Is There Treatment For Alcoholic Liver Disease
People that develop any stage of alcoholic liver disease need to focus on removing alcohol from their life. Early stages of ALD can be reversed if a person stops drinking.
Cognitive behavioral therapy can also help a person with alcohol dependence. Inpatient rehabilitation facilities may also help a person with severe alcohol dependency.
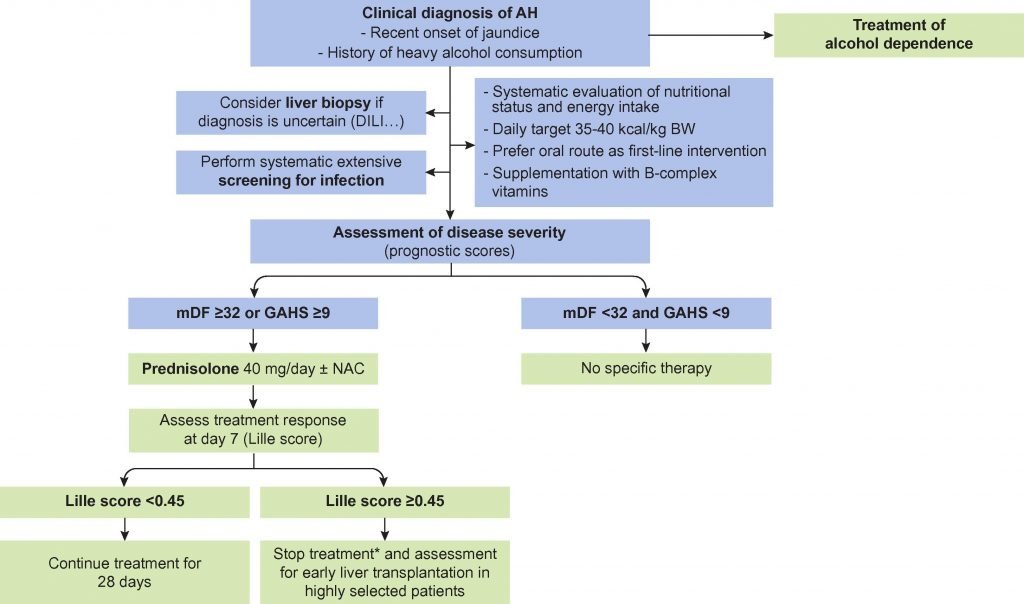
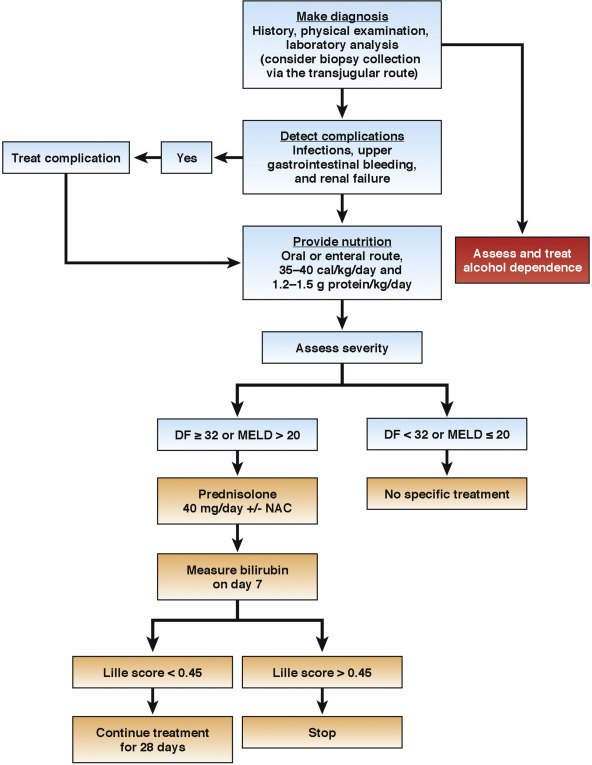
Individuals diagnosed with acute alcoholic hepatitis may be given corticosteroids or pentoxifylline to reduce the inflammation of the liver while receiving treatment in a hospital.
In the advanced stages of alcoholic liver disease, a person may develop liver failure. If this happens, a liver transplant is the only option for survival. People must demonstrate sobriety by going at least six months of abstaining from alcohol to be considered for a liver transplantation.
The best way for a person to reduce the risks of alcoholic liver disease is to monitor their alcohol intake and get help for alcohol abuse. People with any stage of alcoholic liver disease need to stop drinking completely to increase their chance of slowing or possibly reversing the disease.
Acute Vs Chronic Alcoholic Hepatitis
Hepatitis caused by alcohol consumption is usually an acute or short-term condition. Lifestyle changes, such as reduced alcohol consumption, may be the only treatment for acute cases of alcoholic hepatitis. Medications may be prescribed for severe cases.
When people return to heavy drinking after recovering from acute alcoholic hepatitis, they increase their risk of developing chronic alcoholic hepatitis. Chronic alcoholic hepatitis is reoccurring liver inflammation that can lead to cirrhosis, or scarring, of the liver.
Cessation Of Alcohol Intake
Cessation of alcohol use is the mainstay of treatment of alcoholic hepatitis. The 2010 American Association for the Study of Liver Diseases alcoholic liver disease guideline states that complete abstinence should be enjoined on all alcoholic hepatitis patients.
In general, alcoholic hepatitis resolves or improves greatly following 6-12 months of alcohol abstinence, and continued improvement may be observed for several years. Mild alcoholic hepatitis often resolves completely, but, following severe alcoholic hepatitis, residual cirrhosis can usually be demonstrated. If alcohol abuse persists, alcoholic hepatitis invariably persists and progresses to cirrhosis, and the prognosis is dramatically worse.
Some experts have questioned whether complete abstinence is necessary or whether reduced amounts of alcohol would be sufficient for recovery in most patients. Given the addictive nature of alcohol in most patients who use it heavily, counseling complete abstinence is prudent. Patients should be referred to a program of rehabilitation and support, and they should be strongly encouraged to attend. Also, patients should be fully informed regarding the serious potential health consequences of continued ethanol use.
Recommended Reading: Can You Catch Hepatitis C From Having Sex
Rationale For Current Therapy For Severe Ah And Results Of Randomized Controlled Trials For Treatment Of Severe Ah
More than 20 RCTs of glucocorticoids have been conducted in patients with severe AH defined by an MDF > 32 . Several of these studies were used to create the current guidelines of the AASLD and EASL . The 1989 U.S. multicenter trial of methylprednisolone vs. placebo for treating severe AH reported that the 28-day mortality rate was significantly lower in those patients treated with methylprednisolone compared with BSC . A subsequent trial from France reported similar findings . Although some trials failed to show significant survival benefit in subjects treated with glucocorticoids, 2 separate meta-analyses that included primarily high-quality studies concluded that there is a benefit to treatment , whereas a third did not . A 2008 Cochrane systematic review of 15 trials concluded that there was no benefit from glucocorticoids, except possibly in the group with an MDF > 32, primarily due to substantial variability in bias . Those trials with low bias showed benefit, whereas trials with high bias showed no benefit.
PTX was reported to reduce mortality in patients with severe AH . Subsequent larger trials reached similar conclusions . Most of the reduction in mortality appeared to be related to a decrease in the frequency of hepatorenal syndrome in the survivors . However, 2 meta-analyses of all trials concluded that there were no differences in short-term mortality related to PTX . Subsequent studies combining PTX with glucocorticoids did not show any additive benefit .
Symptoms & Causes Of Alcoholic Hepatitis
Some cases of acute alcoholic hepatitis may not cause symptoms, and people who are developing alcoholic hepatitis may not know until it becomes more advanced. These symptoms may include:
- Confusion, due to the buildup of the toxin ammonia
- Swelling in the abdomen caused when the liver does not make enough of a protein called albumin
- Bleeding that may be severe because the liver does not produce enough of the proteins needed for blood clotting
- Bleeding in the throat caused by weakened blood vessels that occur with hepatitis
- Yellowing of the skin and whites of the eyes, also called jaundice, occurs when the liver cannot break down a substance called bilirubin. The jaundice alcoholic hepatitis causes is not dangerous in and of itself. However, it indicates that other dangerous liver conditions are likely present. People who experience jaundice should seek immediate medical care.
Scientists are not entirely certain what it is about alcohol that causes alcoholic hepatitis. However, heavy alcohol use plays an important role. Without alcohol use, there is virtually no risk at all for developing alcoholic hepatitis. When alcohol use is stopped, the inflammation from alcoholic hepatitis may eventually go away completely.
Several other risk factors may, when combined with alcohol misuse, make the risk of developing alcoholic hepatitis greater. These risk factors include:
- Poor nutrition
- Obesity
Recommended Reading: Can I Get Rid Of Hepatitis C
How Can Prevent Alcoholic Hepatitis
The best treatment is to stop drinking.
Treatment also may include:
- Hereditary defects in iron or copper metabolism
- Prolonged exposure to toxins
In children, the most frequent causes are biliary atresia â a disease that damages the bile ducts â and neonatal hepatitis. Children with these diseases often receive liver transplants.
Many adult patients who require liver transplants suffer from primary biliary cirrhosis. We do not yet know what causes this illness, but it is not in any way related to alcohol consumption.
How Long Does It Take For Alcoholic Hepatitis To Turn Into Cirrhosis
About 10 to 20 percent of heavy drinkers usually develop cirrhosis after 10 or more years. Generally, drinking 80 grams of ethanol daily for 10 to 20 years is required to develop cirrhosis which corresponds to approximately one liter of wine, eight standard sized beers, or one half pint of hard liquor each day.
You May Like: Hepatitis C Symptoms In Females
Treatment Options For Alcoholic Hepatitis
Alcohol use both causes and worsens alcoholic hepatitis, so a diagnosis of alcoholic hepatitis means you may want to consider stopping drinking gradually. Quitting drinking can help reduce symptoms and prevent further damage to your liver.
In the early stages of the condition, avoiding alcohol may even help reverse liver damage. Once more significant damage has occurred, the changes to your liver may become permanent.
Even if the damage is too severe to reverse, quitting drinking could prevent further harm to your liver.
- According to
Alcoholic hepatitis can lead to severe and lasting liver damage, which can, in turn, cause serious health complications. In some cases, these complications can be life threatening.
How Is It Diagnosed
- Medical history. Your doctor may ask about your medical past to see if thereâs reason to believe you may have alcohol-related liver problems.
- Questionnaire. Theyâll ask you questions to determine if your drinking has become a problem.
- Blood tests. These will check your liver enzymes. Abnormally high levels are a sign of liver damage.
- Liver biopsy. Your doctor may request one in addition to blood tests.
You May Like: Is Hepatitis C An Std
Treating Alcoholic Liver Disease
The most important part of treating alcoholic liver disease is to permanently stop all alcohol consumption. Your health care team can help you find programs to support you on this critical undertaking, including both inpatient and outpatient treatment programs at UChicago Medicine. Additionally, treatment for alcoholic liver disease may involve:
- Taking medications to prevent your craving for alcohol
- Eating healthy, well-balanced meals
How Do You Repair Liver Damage From Alcohol
There are several things you can do to help reverse the effects of alcohol on your liver, such as:
Also Check: What Is Hepatitis C Caused By
Who Is At Risk For Alcoholic Hepatitis
Both women and men can have alcoholic hepatitis. Most people who are diagnosed with alcoholic hepatitis are between 40 and 60 years old. Patients at highest risk for alcoholic hepatitis typically drink more than 100 grams of alcohol a day for many years. Those who have a family history of alcoholism may also be at risk for the disease.
Liver Disease & Pancreatitis
Along with looking at the impact of alcohol on the liver, its also relevant to consider how alcoholism causes pancreatitis. There is acute pancreatitis and chronic pancreatitis.
The pancreas is a gland behind the stomach responsible for releasing digestive enzymes and works with the liver to process substances. An inflamed pancreas is called pancreatitis.
Acute pancreatitis is sudden onset inflammation thats short-lived. The results of the condition range significantly, from being mildly uncomfortable to fatal, but most people recover. Chronic pancreatitis has symptoms similar to acute, but theres frequent pain, weight loss and the potential for diabetes to develop.
In the majority of cases, alcohol causes acute pancreatitis, although other causes may include trauma, metabolic conditions or infections. Heavy, long-time alcohol use accounts for about 60-90% of chronic pancreatitis cases.
Having chronic pancreatitis puts you at risk for other serious illnesses, including cancer and diabetes. Stopping alcohol use significantly increases your chances of recovering from pancreatitis.
Read Also: Interpretation Of Hepatitis A Serologic Test Results
Nutrition Services And Gastroenterology/hepatology
Adequate nutritional support is of paramount importance for the survival and recovery of patients with alcoholic hepatitis. The complexity of the disease and the wide variation in nutritional regimens and modalities mandate consultation with a nutritionist. Customarily, the gastroenterology service of the hospital should be able to handle this issue and should be instrumental in treatment.
In patients with alcoholic hepatitis who have developed cirrhosis, especially those with coexistent chronic viral hepatitis B or C, consider periodic surveillance for hepatocellular carcinoma. A common algorithm includes the determination of serum alpha-fetoprotein levels at 6-month intervals along with annual diagnostic ultrasonography. The finding of a liver nodule or an elevated AFP level should lead to referral to a liver specialist and additional diagnostic studies.
In general, for patients with severe alcoholic hepatitis or cirrhosis, observation by a gastroenterologist or a hepatologist is desirable, particularly if the illness is of sufficient severity or complexity to require intensive care.
Protein Restriction Vs Normal Protein Intake
Except in patients with severe encephalopathy, protein restriction is unnecessary and should be avoided because a protein-deficient diet impairs liver regeneration and worsens liver function. Even in the presence of hepatic encephalopathy, patients are usually able to ingest a minimum of 60-100 g/d of dietary protein if other measures to control encephalopathy have been aggressively pursued. In rare instances, restricting dietary proteins may be necessary. In these cases, alternatives include provision of high-quality protein via the parenteral route or provision of oral amino acid supplements that are selectively enriched with branched-chain amino acids.
Read Also: Does Hepatitis C Have Symptoms
What Is Alcoholic Hepatitis
Itâs a serious condition that affects people who are, or used to be, heavy drinkers. It can cause short- or long-term liver damage.
The liver is the largest organ in the body, and it removes poisons such as alcohol from the blood. When itâs damaged by decades of heavy drinking, it can become inflamed, scarred, and fatty. Over time, it stops working right. Up to 35% of long-time heavy drinkers develop alcoholic hepatitis.
If you have it, you might wake up and notice that your skin or the whites of your eyes look yellow — a condition called jaundice. You might also have a fever, stomachache, or liquid buildup in your belly, and you may lose weight. If youâve been diagnosed with it or think you might have it, hereâs what you need to know. Learn more about health problems caused by alcohol.
Treatment Options For Alcoholism
Severe alcoholism is a disease, and often needs the assistance of addiction treatment specialists. Seeking treatment for an alcohol use disorder while attempting to manage medical issues can be overwhelming.
Treating addiction and alcoholic liver disease at the same time is an option that will help your recovery to be as successful as possible. Please reach out to our qualified and helpful staff so we can help explore substance abuse treatment options with you.
Written by the Addiction Resource Editorial Staff
Addiction Resource aims to provide only the most current, accurate information in regards to addiction and addiction treatment, which means we only reference the most credible sources available.
These include peer-reviewed journals, government entities and academic institutions, and leaders in addiction healthcare and advocacy. Learn more about how we safeguard our content by viewing our editorial policy.
- American Association for the Study of Liver DiseasesPrediction of histologic alcoholic hepatitis based on clinical presentation limits the need for liver biopsy
Read Also: Hepatitis B Can It Be Cured
Is Alcoholic Hepatitis The Same As Cirrhosis
Alcoholic cirrhosis is an advanced stage of alcoholic liver disease, and is irreversible. Cirrhosis results when sustained inflammation destroys healthy, functioning liver cells which are replaced by scar tissue.
Taking remedial steps for alcoholic hepatitis can help regain significant liver function, but liver damage from cirrhosis is permanent and often leads to liver failure.
Definition Of Alcoholic Hepatitis
Histologic features of AH include steatosis and ballooning degeneration of hepatocytes , intrahepatic cholestasis , chicken-wire fibrosis, Mallory-Denk bodies, and megamitochondria. Cirrhosis is present in the vast majority of those who are severely ill.
A recent consensus statement from the Alcoholic Hepatitis Consortium sponsored by the National Institute of Alcohol Abuse and Alcoholism provided a working definition of AH that includes onset of jaundice within 60 days of heavy consumption of alcohol for a minimum of 6 months, a serum bilirubin > 3 mg/dL, an elevated AST , an AST:ALT ratio > 1.5, and no other obvious cause for hepatitis . The consensus statement proposed classifying patients with AH as definite when a liver biopsy was used to establish the diagnosis probable when the clinical and laboratory features were present without potential confounding problems and possible when confounding problems were present. This proposed classification is intended to improve interpretation of future treatment trials in patients with AH, since prior studies indicated that 10-15% of subjects diagnosed with acute AH based on clinical criteria alone did not have characteristic histologic features on a liver biopsy specimen.
You May Like: How Long Do You Live With Hepatitis C
Signs & Symptoms Of Afld
Unfortunately, AFLD itself has very few symptoms. The main AFLD symptoms include:
- Feeling tired
- Having discomfort in your upper right abdomen
- Yellow coloration of the skin or whites of the eyes
Because there are so few symptoms, it can be hard for doctors to make a diagnosis for AFLD in the early stages. The disease is often found if you need to have imaging done, or if you have a blood test that comes back showing problems with the chemicals in your liver. Sometimes, doctors are not able to find alcoholic fatty liver disease until it progresses into a more dangerous condition like cirrhosis.
From Steatosis To Cirrhosis

Alcoholic Liver Disease includes three conditions: Fatty liver, alcoholic hepatitis, and cirrhosis. Heavy drinking for as little as a few days can lead to “fatty” liver, or steatosis-the earliest stage of alcoholic liver disease and the most common alcohol-induced liver disorder.
Steatosis is marked by an excessive buildup of fat inside liver cells. This condition can be reversed, however, when drinking stops.
Drinking heavily for longer periods may lead to a more severe, and potentially fatal condition, alcoholic hepatitis-an inflammation of the liver. Symptoms include nausea, lack of appetite, vomiting, fever, abdominal pain and tenderness, jaundice, and, sometimes, mental confusion. Scientists believe that if drinking continues, in some patients this inflammation eventually leads to alcoholic cirrhosis, in which healthy liver cells are replaced by scar tissue , leaving the liver unable to perform its vital functions.
The presence of alcoholic hepatitis is a red flag that cirrhosis may soon follow: Up to 70 percent of all alcoholic hepatitis patients eventually may go on to develop cirrhosis. Patients with alcoholic hepatitis who stop drinking may have a complete recovery from liver disease, or they still may develop cirrhosis.
You May Like: What Is Hepatitis B Shot For