – Vancouver Island HIV/Hepatitis C/STI Peer Education Project:
This project will reduce the transmission of HIV, hepatitis C and other sexually transmitted and blood-borne infections by providing training to members of priority populations and their service providers. To achieve this, peer leaders from priority populations will be trained to deliver STBBI education to their peers, while service providers will be trained to deliver stigma-free health services.
PAN Provincial Capacity and Skills Building Project:
This project will offer training events, educational forums and webinars to community-based staff, public health and healthcare professionals, people living with HIV or hepatitis C , and policymakers. These skills-building opportunities will increase the capacity of participants to develop policies, programs and interventions that address the prevention and care needs of people living with and at risk of HIV/HCV, including in Indigenous communities.
Real Talk:HIV and Viral Hepatitis Interventions Among British Columbia’s At-Risk Immigrants and Refugees Through Alignment between Social Services and Provincial Care:Peers Educating and Empowering to Reduce Stigma Project:A Targeted Northern BC HIV/AIDS, HCV and STBBI Strategy:Sex Workers’ Rights are Human Rights: Community-Based HIV and Hepatitis C Interventions for Prevention, Increased Care Access and Stigma Reduction:
At What Stage Did The Evidence Emerge Around Sexual Transmission
This cluster of hepatitis C cases that occurred in mostly HIV-positive men who have sex with men was first reported in Europe. Then similar cases were reported in Australia and the United States, between 2004 and 2006. The co-associated factors were high-risk sex, chem sex and STIs . That cast a whole new light on how exactly its spread.
You May Like: Can You Die From Hepatitis C
Safer Sex Screening Treatment
Drs. Nelson and Bhagani both believe that people with HIV can best protect themselves from acquiring HCV sexually by continuing to practice protected anal intercourse, rimming and fisting. “Like everything, you’re better off not getting it, and since there is no vaccine available, taking precautions is the only way,” says Dr. Nelson.
They also strongly suggest that yearly screening for HCV should become the norm in all U.K. HIV clinics. “The first thing we really need to know in this country is what is the true prevalence of HCV in the HIV population,” continues Dr. Nelson. “It is clearly something that people who have got HIV have put themselves at risk of. We need to make sure that everyone is screened for HCV. The advantage of picking it up early means you are much more likely to eradicate it.”
Hepatitis C Was Not Originally Believed To Be Sexually Transmissible Why Did That Belief Change
In monogamous heterosexual couples where one partner is HCV-positive and the other not, the transmission rates are very low. However, around 2004 a new epidemic of hep C within the male gay community around the world occurred. Studies into sexual practices showed that one of the risk factors was chem sex.
So, we came to understand that its the type of sex that is key. The more robust the sex, the more likely that HCV is to be transmitted.
Read Also: Can You Catch Hepatitis C
What Are The Chances Of Getting Hep C Sexually
Hepatitis C spreads by contact with an infected persons blood. Although uncommon, hepatitis C can be transmitted through sexual activity, if the person has genital sores and cuts. It can also be transmitted during menstruation. However, just 2% of hepatitis C cases are sexually transmitted.
The risk of getting hepatitis C sexually increases in the following situations:
- Men who have sex with men
How Is The Virus Spread
Like hepatitis B virus, hepatitis C virus is spread when blood of an infected person enters the body of a person who is not infected, such as through sharing needles or “works” when shooting drugs or occupational needle stick injury. The risk of sexual transmission has not been thoroughly studied but appears to be low in long-term, monogamous relationships. There is no evidence that the hepatitis C virus can be transmitted by casual contact such as hugging or shaking hands, through foods, by sharing eating utensils or drinking glasses, or by coughing or sneezing. Hepatitis C is not spread by breastmilk.
Also Check: How To Read Hepatitis B Test Results
How Common Is Sexual Transmission Of Hepatitis C
Sexual transmission of hepatitis C is not as common as hepatitis B. But theres undoubtedly a possibility, and you can get infected after having sexual intercourse with an infected individual. There have been sexually-transmitted outbreaks of hepatitis C, especially in HIV-positive patients and other immunocompromised individuals. In this group, the chance of getting hepatitis C through sexual activity is increasing.
In the past, 0.07 people per 100 were infected through sexual transmission . But since 2014, the increase is dramatic: 1.8 people per 100 . This is perhaps because the virus is mutating and making sexual transmission more common. Our current diagnostic measures are better than before, and the transmission rate was actually higher than we thought.
Some patients think that after getting infected with hepatitis C, they cannot be infected again. But thats not the case, and reinfection due to sexual transmission is even higher than primary infection. In other words, people who were infected with hepatitis have an even higher chance of getting infected once again after sexual intercourse with an infected individual. According to studies, 7.3 out of 100 people can be reinfected with the disease.
Newfoundland/labrador Projects And Organizations
Social Health Information Exchange Labrador District :
This project will offer annual arts-based leadership summits for Indigenous youth in Labrador communities, in order to improve their leadership skills, self-worth, holistic well-being and knowledge and uptake of effective ways to prevent HIV, hepatitis C and sexually transmitted and blood-borne infections . Using ACT , Peer Leadership Teams will support, empower and educate youth on sexual health, STBBI, healthy relationships and positive life skills through skills sharing opportunities at regional events and in participants’ home communities. An arts-based, culturally-relevant and multi-language website will provide resources and information to increase access to holistic health and social services for Labradorians .
Getting to Zero:
This project will increase knowledge of effective prevention interventions for HIV, hepatitis C and other sexually transmitted and blood-borne infections through training, a youth-focussed educational app and a social media campaign. The training will be offered to front-line professionals working with target populations-lesbian, gay, bisexual, transgender and queer youth, gay men, seniors, people who use drugs, people living in correctional facilities. The educational app will reach youth between the ages of 16-29 from across the province. The social media campaign will reach people living with HIV and/or hepatitis C.
Recommended Reading: Home Remedies For Hepatitis C In Urdu